Original Article
VOLUME: 39 | ISSUE: 2 | Jun 25, 2023 | PAGE: (84 - 90) | DOI: 10.24911/BioMedica/5-991
Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab
Authors:
Sadia Anwar
, Fakeha Rehman
, Samreen Hameed
,
Article Info
Authors
Sadia Anwar
Associate Professor, Pathology Department, Ameer-ud-Din Medical College/Postgraduate Medical Institute, Lahore, Pakistan.
Fakeha Rehman
Associate Professor, Pathology Department, Ameer-ud-Din Medical College/Postgraduate Medical Institute, Lahore, Pakistan.
Samreen Hameed
Associate Professor, Pathology Department, King Edward Medical University, Lahore, Pakistan.
Publication History
Received: March 10, 2023
Revised: May 22, 2023
Accepted: June 12, 2023
Published: June 25, 2023
Abstract
Background and Objective: Thyroid specimens constitute a major bulk of the head and neck surgical specimens received at the Pathology Departments. Careful handling of the specimens in the grossing room will result in an efficient reporting of useful histological parameters required for patient management and prognosis. The objective of this study was to analyze different errors and near-miss events in the grossing of thyroid specimens in the surgical pathology gross room of a Tertiary Care Hospital in Lahore, Pakistan.
Methods: A cross-sectional analysis was done on different thyroid specimens received at the Pathology reception of Lahore General Hospital, Lahore, Pakistan, from January 2022 to April 2023. Different types of errors involved in standard gross examinations were studied. Data were entered using SPSS version 23.0.
Results: Errors observed in the preanalytical phase included the use of inappropriate fixative (15.2%), insufficient clinical information (76.5), mislabeled jar/request form (7.6%), and loss of specimen (8%). Grossing errors included insufficient grossing notes (12.2%), cutting thick slices (10.7%), missing lesions on gross examination (9.9%), inappropriate inking (6.9%), overfilling cassette with large tissue sections (6.9%), mislabeled cassettes (93.8%), and incomplete submission of capsule (2.3%).
Conclusion: This study concludes that errors and near-miss events in handling thyroid specimens can be avoided by effective training of the handling staff and grossing residents. Collaboration between clinical wards and histopathology laboratories can also be helpful in this regard.
Keywords: Errors, grossing, gross room, near-miss events, thyroid specimens, biopsies, surgical pathology.
Pubmed Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed. Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab. BioMedica. 2023; 25 (June 2023): 84-90. doi:10.24911/BioMedica/5-991
Web Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed. Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab. https://biomedicapk.com/articles/online_first/991 [Access: July 27, 2024]. doi:10.24911/BioMedica/5-991
AMA (American Medical Association) Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed. Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab. BioMedica. 2023; 25 (June 2023): 84-90. doi:10.24911/BioMedica/5-991
Vancouver/ICMJE Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed. Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab. BioMedica. (2023), [cited July 27, 2024]; 25 (June 2023): 84-90. doi:10.24911/BioMedica/5-991
Harvard Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed (2023) Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab. BioMedica, 25 (June 2023): 84-90. doi:10.24911/BioMedica/5-991
Chicago Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed. "Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab." 25 (2023), 84-90. doi:10.24911/BioMedica/5-991
MLA (The Modern Language Association) Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed. "Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab." 25.June 2023 (2023), 84-90. Print. doi:10.24911/BioMedica/5-991
APA (American Psychological Association) Style
Sadia Anwar, Fakeha Rehman, Samreen Hameed (2023) Analysis of Near-Miss Events and Errors in Handling Thyroid Specimens; A Gross Room Experience from a Pathology Lab. , 25 (June 2023), 84-90. doi:10.24911/BioMedica/5-991
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 39(2):84-90
ORIGINAL ARTICLE
Analysis of near-miss events and errors in handling thyroid specimens; a gross room experience from a Pathology Laboratory
Sadia Anwar1, Fakeha Rehman1*, Samreen Hameed2
Received: 10 March 2023 Revised date: 22 May 2023 Accepted: 12 June 2023
Correspondence to: Fakeha Rehman
*Associate Professor, Pathology Department, Ameer-ud-Din Medical College/Postgraduate Medical Institute, Lahore, Pakistan.
Email: sohnia@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Thyroid specimens constitute a major bulk of the head and neck surgical specimens received at the Pathology Departments. Careful handling of the specimens in the grossing room will result in an efficient reporting of useful histological parameters required for patient management and prognosis. The objective of this study was to analyze different errors and near-miss events in the grossing of thyroid specimens in the surgical pathology gross room of a Tertiary Care Hospital in Lahore, Pakistan.
Methods:
A cross-sectional analysis was done on different thyroid specimens received at the Pathology reception of Lahore General Hospital, Lahore, Pakistan, from January 2022 to April 2023. Different types of errors involved in standard gross examinations were studied. Data were entered using SPSS version 23.0.
Results:
Errors observed in the preanalytical phase included the use of inappropriate fixative (15.2%), insufficient clinical information (76.5), mislabeled jar/request form (7.6%), and loss of specimen (8%). Grossing errors included insufficient grossing notes (12.2%), cutting thick slices (10.7%), missing lesions on gross examination (9.9%), inappropriate inking (6.9%), overfilling cassette with large tissue sections (6.9%), mislabeled cassettes (93.8%), and incomplete submission of capsule (2.3%).
Conclusion:
This study concludes that errors and near-miss events in handling thyroid specimens can be avoided by effective training of the handling staff and grossing residents. Collaboration between clinical wards and histopathology laboratories can also be helpful in this regard.
Keywords:
Errors, grossing, gross room, near-miss events, thyroid specimens, biopsies, surgical pathology.
Introduction
A histopathological report of a surgical specimen is the mainstay in determining the prognosis and clinical management of the patients.1 Its quality is reliant on specimen management, starting from the collection in the sampling area till the release of the results, encompassing multiple supporters from various disciplines. Errors in reporting not only result in distrust of laboratory services but can also mislead the physicians in treating patient’s disease.2
For an effective root cause analysis of laboratory errors, it is important to define the phase of the laboratory testing in which the error was encountered. A laboratory test has three phases of testing, including preanalytical, analytical, and postanalytical. Many stakeholders involving operation theatre attendants, ward attendants, physicians, laboratory receptionists, IT team, transcriptionists, surgical pathology residents, and consultants, are involved in all these phases. Therefore, generation of a good quality report is dependent on and needs full commitment and responsibility from these stakeholders.3,4
Thyroid gland pathology and specimen management are different from the rest of the organs in the body. The criteria to rule out malignancy include nuclear features of the malignancy, capsular and vascular invasion, and anaplasia. This is made possible only with an effective surgical excision and adequate preservation and sampling of the submitted specimen.5
Various studies revealed that most of the preanalytical errors were mainly encountered in specimen identification, order entry, specimen collection and preservation, and transport to the laboratory reception.6,7 The aim of this study is to analyze the type and frequency of errors occurring in the preanalytical and grossing phases of various types of thyroid specimens. Analyzing these errors will help in better understanding the cause and rectification of the error for better outcomes.
Methods
A cross-sectional analysis was done on different types of 132 thyroid specimens submitted at the Pathology Department of Lahore General Hospital, Lahore, Pakistan, from January 2022 to April 2023. Various errors and near-miss events encountered in a preanalytical and grossing phases were recorded by voluntary observation in the Histopathology Department. Near miss event means any unsafe situation that is indistinguishable from a preventable adverse event except for the outcome. A patient is exposed to a hazardous situation, but does not experience harm either through luck or early detection, while error is a broader term referring to any act of commission (doing something wrong) or omission (failing to do the right thing) that exposes patients to a potentially hazardous situation.
Ethical approval of the study was taken from the Institutional Ethical Review Committee. Different types of thyroid specimens included were lobectomies, isthmusectomies, nodule excision, lobectomies with isthmusectomies, and thyroidectomies (subtotal and total). Request forms and reports of the thyroid specimens were collected and scrutinized along with the surgical specimen status before and after grossing the specimen in the standard gross room. Patient consent was not required as this study did not involve any human subjects research. Cytology and frozen sections were excluded from the study. Surgical specimen events were classified by the specimen type and the type of event.
Statistical analysis
Data were entered using SPSS version 23.0. Quantitative variables, such as the size of the tumor, number of errors, and so on, were presented as mean+/- SD, whereas qualitative variables, such as type of specimen, type of error, or near-miss event, were presented as frequencies and percentages. The chi-square test was applied to find the associations between types of procedures and different preanalytical and grossing errors.
Results
The most frequently received specimen was lobectomy (50.8%), followed by thyroidectomy (25.8%), lobectomy with isthmusectmy (22%), and nodule excision alone in 2 (1.55) cases. Types of preanalytical errors included insufficient clinical information in 101 cases (76.5%), use of inappropriate fixatives (15.2%), and mislabeled jar/request form (7.6%). Only one specimen out of 132 specimens (0.8%) was lost (Figure 1).
Types of grossing errors included an inappropriate recording of dimensions in 35 cases (26.7%), followed by improper fixation (13.0%), and insufficient grossing notes (12.2%). Other types of errors encountered are listed in Table 1.
The most common peanalytical error seen was insufficient clinical information that was observed in 2 (100%) of nodule excision specimens, 59 (88.1%) of lobectomy specimens, 25 (86.2%) of lobectomy with isthumusectomy specimens, and 15 (44.1%) of thyroidectomy specimens. Mislabeled jar/request form was found in 8 (23.5%) of thyroidectomy and 2 (3.0%) of lobectomy specimens. None of the nodule excision and lobectomy with isthumusectomy specimens showed this error (p-value <0.001) (Table 2). Lack of documentation of specimen type failed to include many significant events and errors. Reports were reviewed by expert pathologists and subject specialists to scrutinize reports in which relevant gross information was missing. Specimen photography was missed in many of the cases, but it was felt particularly substantial in specimens with suspicion of tumors.
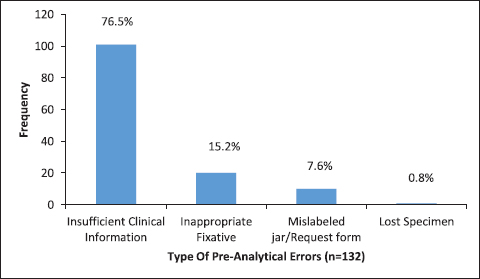
Figure 1. Different types of preanalytical errors (n = 132).
Different types of grossing errors were also seen in different types of specimens. Most common observed error was inappropriate recording of dimensions seen in 15 (22.4%) of lobectomy, 12 (41.4%) of lobectomy with isthumusectomy, 1 (50%) of nodule excision, and 7 (21.2%) of thyroidectomy specimens (p-value = 0.010) (Table 3).
Different types of preanalytical (Table 4) and grossing errors (Table 5) were also observed in relation to the year of residency of the trainees involved in grossing; however, no significant association was seen (p-value = 0.180, 0.436).
Discussion
This study examines a significant proportion of errors encountered in handling thyroid specimens received at one of the busiest Pathology Sections of a public sector teaching hospital in Lahore, Pakistan. The frequency of reporting errors was low (23%), and interpreted data are not representative of all the errors in the preanalytical and grossing phase (Table 1, Figure 1). This may be due to the fear of accountability and the lack of an effective error management system. Instituting regular quality checks and providing a blame-free environment may be helpful in encouraging employees to report errors.4-8
Although the majority of labeling issues were near-misses, it can have serious repercussions when specimens are misinterpreted or labeled with the wrong patient’s name or clinical information, which can be crucial for the pathologist to interpret the specimen correctly.
Table 1. Different types of grossing errors (n = 131).
| Type of grossing error | Frequency | Percent |
|---|---|---|
| Improper fixation | 17 | 13.0 |
| Inappropriate recording of dimensions | 35 | 26.7 |
| Inappropriate submission of capsule | 3 | 2.3 |
| Insufficient application of ink | 9 | 6.9 |
| Insufficient grossing notes | 16 | 12.2 |
| Mislabeling cassette | 5 | 3.8 |
| Missing lesion on gross examination | 13 | 9.9 |
| Missing margin and distance of tumor from margin | 10 | 7.6 |
| Overfilling cassette with large tissue section | 9 | 6.9 |
| Thick slices | 14 | 10.7 |
| Total | 131 | 100.0 |
Table 2. Different types of preanalytical errors are seen in different types of procedures.
| Type of preanalytical error | Total | ||||
|---|---|---|---|---|---|
| Type of procedure | Inappropriate fixative | Insufficient clinical information | Lost specimen | Mislabeled jar/request form | |
| Lobectomy | 6 | 59 | 0 | 2 | 67 |
| 9.0% | 88.1% | 0.0% | 3.0% | 100.0% | |
| Lobectomy with isthmusectomy | 4 | 25 | 0 | 0 | 29 |
| 13.8% | 86.2% | 0.0% | 0.0% | 100.0% | |
| Nodule excision | 0 | 2 | 0 | 0 | 2 |
| 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |
| Thyroidectomy | 10 | 15 | 1 | 8 | 34 |
| 29.4% | 44.1% | 2.9% | 23.5% | 100.0% | |
| Total | 20 | 101 | 1 | 10 | 132 |
| 15.2% | 76.5% | 0.8% | 7.6% | 100.0% | |
Table 3. Different types of grossing errors are seen in different procedures (n = 131).
| Grossing error | Type of procedure | Total | |||
|---|---|---|---|---|---|
| Lobectomy | Lobectomy with isthmusectomy | Nodule excision | Thyroidectomy | ||
| Improper fixation | 13 | 3 | 0 | 1 | 17 |
| 19.4% | 10.3% | 0.0% | 3.0% | 13.0% | |
| Inappropriate recording of dimensions | 15 | 12 | 1 | 7 | 35 |
| 22.4% | 41.4% | 50.0% | 21.2% | 26.7% | |
| Inappropriate submission of capsule | 1 | 1 | 1 | 0 | 3 |
| 1.5% | 3.4% | 50.0% | 0.0% | 2.3% | |
| Insufficient application of ink | 5 | 2 | 0 | 2 | 9 |
| 7.5% | 6.9% | 0.0% | 6.1% | 6.9% | |
| Insufficient grossing notes | 9 | 2 | 0 | 5 | 16 |
| 13.4% | 6.9% | 0.0% | 15.2% | 12.2% | |
| Mislabeling cassette | 4 | 0 | 0 | 1 | 5 |
| 6.0% | 0.0% | 0.0% | 3.0% | 3.8% | |
| Missing lesion on gross examination | 6 | 3 | 0 | 4 | 13 |
| 9.0% | 10.3% | 0.0% | 12.1% | 9.9% | |
| Missing margin and distance of the tumor from ma | 1 | 3 | 0 | 6 | 10 |
| 1.5% | 10.3% | 0.0% | 18.2% | 7.6% | |
| Overfilling cassette with large tissue sections | 3 | 2 | 0 | 4 | 9 |
| 4.5% | 6.9% | 0.0% | 12.1% | 6.9% | |
| Thick slices | 10 | 1 | 0 | 3 | 14 |
| 14.9% | 3.4% | 0.0% | 9.1% | 10.7% | |
| Total | 67 | 29 | 2 | 33 | 131 |
| 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | |
Table 4. Different types of preanalytical errors were seen with the year of residency of trainees (n = 132).
| Pre analytic Error | Year of residency | Total | |||
|---|---|---|---|---|---|
| Residency year 1 | Residency year 2 | Residency year 3 | Residency year 4 | ||
| Inappropriate fixative | 12 | 3 | 5 | 0 | 20 |
| 21.1% | 8.3% | 15.6% | 0.0% | 15.2% | |
| Insufficient clinical information | 38 | 31 | 26 | 6 | 101 |
| 66.7% | 86.1% | 81.3% | 85.7% | 76.5% | |
| Lost specimen | 0 | 0 | 1 | 0 | 1 |
| 0.0% | 0.0% | 3.1% | 0.0% | 0.8% | |
| Mislabeled jar/request form | 7 | 2 | 0 | 1 | 10 |
| 12.3% | 5.6% | 0.0% | 14.3% | 7.6% | |
| Total | 57 | 36 | 32 | 7 | 132 |
| 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | |
The unsatisfactory outcome of the histopathology request form continues to be a concern among laboratory workers. The majority of the insufficient clinical information was observed in lobectomy and lobectomy with isthmusectomy specimens (88.1% and 86.2%, respectively).
Other problem-prone processes in the preanalytical phase were specimen collection, preservation, and transport. Of particular concern is that many specimens were compromised when prepared with incorrect transport medium/fixative. Commonly, reports indicated that specimens were not received in the laboratory, having been either temporarily or permanently lost. However, in our study, just one specimen was lost during transport of the specimen from the ward to the Pathology reception (n = 1, 0.8%).
Table 5. Different types of grossing errors are seen with the year of residency of trainees (n = 131).
| Grossing error | Year of residency | Total | |||
|---|---|---|---|---|---|
| Residency year 1 | Residency year 2 | Residency year 3 | Residency year 4 | ||
| Improper fixation | 9 | 3 | 4 | 1 | 17 |
| 15.8% | 8.3% | 12.9% | 14.3% | 13.0% | |
| Inappropriate recording of dimensions | 14 | 11 | 8 | 2 | 35 |
| 24.6% | 30.6% | 25.8% | 28.6% | 26.7% | |
| Inappropriate submission of capsule | 1 | 1 | 1 | 0 | 3 |
| 1.8% | 2.8% | 3.2% | 0.0% | 2.3% | |
| Insufficient application of ink | 3 | 2 | 4 | 0 | 9 |
| 5.3% | 5.6% | 12.9% | 0.0% | 6.9% | |
| Insufficient grossing notes | 7 | 5 | 2 | 2 | 16 |
| 12.3% | 13.9% | 6.5% | 28.6% | 12.2% | |
| Mislabeling of cassette | 2 | 3 | 0 | 0 | 5 |
| 3.5% | 8.3% | 0.0% | 0.0% | 3.8% | |
| Missing lesion on gross examination | 8 | 2 | 3 | 0 | 13 |
| 14.0% | 5.6% | 9.7% | 0.0% | 9.9% | |
| Missing margin and distance of tumor from margin | 7 | 0 | 3 | 0 | 10 |
| 12.3% | 0.0% | 9.7% | 0.0% | 7.6% | |
| Overfilling cassette with large tissue section | 3 | 2 | 2 | 2 | 9 |
| 5.3% | 5.6% | 6.5% | 28.6% | 6.9% | |
| Thick slices | 3 | 7 | 4 | 0 | 14 |
| 5.3% | 19.4% | 12.9% | 0.0% | 10.7% | |
| Total | 57 | 36 | 31 | 7 | 131 |
| 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | |
A study conducted in Ethiopia by Tola et al.4 reported preanalytical errors (75.5%) were the highest in frequency, while another study from India also found preanalytical errors making 77.7% of the total errors in thyroid grossing.9
Pathologic findings are particularly important in surgical specimens containing malignant neoplasms for the determination of the prognosis and type of adjuvant therapy. The most frequently detected analytical errors were due to the standard protocol not being followed by the laboratory professionals, which contributed to 31 (2.8%) of the total errors. Standard operating procedures (SOPs) are used by the laboratories to ensure proper test selection, sample collection, and processing.
Most of the near-miss events and errors involved more than one phase (n = 69, 52.27%). The majority of the requisition forms lacked the significant clinical and radiological data important in making a final histopathological diagnosis. This data were in accordance with the results of other similar studies.10-12 Inappropriate jar size, poor quality fixative, and delayed transport to the laboratory resulted in autolyzed specimens. Furthermore, lack of supervision and training of junior residents and irresponsible attitudes on the part of both technical staff and grossing residents may be attributed. A maximum number of errors were seen in the recording of gross dimensions of the specimen, particularly by the grossing trainees of the second year of residency (30.6%) Morelli et al.13 observed that 28% of the errors were encountered in gross dissection of the surgical specimens in the analytical phase.13
Capsular invasion has a significant role in differentiating between follicular adenoma and carcinoma. In our study, capsule submission was found to be insufficient in only 2.4% of cases. Most of these errors were observed in the residents who were in the third year of their residency (3.8%). A study conducted by Hamza et al.5 examined 80 patients who had been diagnosed with follicular adenoma. Based on the pathological diagnoses of specimens from the entire capsule, they observed capsular invasion in three patients (3.8%). Oh et al.6 previously prepared additional blocks by vertically slicing the upper and lower ends of the transverse section of thyroid nodule specimens; this technique resulted in an approximately two-fold increase in the number of diagnoses of capsular invasion; however, there was no change in the frequency of vascular invasion observed. Thus, it can be assumed that increasing the number of tissue blocks used for the diagnosis could result in the increased frequency of diagnosis of suspected cases of capsular invasion.
The results of our study will help in better coordination between all the stakeholders involved in the surgical specimen collection, transport, submission, and gross examination. It will also play an important role in reducing the wastage of resources and will help physicians make precise decisions regarding patient’s treatment.14,15 Limited access to the authorized data, noncooperative attitudes on the part of the healthcare professionals involved in handling different phases of thyroid specimen handling, and loss of specimen follow-up during data tracking were limitations of this study. However, this study significantly contributed to delivering a strong insight into the possible causes of the errors and the factors contributing to them. These events are critical to patient care and outcomes, including the need for additional testing, therapy, and patient monitoring, as well as extended hospital stays, higher levels of care, hospitalizations, and additional surgical procedures may have an impact.16,17 Measuring the cost of this additional care is beyond the scope of this article, but it can be a significant expense and warrants further investigation.18
The basic components of laboratory processing, with emphasis on all three phases of testing, including preanalytical, analytical, and postanalytical phases, should be prioritized in orientation training for all newly inducted laboratory workers, residents, and other users of laboratory services.19 Joint conferences and review meetings between physicians and laboratories should be revived and maintained to share knowledge, enhance communication, and facilitate feedback for quality improvement. Regular comprehensive laboratory audits, compliance with predefined SOPs, and comparing baseline information with postassessment data can effectively aid in continuous quality improvement efforts.
Conclusion
Pathology laboratory errors can have catastrophic effects on patients and result in major unfavorable patient outcomes. The present study was designed to focus on the near-miss events and errors in the preanalytical and grossing phase of specimen testing in the histopathology laboratory. This study could not provide any evidence of a significant correlation between grossing errors and type of specimens; however, insufficient clinical information had a major contributory role in preanalytical errors.
Limitations of the Study
The small sample size was a limitation in this study. Future studies shall be conducted with a larger sample size and the inclusion of all three phases of laboratory testing to establish significant correlations between different parameters.
Acknowledgement
The authors are grateful to the Head of the Pathology Department at the Postgraduate Medical Institute, Lahore, Pakistan, for the permission to access the data of the Pathology laboratory archives.
List of Abbreviations
| SOPs | Standard operating procedures |
Conflict of interests
None to declare.
Grant support and financial disclosure
None to disclose.
Authors’ contributions
FR, SA: Concept and design of study, acquisition, and analysis of data, drafting of the manuscript.
SA, SH: Critical intellectual input to the manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Ethical approval
Ethical approval of the study was taken from the Institutional Ethical Review Committee of the Postgraduate Medical Institute/Lahore General Hospital, Lahore, Pakistan, vide Reference No. 00-16-A-2023, dated 14th January, 2023.
Authors’ Details
Sadia Anwar1, Fakeha Rehman1, Samreen Hameed2
- Associate Professor, Pathology Department, Ameer-ud-Din Medical College/Postgraduate Medical Institute, Lahore, Pakistan
- Associate Professor, Pathology Department, King Edward Medical University, Lahore, Pakistan
References
- Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016 Jan;26(1):1–133. https://doi.org/10.1089/thy.2015.0020
- Krishnan RP, Ramani P, Sherlin HJ, Sukumaran G, Ramasubramanian A, Jayaraj G, et al. Surgical specimen handover from operation theater to laboratory: a survey. Ann Maxillofac Surg. 2018;8(2):234–8. https://doi.org/10.4103/ams.ams_51_18
- RCPA. Guidelines for authors of structured cancer pathology reporting protocols. Surry Hills, Australia: RCPA; 2009.
- Tola EK, Dabi YT, Dano GT. Assessment of types and frequency of errors in diagnostic laboratories among selected hospitals in East Wollega Zone, Oromia, Ethiopia. Pathol Lab Med Int. 2022;14:1–6. https://doi.org/10.2147/PLMI.S351851
- Hamza A, Khawar S, Alrajjal A, Salehi S. Processing the entire capsule in thyroid follicular lesions improves diagnostic accuracy. Ann Diagn Pathol. 2019 Apr;39:21–4. https://doi.org/10.1016/j.anndiagpath.2018.12.007
- Oh HS, Kim SJ, Song E, Lee YM, Sung TY, Kim WG, et al. Modified transverse-vertical gross examination: a better method for the detection of definite capsular invasion in encapsulated follicular-patterned thyroid neoplasms. Endocr Pathol. 2019 Jun;30(2):106–12. https://doi.org/10.1007/s12022-019-9565-8
- Lacout A, Chamorey E, Thariat J, El Hajjam M, Chevenet C, Schiappa R, et al. Insight into differentiated thyroid cancer gross pathological specimen shrinkage and its influence on TNM staging. Eur Thyroid J. 2017 Nov;6(6):315–20. https://doi.org/10.1159/000478774
- Koyuncuer A, Bayraktar SG, Gurkan E. Histopathologic examination of thyroidectomy specimens from 1149 nodular goiter patient. Acta Med Mediter. 2016;32:35–43.
- Rao S, Masilamani S, Sundaram S, Duvuru P, Swaminathan R. Quality measures in pre-analytical phase of tissue processing: understanding its value in histopathology. J Clin Diagn Res. 2016 Jan;10(1):EC07–11. https://doi.org/10.7860/JCDR/2016/14546.7087
- Layfield LJ, Anderson GM. Specimen labeling errors in surgical pathology: an 18-month experience. Am J Clin Pathol. 2010 Sep;134(3):466–70. https://doi.org/10.1309/AJCPHLQHJ0S3DFJK
- Tabatabaee SS, Ghavami V, Kalhor R, Amerzadeh M, Zomorrodi-Niat H. Evaluation of errors related to surgical pathology specimens of different hospital departments with a patient safety approach: a case study in Iran. Patient Saf Surg. 2023 Apr;17(1):8. https://doi.org/10.1186/s13037-023-00360-1
- Jabarkhil AQ, Tabatabaee SS, Jamali J, Moghri J. Assessment of patient safety culture among doctors, nurses, and midwives in a public hospital in Afghanistan. Risk Manag Healthc Policy. 2021 Mar;14:1211–7. https://doi.org/10.2147/RMHP.S292193
- Morelli P, Porazzi E, Ruspini M, Restellit U, Banfi G. Analysis of errors in histology by root cause analysis: a pilot study. J Prev Med Hyg. 2014;54:90–6.
- Holstine JB, Samora JB. Reducing surgical specimen errors through multidisciplinary quality improvement. Jt Comm J Qual Patient Saf. 2021 Sep;47(9):563–71. https://doi.org/10.1016/j.jcjq.2021.04.003
- Steelman VM, Williams TL, Szekendi MK, Halverson AL, Dintzis SM, Pavkovic S. Surgical specimen management: a descriptive study of 648 adverse events and near misses. Arch Pathol Lab Med. 2016 Dec;140(12):1390–6. https://doi.org/10.5858/arpa.2016-0021-OA
- Kinlaw TS, Whiteside D. Surgical specimen management in the preanalytic phase: perioperative nursing implications. AORN J. 2019;110(3):237–50. https://doi.org/10.1002/aorn.12782
- Seferian EG, Jamal S, Clark K, Cirricione M, Burnes-Bolton L, Amin M, et al. A multidisciplinary, multifaceted improvement initiative to eliminate mislabelled laboratory specimens at a large tertiary care hospital. BMJ Qual Saf. 2014 Aug;23(8):690–7. https://doi.org/10.1136/bmjqs-2014-003005
- Sakorafas GH, Stafyla V, Kolettis T, Tolumis G, Kassaras G, Peros G. Microscopic papillary thyroid cancer as an incidental finding in patients treated surgically for presumably benign thyroid disease. J Postgrad Med. 2007;53(1):23–6. https://doi.org/10.4103/0022-3859.30323
- Rehman F, Haider MS, Bajwa R, Anwar MR, Sarwar MZ, Naumeri F, et al. Root cause analysis of pre-microscopic errors in anatomical pathology using Eindhoven classification. J Pak Med Assoc. 2020 Apr;70(4):687–93. https://doi.org/10.5455/JPMA.5565
