Case Report
VOLUME: 39 | ISSUE: 2 | Jun 25, 2023 | PAGE: (50 - 53) | DOI: 10.24911/BioMedica/5-1025
Mucinous Cystadenoma of Parotid Gland: A Rare Entity
Authors: Umber Irshad Butt , Gulfishan Zameer , Aatiqa Rana , Sameer Anjum
Article Info
Authors
Umber Irshad Butt
Lecturer, Department of Histopathology, University of Health Sciences Lahore, Pakistan.
Gulfishan Zameer
M. Phil Sch, MLS (Cytotechnology), Department of Histopathology, University of Health Sciences Lahore, Pakistan.
Aatiqa Rana
M. Phil Sch, MLS (Histotechnology), Department of Histopathology, University of Health Sciences Lahore, Pakistan.
Sameer Anjum
Laboratory Technologist, Department of Histopathology, University of Health Sciences Lahore, Pakistan.
Publication History
Received: April 25, 2023
Revised: May 16, 2023
Accepted: June 08, 2023
Published: June 25, 2023
Abstract
Cystadenoma is a benign salivary gland tumor that develops very infrequently. The commonest site for their occurrence is minor salivary glands, where these present as cystic growths with papillary projections. Cystadenomas are often interpreted as mucous retention cysts. Therefore, histopathological confirmation is essential for further treatment and follow-up of the patients, even after the surgery, to keep a check on the recurrence and, in the long run, the exclusion of the possibility of malignant transformation. We report a case of mucinous cystadenoma of the salivary gland occurring in a 44-year-old male who presented with a painless mass, gradually increasing in size over the period of 3 years. The radiological evaluation reported it as a retention cyst. Fine needle aspiration cytology was performed, followed by complete surgical excision of the lesion. Diagnosis of mucinous cystadenoma in the parotid gland was made. There are only a few cases of mucinous cystadenoma of the parotid gland reported so far from the world, and to the best of author’s knowledge, it is the first case of its kind reported from Pakistan.
Keywords: Mucinous cystadenoma, parotid gland, diagnosis, fine needle aspiration cytology, histopathology.
Pubmed Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum. Mucinous Cystadenoma of Parotid Gland: A Rare Entity. BioMedica. 2023; 25 (June 2023): 50-53. doi:10.24911/BioMedica/5-1025
Web Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum. Mucinous Cystadenoma of Parotid Gland: A Rare Entity. https://biomedicapk.com/articles/online_first/1025 [Access: July 27, 2024]. doi:10.24911/BioMedica/5-1025
AMA (American Medical Association) Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum. Mucinous Cystadenoma of Parotid Gland: A Rare Entity. BioMedica. 2023; 25 (June 2023): 50-53. doi:10.24911/BioMedica/5-1025
Vancouver/ICMJE Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum. Mucinous Cystadenoma of Parotid Gland: A Rare Entity. BioMedica. (2023), [cited July 27, 2024]; 25 (June 2023): 50-53. doi:10.24911/BioMedica/5-1025
Harvard Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum (2023) Mucinous Cystadenoma of Parotid Gland: A Rare Entity. BioMedica, 25 (June 2023): 50-53. doi:10.24911/BioMedica/5-1025
Chicago Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum. "Mucinous Cystadenoma of Parotid Gland: A Rare Entity." 25 (2023), 50-53. doi:10.24911/BioMedica/5-1025
MLA (The Modern Language Association) Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum. "Mucinous Cystadenoma of Parotid Gland: A Rare Entity." 25.June 2023 (2023), 50-53. Print. doi:10.24911/BioMedica/5-1025
APA (American Psychological Association) Style
Umber Irshad Butt, Gulfishan Zameer, Aatiqa Rana, Sameer Anjum (2023) Mucinous Cystadenoma of Parotid Gland: A Rare Entity. , 25 (June 2023), 50-53. doi:10.24911/BioMedica/5-1025
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 39(2):50-53
CASE REPORT
Mucinous cystadenoma of parotid gland: a rare entity
Umber Irshad Butt1*, Gulfishan Zameer2, Aatiqa Rana3, Sameer Anjum4
Received: 25 April 2023 Revised date: 16 May 2023 Accepted: 08 June 2023
Correspondence to: Umber Irshad Butt
*Lecturer, Department of Histopathology, University of Health Sciences Lahore, Pakistan.
Email: drumberbutt@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Cystadenoma is a benign salivary gland tumor that develops very infrequently. The commonest site for their occurrence is minor salivary glands, where these present as cystic growths with papillary projections. Cystadenomas are often interpreted as mucous retention cysts. Therefore, histopathological confirmation is essential for further treatment and follow-up of the patients, even after the surgery, to keep a check on the recurrence and, in the long run, the exclusion of the possibility of malignant transformation. We report a case of mucinous cystadenoma of the salivary gland occurring in a 44-year-old male who presented with a painless mass, gradually increasing in size over the period of 3 years. The radiological evaluation reported it as a retention cyst. Fine needle aspiration cytology was performed, followed by complete surgical excision of the lesion. Diagnosis of mucinous cystadenoma in the parotid gland was made. There are only a few cases of mucinous cystadenoma of the parotid gland reported so far from the world, and to the best of author’s knowledge, it is the first case of its kind reported from Pakistan.
Keywords:
Mucinous cystadenoma, parotid gland, diagnosis, fine needle aspiration cytology, histopathology.
Introduction
Cystadenoma of the salivary gland is a rare benign epithelial tumor, representing approximately 4.2%-4.7% of all benign salivary gland tumors. The most common sites include the parotid gland (58%), submandibular gland (6.6%), sublingual gland (0.5%), minor salivary glands in the lips (10.7%), and palate (7.1%). Clinically, cystadenomas typically appear as a painless, slow-growing mass in the major salivary glands and as a smooth-surfaced nodule within the oral mucosa, resembling a mucocele.1,2
Cystadenomas have two histopathological types identified as the papillary and the mucinous forms by the World Health Organization. Clinically these lesions cannot be easily differentiated from other benign tumors. Hence, the diagnosis is primarily based on characteristic histological findings. These salivary gland tumors are difficult to identify because of their diverse appearances.3 Mucinous cystadenoma is characterized by a cyst lined by tall columnar epithelium predominantly composed of mucous cells with restricted papillary growth. Papillary cystadenomas are rare, benign, slow-growing tumors composed of unilocular or multilocular cysts lined by cuboidal or columnar cells with intraluminal papillary projections.4,5 Moreover, papillary cystadenomas can have a malignant potential, as documented by some studies, but it depends upon the recurrence rates and complete or incomplete surgical removal of major salivary glands. However, malignant transformation has not been reported in minor salivary glands.5,6
Physical examination plays a vital role in making a diagnosis, as almost 80% of salivary gland malignancies occur in the parotid gland, and around 80% of them are benign. The first and foremost approach is to differentiate between benign (cysts, inflammatory conditions, and hyperplasia) and malignant tumors. If malignancy is suspected, a pathological diagnosis is required.6
Case Presentation
This is a case report of mucinous cystadenoma of the parotid gland. A 44-year-old male presented at the Otorhinolaryngology outdoor of a tertiary care hospital in Lahore, Pakistan, with a complaint of a painless swelling in the right peri-auricular area for the last 3 years. Initially, it was a small swelling which remained unnoticed by the patient. During the last 6 months, it gradually increased in size. Clinical examination revealed a well-defined, painless, round mass ranging in diameter from 5.0 to 3.5 cm, slightly compressible, and soft to firm in consistency.
After clinical examination, a provisional diagnosis of benign salivary gland tumor was made. In addition to Pleomorphic adenomas and Warthin tumors, Cyst adenomas possibility of malignant neoplasm were also considered as possible differential diagnoses. Further non-invasive investigations were advised, and the patient was sent for a scan of the peri-auricular area that showed a heterogenous solid mass at the angle of the right mandibular region below the pinna measuring 3.0 × 3.0 cm. The patient was then referred to the Histopathology Department of the University of Health Sciences, Lahore, for fine needle aspiration cytology (FNAC). The aspiration showed an adequate mucinous background against which a few clusters of columnar cells with basally placed nuclei, vacuolated cytoplasm, and inflammatory cells were seen. (Figure 1)
After the FNAC report, the patient was sent to the Surgery department of the hospital for excision of the lesion. Prior to the referral for surgery, routine baseline investigations were carried out, which were within the normal ranges.
A superficial right parotidectomy was performed. The specimen was put in 10% formalin and sent for histopathological examination. Gross examination revealed a single, encapsulated, and lobular mass of dark brown color measuring 5.5 × 4.0 × 3.5 cm in size. Serial slicing revealed a cystic cavity filled with pearly white mucoid material within the lumen (Figure 2).
The histopathological findings of the H & E stained slides revealed mainly a large cystic cavity containing mucoid material. The cyst was lined by low cuboidal to benign appearing mucin-secreting columnar epithelium with focal stratification but intact polarity. The adjacent areas showed smaller cystic cavities lined by fibrous connective tissue. Normal salivary gland tissue was also identified (Figure 3) at the periphery. A diagnosis of “Mucinous Cystadenoma” was made based on the above findings.

Figure 1. Cytomorphology of the mucinous cystadenoma: a cluster of epithelial cells (star-B & C) with scattered inflammatory cells (arrow) within the mucin pools (A & D).
Discussion
Cystic salivary gland lesions are not common and make up almost 8% of all salivary gland pathologies. The parotid gland is involved frequently; 45%-50% of cases of cystadenoma occur in the parotid gland, followed by the minor salivary glands of the lip and buccal mucosa. Cystadenomas usually present as painless masses that grow slowly.3 In the present case, the swelling also developed as a painless small mass over the period of 3 years at the peri-auricular area, finally reaching the size of 5.5 cm. It has been documented that females are more commonly affected than males, especially in advanced age (>50 years),7 but in the current case, the swelling developed in a male patient of 44 years old. Contrary results were obtained in a study performed by Perks et al.,8 who reported a case of cystadenoma (both mucinous and papillary components) in a 78-year-old male with a 3-month history of an asymptomatic palatal swelling.
Salivary gland tumors are considered challenging to diagnose and interpret due to their diverse presentation patterns. Patients presenting with mucinous cystadenoma often do not exhibit distinct clinical features, making it challenging to clinically distinguish them from the rest of the benign salivary gland neoplasms such as mucous retention or extravasation cysts, or low-grade minor salivary gland malignancies such as papillary cystic variant of acinic cell carcinoma, adenoid cystic carcinoma, and mucoepidermoid carcinoma.2 There are certain case reports that document the location of mucinous cystadenoma to be at the hard palate. A report from the Japanese population documented a slowly enlarging tumor, 10 mm in diameter, in the hard palate.9 Another case published by Girotra et al.7 reported a non-tender swelling on the right side of the hard palate of a female patient. Yet another case reported a 2-year history of a slow-growing tumor in the left parotid gland but without any obvious clinical symptoms.10 In the current study, the patient presented with a complaint of a painless, gradually enlarging swelling in the right peri-auricular area. Similar clinical features were observed by Rai et al.,2 who reported a case of mucinous cystadenoma in a 60-year-old female patient who presented with an asymptomatic, gradually increasing swelling in the right posterior palatal area. Moreover, in another study bilateral buccal mucinous cystadenomas were diagnosed with no recurrence on 6-month follow-up.1
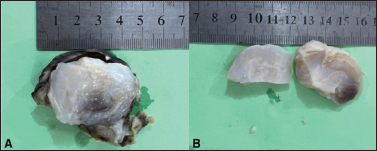
Figure 2. A capsular mass (arrow) with pearly white solidified mucoid material (A & B-star) within the cavity.
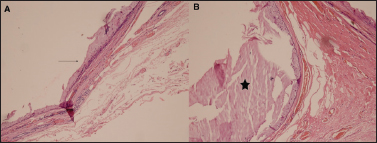
Figure 3. Photomicrograph on H&E staining (A)showing a cystic wall lined by mucinous epithelium (arrow) with adjacent normal parotid tissue. B: amorphous colloid material is seen within the cavity (star).
In the current study, the ultrasound scan of the patient showed a heterogenous solid mass of about 3.7 × 3.0 cm at the angle of the right mandibular region below the pinna. Ultrasound in routine clinical practice is non-invasive and can reveal certain characteristics of the lesion, but determining whether the lesion is benign or malignant seems challenging. The contrast-enhanced and multiparametric ultrasound, however, provides a more accurate image of the parotid tumor.11 In certain cases, preoperative imaging is not very helpful in diagnosing mucinous cystadenomas because they are mostly smaller in size with atypical features.1 In the current case, FNAC helped the pathologists reach a conclusion; however, a final diagnosis was made on the biopsy report. According to a study done by Naz et al.12 it has been documented that the diagnostic accuracy of FNAC for salivary gland swellings is 83.8%, with 70% positive predictive value and a specificity of almost 86.3%. Precise diagnosis and the critical role of surgical excision in the treatment cannot be emphasized, as the definitive diagnosis is established through a comprehensive histopathological examination.1
The swelling, in the current case, was excised after superficial right parotidectomy. Mostly, the superficial parotidectomy is opted for surgical removal of these parotid adenomas13 or a complete surgical excision of the tumor is undertaken depending upon its location.7
Literature has shown that some of the cystadenomas may have a malignant potential based on the recurrence rate and extent of surgical excision of major salivary glands.6 Surgical excision of the complete tumor with clear resection margins is advisable to avoid the transformation of a mucinous cystadenoma into a mucinous cystadenocarcinoma over the time period.1,5,14,15 One of the cases reported came up with an initial histopathological picture of mucinous cystadenoma with focal apocrine differentiation, but a prominent invasive micropapillary adenocarcinoma component along with a rim of lymphoid tissue surrounding the margins was observed. The morphology of the micropapillary adenocarcinoma component was similar to the invasive micropapillary carcinoma of the mammary gland.8 It has also been documented by Mariano et al.16 that papillary mucinous adenocarcinoma presented as a simple nodular, slow-growing, painless, benign cyst on the inner side of the left lower lip protruding deep to the buccal mucosa in a male patient. It had no clinical picture related to malignancy. But later, after the surgical excision, it turned out to be mucinous cystadenocarcinoma without distant metastasis, and the patient remained clinically stable in a follow-up period of 11 years and 6 months.
Conclusion
Mucinous cystadenomas of the salivary glands are rare tumors composed of cysts and glands lined by gastrointestinal or Müllerian type mucinous epithelium without any architectural complexity or cytologic atypia. These must be excised completely after histopathologic confirmation to prevent recurrence or malignant transformation. In addition, a consistent follow-up of the patient is extremely important, especially for all those surgeries with incomplete excision.
List of Abbreviations
| FNAC | Fine needle aspiration cytology |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The case is approved by the Institutional Ethical Review Committee of the University of Health Sciences Lahore, Pakistan, vide Letter No: UHS/REG-23/ERC/1456; dated: 22-03-2023.
Authors’ contributions
UIB: Conception and drafting of the manuscript; Important intellectual input.
GZ, AR, and SA: Acquisition and interpretation of data; Drafting of manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Umber Irshad Butt1, Gulfishan Zameer2, Aatiqa Rana3, Sameer Anjum4
- Lecturer, Department of Histopathology, University of Health Sciences Lahore, Pakistan
- M. Phil Scholar, Medical Laboratory Sciences (Cytotechnology), Department of Histopathology, University of Health Sciences Lahore, Pakistan
- M. Phil Scholar, Medical Laboratory Sciences (Histotechnology), Department of Histopathology, University of Health Sciences Lahore, Pakistan
- Laboratory Technologist, Department of Histopathology, University of Health Sciences Lahore, Pakistan
References
- Choi JH, Kim SH, Hwang JH, Kim KS, Lee SY. Multiple bilateral malar mucinous cystadenomas in the minor salivary glands. Arch Craniofac Surg. 2020;21(5):329–33. https://doi.org/10.7181/acfs.2020.00367
- Rai S, Rana A, Gupta V, Jain G, Prabhat M. Mucinous cystadenoma: a rare entity. Dent Res J. 2013;10(5):685–88.
- El-Naggar A, Chan J, Grandis JR, Takata T, Slootweg P. WHO classification of head and neck tumours International Agency for Research on Cancer (IARC). Geneva, Switzerland: World Health Organization (WHO); 2017.
- Wang L, Zhang SK, Ma Y, Ha PK, Wang ZM. Papillary cystadenoma of the parotid gland: a case report. World J Clin Cases. 2019;7(3):366–72. https://doi.org/10.12998/wjcc.v7.i3.366
- Tjioe KC, de Lima HG, Thompson LD, Lara VS, Damante JH, de Oliveira-Santos C. Papillary cystadenoma of minor salivary glands: report of 11 cases and review of the English literature. Head Neck Pathol. 2015;9:354–9. https://doi.org/10.1007/s12105-014-0602-0
- Guzzo M, Locati LD, Prott FJ, Gatta G, McGurk M, Licitra L. Major and minor salivary gland tumors. Crit Rev Oncol Hematol. 2010;74(2):134–48. https://doi.org/10.1016/j.critrevonc.2009.10.004
- Girotra C, Padhye MN, Mahajan P, Nair A. A rare case report of mucinous cystadenoma with immunohistochemical analysis and review of literature. J Maxillofac Oral Surg. 2015;14(Suppl 1):426–34. https://doi.org/10.1007/s12663-014-0656-2
- Perks A, Martin K, Domah F, Bates T, Anstey H. Cystadenoma of the palate: a rare site for a rare entity. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;132(1):e35. https://doi.org/10.1016/j.oooo.2021.03.130
- Tange K, Fukuta K, Yonezaki H, Nakayama A, Matsuura H, Maeda M. A case of mucinous cystadenoma arising in the palate. Japanese J Oral Maxillofac Surg. 2006;52(2):73–6.
- Michal M, Skálová A, Mukenšnabl P. Micropapillary carcinoma of the parotid gland arising in mucinous cystadenoma. Virchows Archiv. 2000;437:465–8.
- Gökçe E. Multiparametric magnetic resonance imaging for the diagnosis and differential diagnosis of parotid gland tumors. J Magn Reson Imaging. 2020;52(1):11–32. https://doi.org/ 10.1002/jmri.27061
- Naz S, Hashmi AA, Faridi N, Edhi MM, Kamal A, Khan M. Diagnostic role of fine needle aspiration cytology (FNAC) in the evaluation of salivary gland swelling: an institutional experience. BMC Res Notes. 2015;8(1):1–5. https://doi.org/ 10.1186/s13104-015-1048-5
- Alexiev BA, Jennings LJ, Samant S, Rao S. Oncocytic papillary cystadenoma with prominent mucinous differentiation of parotid gland: a case report. Pathol Res Pract. 2017;213(10):1310–4.
- O’Brien CJ. Current management of benign parotid tumors - the role of limited superficial parotidectomy. Head Neck J Sci Spec Head Neck. 2003;25(11):946–52. https://doi.org/10.1002/hed.10312
- Dutra S, Rito M, Vilares M, Borges A. Mucinous cystadenocarcinoma of the oral tongue: malignant transformation from a mucinous cystadenoma? BMJ Case Rep. 2020 Oct 30;13(10):e235932. doi: 10.1136/bcr-2020-235932
- Mariano RC, Oliveira MR, Silva ADC, Mariano LDCF, Vargas PA, Almeida OPD. Papillary mucinous cystadenocarcinoma: rare malignant tumor in minor salivary gland. Rev Gaúch Odontol. 2016;64(2):207–11. https://doi.org/10.1590/1981-863720160002000133117
