Original Article
VOLUME: 38 | ISSUE: 4 | Dec 30, 2022 | PAGE: (209 - 213) | DOI: 10.24911/BioMedica/5-772
Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan
Authors: Rabia Nafees , Humaira Zareen , Zoofishan Imran , Dr Maujid Masood Malik , Assistant Professor Shazia Jang Sher
Article Info
Authors
Rabia Nafees
Department of Obstetrics & Gynaecology, Post Graduate Medical Institute, Lahore General Hospital, Lahore, Pakistan.
Humaira Zareen
Department of Obstetrics & Gynecology, College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
Zoofishan Imran
Department of Community Medicine, Combined Military Hospital Medical College, Lahore, Pakistan
Dr Maujid Masood Malik
Department of Biomedical Sciences, College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
Assistant Professor Shazia Jang Sher
Department of Obstetrics and Gynecology, Bakhtawar Amin Trust Teaching Hospital, Multan, Pakistan
Publication History
Received: July 04, 2022
Revised: November 17, 2022
Accepted: December 10, 2022
Published: December 30, 2022
Abstract
Background and Objective: The discrimination between benign and malignant adnexal masses is important for clinical management and surgical planning in such patients. The risk of malignancy index (RMI) is a combined parameter that is a simple, highly sensitive, and more specific scoring system based on three factors: serum cancer antigen 125 (CA-125) levels, ultrasonographic (USG) score, and menopausal status. The objective of the study is to evaluate the diagnostic efficacy of RMI for the primary evaluation of ovarian masses in females presenting at a local tertiary care hospital in Pakistan.
Methods: This prospective observational study was carried out at the Gynecology outdoor clinic of Fouji Foundation Hospital, Rawalpindi, Pakistan. The study comprised 141 females admitted for surgical exploration of ovarian masses. Pre-operative USG evaluations of ovarian mass, menopausal status, and serum CA-125 levels were determined for all the patients. RMI was calculated and post-operative histopathology of resected ovarian masses was done in all the cases to confirm the diagnosis.
Results: The sensitivity and specificity of CA-125 alone at a cut-off value of 35 U/ml was 67.64% and 83.17% respectively. Using a cutoff value for RMI at 200 U/ml, the specificity and sensitivity of CA-125 were 85.98% and 76.47%, respectively. The receiver operating characteristic curve revealed that RMI was a better discriminate than CA-125, ultrasound, and menopausal status alone.
Conclusion: The RMI is a useful tool in the primary evaluation of ovarian masses. It can be used to differentiate between benign and malignant ovarian masses with high sensitivity and specificity. Suspected malignant patients can be referred to a gynecological oncologist for further management.
Keywords: Risk of malignancy index (RMI), receiver operating curve (ROC), cancer antigen 125 (CA-125), ovarian masses, menopause, ovarian cancer, ovarian tumor.
Pubmed Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher. Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan. BioMedica. 2022; 30 (December 2022): 209-213. doi:10.24911/BioMedica/5-772
Web Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher. Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan. https://biomedicapk.com/articles/online_first/772 [Access: July 03, 2024]. doi:10.24911/BioMedica/5-772
AMA (American Medical Association) Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher. Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan. BioMedica. 2022; 30 (December 2022): 209-213. doi:10.24911/BioMedica/5-772
Vancouver/ICMJE Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher. Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan. BioMedica. (2022), [cited July 03, 2024]; 30 (December 2022): 209-213. doi:10.24911/BioMedica/5-772
Harvard Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher (2022) Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan. BioMedica, 30 (December 2022): 209-213. doi:10.24911/BioMedica/5-772
Chicago Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher. "Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan." 30 (2022), 209-213. doi:10.24911/BioMedica/5-772
MLA (The Modern Language Association) Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher. "Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan." 30.December 2022 (2022), 209-213. Print. doi:10.24911/BioMedica/5-772
APA (American Psychological Association) Style
Rabia Nafees, Humaira Zareen, Zoofishan Imran, Dr Maujid Masood Malik, Assistant Professor Shazia Jang Sher (2022) Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan. , 30 (December 2022), 209-213. doi:10.24911/BioMedica/5-772
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(4):209-213
ORIGINAL ARTICLE
Risk of malignancy index: a useful tool in primary evaluation of ovarian masses at tertiary care center in Pakistan
Rabia Nafees1*, Humaira Zareen2, Zoofishan Imran3, Maujid Masood Malik4, Shazia Jang Sher5
Received: 04 July 2022 Revised date: 17 November 2022 Accepted: 10 December 2022
Correspondence to: Rabia Nafees
*Department of Obstetrics & Gynaecology, Post Graduate Medical Institute, Ameer Ud Deen Medical College, Lahore General Hospital, Lahore, Pakistan.
Email: rabia_nafees@hotmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
The discrimination between benign and malignant adnexal masses is important for clinical management and surgical planning in such patients. The risk of malignancy index (RMI) is a combined parameter that is a simple, highly sensitive, and more specific scoring system based on three factors: serum cancer antigen 125 (CA-125) levels, ultrasonographic (USG) score, and menopausal status. The objective of the study is to evaluate the diagnostic efficacy of RMI for the primary evaluation of ovarian masses in females presenting at a local tertiary care hospital in Pakistan.
Methods:
This prospective observational study was carried out at the Gynecology outdoor clinic of Fouji Foundation Hospital, Rawalpindi, Pakistan. The study comprised 141 females admitted for surgical exploration of ovarian masses. Pre-operative USG evaluations of ovarian mass, menopausal status, and serum CA-125 levels were determined for all the patients. RMI was calculated and post-operative histopathology of resected ovarian masses was done in all the cases to confirm the diagnosis.
Results:
The sensitivity and specificity of CA-125 alone at a cut-off value of 35 U/ml was 67.64% and 83.17% respectively. Using a cut-off value for RMI at 200 U/ml, the specificity and sensitivity of CA-125 were 85.98% and 76.47%, respectively. The receiver operating characteristic curve revealed that RMI was a better discriminate than CA-125, ultrasound, and menopausal status alone.
Conclusion:
The RMI is a useful tool in the primary evaluation of ovarian masses. It can be used to differentiate between benign and malignant ovarian masses with high sensitivity and specificity. Suspected malignant patients can be referred to a gynecological oncologist for further management.
Keywords:
Risk of malignancy index (RMI), receiver operating curve (ROC), cancer antigen 125 (CA-125), ovarian masses, menopause, ovarian cancer, ovarian tumor.
Introduction
One of the common reasons that patients consult a gynecologist is pelvic mass/adnexal mass, which could be benign or malignant.1,2 Ovarian cancer is a silent killer with the highest mortality rate as compared to other female reproductive tract cancers. The high mortality rate for ovarian malignancy is mainly due to the late detection of disease.3 United States preventive service task force found adequate evidence that screening for ovarian cancer doesn’t reduce ovarian cancer mortality and thus recommends against screening for ovarian cancer in asymptomatic women who are not known to have high-risk hereditary cancer syndrome.4 Early detection of ovarian cancers and timely referral to a gynecological oncologist is the key to reducing mortality from ovarian cancers. A single reliable and accurate method, which can accurately predict ovarian malignancies, is still unavailable.5 Available pre-operative assessment tools including pelvic assessment, tumor biomarkers like cancer antigen 125 (CA-125), and radiological investigations, are not adequately sensitive or specific in their individual capacity. Different types of combined pre-operative assessment tools have been reported and studied in the literature to find out some better diagnostic tools.6-8 Among them, the risk of malignancy index (RMI) is one of the commonly used methods, based upon the ultrasound morphological features, menopausal status, and a tumor product, CA-125 that is present in the patient serum as a biomarker.9 RMI is considered a practical and reliable tool in the preoperative discrimination between benign and malignant adnexal masses.10 This study was conducted to determine the accuracy of RMI in the primary evaluation and triaging of the local female patients with adnexal masses presenting at a tertiary care hospital in Pakistan.
Methods
It was a prospective observational study, conducted over a period of 2 years(January 2020 - Jan 2022) at the Gynecology outdoor clinic of Fauji Foundation Hospital, Rawalpindi, Pakistan. The study was approved by the institutional ethical review committee.
Non-probability consecutive sampling technique was used to recruit 141 females admitted for surgical exploration of ovarian masses. Patients having functional cysts of <5 cm, signs evident of metastasis like peritoneal, hepatic, or lung metastasis, etc., already diagnosed ovarian malignancy cases receiving treatment like chemotherapy, or masses arising from organs other than ovaries, were excluded.
Written consent was obtained from the patients followed by acquiring a detailed clinical history, general as well as the gynecological examination and transabdominal or transvaginal ultrasound was also carried out. The evaluation regarding morphological sonographic criteria for adnexal masses included: solid areas, bilaterality, multilocularity, metastases, and ascites. Zero ultrasound score was considered if no positive factor was present, one with a single positive factor, and three if there were two or more positive factors. Serum CA-125 was estimated through a collection of 5 ml venous blood. The status of menopause was also enquired from all the patients and labeled as M = 1 if premenopausal, M = 2 if perimenopausal and M = 3 if postmenopausal. The definition of menopause was taken as women having amenorrhea of 1 year or a hysterectomy was done.11
RMI was calculated for every patient by using a simple regression equation
RMI = U × M × Serum CA-125
In lieu of doubtful ultrasound findings and to see the extent of the disease, a computerized tomography scan was carried out wherever needed. Laparotomy was done in all cases. Adnexal mass specimens obtained after surgeries were sent for the histopathological examination in the Pathology department of the Fauji Foundation Hospital Rawalpindi, Pakistan. The histopathological diagnosis of resected masses was used for a definite outcome.
Statistical analysis
All the data were encoded in (International Business Machines) IBM Statistical Package for the Social Sciences version 25.0. Data for CA-125 and RMI were analyzed separately. Sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were calculated at different cutoff levels. Diagnostic accuracy of CA-125, ultrasound, menopausal status, and RMI each were determined by receiver operating characteristic curves (ROC) conventionally prepared by plotting sensitivity against specificity over a prescribed range of analytical values. The level of significance was taken as 5%.
Results
Histopathology of the surgical specimens revealed 107 benign masses (75.9%) and 34 malignant (24.1%). The mean age of the participants enrolled having benign and malignant masses was 39.41 ± 12.21 years and 46.35 ± 17.18 years, respectively. Histopathological subtypes of the ovarian masses are shown in Table 1. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio of RMI, and CA-125 at different cut-off values are shown in Table 2. Best performance of RMI and serum CA-125 was seen at cut-off values of 200 and 50 u/ml respectively. ROC (Figures 1 and 2) of CA-125, ultrasound score, menopausal status, and RMI showed that among all the parameters, RMI had the highest area under the curve.
Table 1. Histopathological types of ovarian masses diagnosed in 141 females.
| Benign tumors | Malignant tumors | ||
|---|---|---|---|
| Subtype | Frequency (107) | Subtype | Frequency (32) |
| Serous cystadenoma | 10 | Serous cystadenocarcinoma | 12 |
| Mucinous cystadenoma | 7 | Mucinous cystadenocarcinoma | 5 |
| Mature teratoma | 22 | Endometroid adenocarcinoma | 2 |
| Endometrioma | 25 | Sarcomatous tumor | 3 |
| Benign ovarian cysts | 30 | Immature teratoma | 2 |
| Granulosa cell tumor | 4 | ||
| Fibroma | 2 | Dysgerminoma | 1 |
| Fibrothecoma | 2 | Ovarian yolk sac tumor | 1 |
| Paraovarian cyst | 2 | Fallopian tube adenocarcinoma | 1 |
| Tubo-ovarian abscess | 3 | Peritoneal carcinoma | 1 |
| Para-tubal cyst | 3 | ||
Discussion
Pre-operative primary evaluation of ovarian/pelvic masses with different methods has been investigated in the literature.6-8 One of the most frequently adopted methods is RMI.12 As until now, no single method is available that can accurately predict ovarian malignancy, we conducted this study with the hypothesis that the multiparametric scoring system of RMI could serve as a useful tool in the primary evaluation of disease of the ovarian tissue, in low-resource settings.
The mean age of the participants enrolled in this study having benign and malignant masses was 39.41 ± 12.21 years and 46.35 ± 17.18 years which is comparable to the mean age of the patients with malignant and benign masses in a study by Qiu et al.13 (46.58 ± 9.80 years and 37.11 ± 12.20 years, respectively) and Al-Asadi et al.10 (58.4 ± 8.4 years and 36.9 ± 10.7 years respectively).
In this study, 75.9% of patients were having benign ovarian masses while 25.1% of patients had malignant ones. An Indian study reported a higher percentage of malignant tumors [54.76% (69/126)] as compared to benign tumors (45.24%).1 Qiu et al.13 however reported a lower frequency [69 (45.7%)] of females with malignant disease as compared to benign pathology [82 (54.3%)].with13 In this study, different cut-off values of the RMI were assessed to determine the best predictive value for malignancy risk. The cut-off value of 200 provided the highest sensitivity, specificity, and positive and negative likelihood ratios. Most of the other studies also reported higher diagnostic accuracy of RMI at cut off point of 200.4-6
Serum CA-125 levels are used in the estimation of the risk regarding cancer of the ovarian tissue, though increased levels might also be due to other gynecological pathologies.14,15
CA-125 levels, ultrasound score, and menopausal score when used alone in the screening of ovarian masses are not very effective; specificity is enhanced when coupled with RMI.16 In this study, ROC drawn for CA-125 levels, ultrasound score, menopausal status, and RMI (Figures 1 and 2) shows that RMI has the highest area under the curve among all the parameters which means RMI has better sensitivity and specificity to differentiate between malignant and benign ovarian tumors. The superiority of RMI as compared to other parameters in estimating the risk of ovarian malignancy has been reported in several studies. Hayam and colleagues in their study of comparison between benign and malignant ovarian masses revealed that there was a statistically significant difference between the two groups regarding all the RMI indices (p-value < 0.001) while ROC analysis of the five RMI indices showed that the best method for prediction of malignant tumors was RMI.17 In an Indian study on 73 patients with ovarian masses, RMI2 showed a sensitivity of 86.6%, specificity of 86.5%, positive predictive value of 81.25%, and negative predictive value of 90.24% whereas RMI4 showed a sensitivity of 86.6%, specificity of 86.5%, positive predictive value of 83.87, and negative predictive value of 90.48%. The authors concluded that the RMI 2 and 4 are almost comparable with each other and so either can be used for determining the risk of malignancy in patients with adnexal masses.18
Table 2. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio of RMI, and CA-125 at different cut-off values.
| Variables | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) | Likelihood ratio Positive | Likelihood ratio Negative |
|---|---|---|---|---|
| CA-125 (U/ml) | ||||
| 10 | 91.17 (76-98) | 41.12 (31-51) | 4.66 (1.54-14.05) | 0.645 (0.534-0.78) |
| 35 | 67.64 (49-82) | 83.17 (74-89) | 2.57 (1.56-4.21) | 0.248 (0.153-0.4) |
| 50 | 67.64 (49-82) | 87.85 (80-93) | 2.71 (1.66-4.43) | 0.179 (0.102-0.31) |
| 65 | 52.94 (35-70) | 87.85 (80-93) | 1.86 (1.29-2.68) | 0.229 (0.125-0.41) |
| 150 | 32.35 (17-50) | 94.39 (88-97) | 1.39 (1.1-1.76) | 0.173 (0.069-0.43) |
| RMI | ||||
| 30 | 91.17 (76-98) | 42.05 (32-51) | 4.76 (1.58-14.36) | 0.635 (0.524-0.77) |
| 100 | 82.35 (65-93) | 75.7 (66-83) | 4.28 (2.05-8.93) | 0.295 (0.204-0.42) |
| 150 | 0 (0-10) | 100 (96-100) | 1 (1-1) | None |
| 200 | 76.47 (58-89) | 85.98 (77-91) | 3.65 (1.98-6.73) | 0.183 (0.11-0.3) |
| 500 | 50 (32-67) | 93.45 (86-97) | 1.86 (1.33-2.62) | 0.13 (0.059-0.28) |
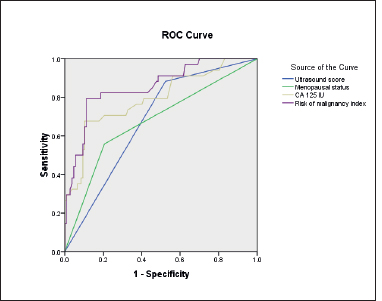
Figure 1. Receiver operator characteristic curve (CA-125 levels, ultrasound score, menopausal status, and RMI).
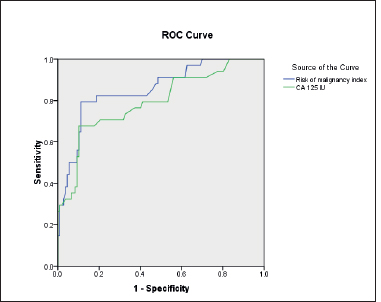
Figure 2. Receiver operator characteristic curve (RMI and CA-125 levels).
This study also advocates the role of RMI as a predictive parameter for the evaluation of risk or probability of ovarian malignancy in females, especially for those presenting with clinically equivocal masses.
Conclusion
RMI is a useful tool in the primary evaluation of patients with adnexal masses with a subsequent referral of higher malignancy risk patients to gynecological oncologists for providing effective as well as timely interventional strategies.
Acknowledgement
The authors would like to acknowledge the support of the staff and faculty of the Departments of Obstetrics & Gynecology and Histopathology at the Fauji Foundation Hospital, Rawalpindi, Pakistan for execution of this research.
List of Abbreviations
| CA 125 | Cancer Antigen 125 |
| RMI | Risk of malignancy index |
| ROC | Receiver operating characteristic curve |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The ethical approval was obtained from the institutional Ethical Review Committee of Fauji Foundation Hospital, Rawalpindi, Pakistan vide letter no. FF/FUMC/215-79/Phy/20, dated 17 November, 2019.
Authors’ contributions
RN, HZ: Conception and study design, acquisition of data, and drafting of manuscript.
ZI, MM, SJ: Analysis and interpretation of data, revision of manuscript with critical intellectual input.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Rabia Nafees1, Humaira Zareen2, Zoofishan Imran3, Maujid Masood Malik4, Shazia Jang Sher5
- Department of Obstetrics & Gynaecology, Post Graduate Medical Institute, Ameer Ud Deen Medical College, Lahore General Hospital, Lahore, Pakistan
- Department of Obstetrics & Gynecology, College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
- Department of Community Medicine, Combined Military Hospital Medical College, Lahore, Pakistan
- Department of Biomedical Sciences, College of Medicine, King Faisal University, Al-Ahsa, Saudi Arabia
- Department of Obstetrics and Gynecology, Bakhtawar Amin Trust Teaching Hospital, Multan, Pakistan
References
- Dora SK, Dandapat AB, Pande B, Hota JP. A prospective study to evaluate the risk malignancy index and its diagnostic implication in patients with suspected ovarian mass. J Ovarian Res. 2017;10(1):55. https://doi.org/10.1186/s13048-017-0351-2.
- Kaur A, Sharma S, Singh S. Role of risk of malignancy index 4 in evaluation of adnexal masses. Int J Reprod Contracept Obstet Gynecol. 2020;9(9):3818–24. https://doi.org/10.18203/2320-1770.ijrcog20203863.
- Karen JC. UpToDate 18. In: B. Goff, editor. The Netherland: Wolter Kluwer; 2018.
- Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, et al. US Preventive services task force. Screening for ovarian cancer: US preventive services task force recommendation statement. JAMA. 2018;319(6):588–94. https://doi.org/10.1001/jama.2017.21926.
- Aziz AB, Najmi N. Is risk malignancy index a useful tool for predicting malignant ovarian masses in developing countries? Obstet Gynecol Int. 2015;2015:951256. https://doi.org/10.1155/2015/951256.
- Van Calster B, Valentin L, Froyman W, Landolfo C, Ceusters J, Testa AC, et al. Validation of models to diagnose ovarian cancer in patients managed surgically or conservatively: multicentre cohort study. BMJ. 2020;370:m2614. https://doi.org/10.1136/bmj.m2614.
- Westwood M, Ramaekers B, Lang S, Grimm S, Deshpande S, de Kock S, et al. Risk scores to guide referral decisions for people with suspected ovarian cancer in secondary care: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2018;22(44):1–264. https://doi.org/10.3310/hta22440.
- Chacón E, Dasí J, Caballero C, Alcázar JL. Risk of ovarian malignancy algorithm versus risk malignancy index-I for preoperative assessment of adnexal masses: a systematic review and meta-analysis. Gynecol Obstet Invest. 2019;84(6):591–8. https://doi.org/10.1159/000501681.
- Rao PS, Reenu B, Prajwal S. Risk of malignancy index in ovarian tumour for predicting ovarian malignancy by using Jacob’s score. Int J Reprod Contracept Obstet Gynecol. 2017;6(4):1318. https://doi.org/10.18203/2320-1770.ijrcog20171385.
- Al-Asadi JN, Al-Maliki SK, Al-Dahhhan F, Al-Naama L, Suood F. The accuracy of risk malignancy index in prediction of malignancy in women with adnexal mass in Basrah, Iraq. Niger J Clin Pract. 2018;21(10):1254–9.
- Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990;97(10):922––9. https://doi.org/10.1111/j.1471-0528.1990.tb02448.x.
- Timmerman D, Ameye L, Fischerova D, Epstein E, Melis GB, Guerriero S, et al. Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: prospective validation by IOTA group [Internet]. BMJ. 2010;341:c6839. https://doi.org/10.1136/bmj.c6839.
- Qiu L, Yang F, Luo H. A preliminary study: the sequential use of the risk malignancy index and contrast-enhanced ultrasonography in differential diagnosis of adnexal masses. Medicine (Baltimore). 2018;97(29):e11536. https://doi.org/10.1097/MD.0000000000011536.
- Nazneen T, Begum SA, Mahmud T, Khatoon F, Islam F, Amatullah M. Preoperative analysis of CA-I25 and its relation with histopathological study in ovarian tumours. Mymensingh Med J. 2021;30(2):402–9.
- McGuire V, Hartge P, Liao LM, Sinha R, Bernstein L, Canchola AJ, et al. Parity and oral contraceptive use in relation to ovarian cancer risk in older women. Cancer Epidemiol Biomarkers Prev. 2016;25(7):1059–63. https://doi.org/10.1158/1055-9965.EPI-16-0011.
- Al-Musalhi K, Al-Kindi M, Ramadhan F, Al-Rawahi T, Al-Hatali K, Mula-Abed WA. Validity of cancer antigen-125 (ca-125) and risk of malignancy index (rmi) in the diagnosis of ovarian cancer. Oman Med J. 2015;30(6):428–34. https://doi.org/10.5001/omj.2015.85.
- Hayam FM, Ashraf MQ, Hassan MK. Assessment of the value of a modified risk of malignancy index (rmi) in preoperative discrimination between benign and malignant ovarian masses. Gynecol Obstet (Sunnyvale). 2016;6(4):417–21. https://doi.org/10.4172/2161-0932.1000417.
- Suchitra R, Burde K, Nilima G, Sahithi PL. Evaluation of the risk of malignancy index in preoperative diagnosis of ovarian masses. IJRCOG. 2018;7(10):4202–9. https://doi.org/10.18203/2320-1770.ijrcog20184152.
