Original Article
VOLUME: 37 | ISSUE: 3 | Sep 25, 2021 | PAGE: (175 - 178) | DOI: 10.51441/BioMedica/5-501
Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa
Authors: Sheikh Qais Falah , Iram Bashir , Arshad Ali Marwat , Asif Shams
Article Info
Authors
Sheikh Qais Falah
Associate Professor, Department of Surgery, Gomal Medical College, Dera Ismail Khan- Pakistan.
Iram Bashir
Senior Registrar, Surgical Unit, Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan- Pakistan.
Arshad Ali Marwat
Professor of Surgery, Gomal Medical College, Dera Ismail Khan- Pakistan.
Asif Shams
Medical Officer, Surgical Unit, Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan- Pakistan.
Publication History
Received: June 19, 2021
Revised: August 21, 2021
Accepted: September 08, 2021
Published: September 25, 2021
Abstract
Background and Objective: Trucut biopsy (TCB) is a commonly used technique for histopathological diagnosis of a clinically and radiologically equivocal or suspicious breast mass. This study aimed to determine the sensitivity and specificity of TCB in the diagnosis of equivocal or suspicious breast masses at local tertiary care hospital in Khyber Pukhtunkhwa.
Methods: This descriptive cross-sectional study was conducted at the surgical unit of Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan, Pakistan. The study included 80 patients who presented with equivocal or suspicious breast masses from September, 2015 to December, 2020. The patients underwent TCB and after the histopathology report, they were followed by a definitive surgical procedure. The histopathology diagnosis following TCB was compared with the histopathology report of postsurgical specimen to determine the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TCB taking post-surgery histopathology as a gold standard for diagnosis.
Results: Out of the 80 patients, 68 (85%) were found to have a primary breast malignancy, while 12 (15%) patients were diagnosed with non-malignant lesions. There were only two false negative cases. The specificity and PPV of TCB were found to be 100%, while a sensitivity of 97% and a NPV of 85.7% was calculated.
Conclusion: TCB is a valid, reliable, and simple first line minimally invasive method to determine the diagnosis of breast masses that are clinically and radiologically (breast imaging-reporting and data system 3 to 5) equivocal or suspicious.
Keywords: Trucut biopsy; Breast mass; Equivocal; Phyllodes tumor; Breast carcinoma.
Pubmed Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams. Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa. BioMedica. 2021; 25 (September 2021): 175-178. doi:10.51441/BioMedica/5-501
Web Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams. Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa. https://biomedicapk.com/articles/online_first/501 [Access: July 03, 2024]. doi:10.51441/BioMedica/5-501
AMA (American Medical Association) Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams. Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa. BioMedica. 2021; 25 (September 2021): 175-178. doi:10.51441/BioMedica/5-501
Vancouver/ICMJE Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams. Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa. BioMedica. (2021), [cited July 03, 2024]; 25 (September 2021): 175-178. doi:10.51441/BioMedica/5-501
Harvard Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams (2021) Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa. BioMedica, 25 (September 2021): 175-178. doi:10.51441/BioMedica/5-501
Chicago Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams. "Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa." 25 (2021), 175-178. doi:10.51441/BioMedica/5-501
MLA (The Modern Language Association) Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams. "Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa." 25.September 2021 (2021), 175-178. Print. doi:10.51441/BioMedica/5-501
APA (American Psychological Association) Style
Sheikh Qais Falah, Iram Bashir, Arshad Ali Marwat, Asif Shams (2021) Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa. , 25 (September 2021), 175-178. doi:10.51441/BioMedica/5-501
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 37(3):175-178
ORIGINAL ARTICLE
Trucut biopsy as a first line diagnostic modality for equivocal or suspicious breast masses: an experience from a teaching hospital in Khyber Pukhtunkhwa
Sheikh Qais Falah1*, Iram Bashir2, Arshad Ali Marwat3, Asif Shams4
Received: 19 June 2021 Revised date: 21 August 2021 Accepted: 08 September 2021
Correspondence to: Sheikh Qais Falah
*Associate Professor, Department of Surgery, Gomal Medical College, Dera Ismail Khan, Pakistan.
Email: qaisfalah@hotmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Trucut biopsy (TCB) is a commonly used technique for histopathological diagnosis of a clinically and radiologically equivocal or suspicious breast mass. This study aimed to determine the sensitivity and specificity of TCB in the diagnosis of equivocal or suspicious breast masses at local tertiary care hospital in Khyber Pukhtunkhwa.
Methods:
This descriptive cross-sectional study was conducted at the surgical unit of Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan, Pakistan. The study included 80 patients who presented with equivocal or suspicious breast masses from September, 2015 to December, 2020. The patients underwent TCB and after the histopathology report, they were followed by a definitive surgical procedure. The histopathology diagnosis following TCB was compared with the histopathology report of postsurgical specimen to determine the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TCB taking post-surgery histopathology as a gold standard for diagnosis.
Results:
Out of the 80 patients, 68 (85%) were found to have a primary breast malignancy, while 12 (15%) patients were diagnosed with non-malignant lesions. There were only two false negative cases. The specificity and PPV of TCB were found to be 100%, while a sensitivity of 97% and a NPV of 85.7% was calculated.
Conclusion:
TCB is a valid, reliable, and simple first line minimally invasive method to determine the diagnosis of breast masses that are clinically and radiologically (breast imaging-reporting and data system 3 to 5) equivocal or suspicious.
Keywords:
Trucut biopsy, breast mass, equivocal, phyllodes tumor, breast carcinoma.
Introduction
Breast tissue is susceptible to various diseases ranging from inflammatory conditions or infections to benign and malignant neoplasms. Most of these conditions appear as a lump, and therefore it is imperative to have a good understanding of the anatomy, physiology, and pathology of breast tissue in order to differentiate benign lumps from potentially malignant ones.1
Breast cancer is the most common malignancy reported in females worldwide and accounts for 20%-30% of cancers reported worldwide. Incidence of breast cancer is alarmingly high in Pakistan with every one out of nine females affected.2 In fact, the incidence rate of breast cancer in Pakistan is one of the highest among Asian countries.2 As reported by Shaukat Khanum Memorial Cancer Hospital Lahore, breast cancer comprised 55.7% cases of malignancies in women in 2020.3 However, the developed countries in the west have seen an incredible downward trend in breast cancer mortality owing to the early and improved diagnosis and better treatment modalities.4
There are many methods to evaluate breast lumps with a specific, sensitive, efficient and cost-effective approach to diagnose breast malignancies. Physical examination, mammography, ultrasonography, thermography, fine needle aspiration cytology (FNAC), core needle biopsy (CNB) and excisional biopsy are all used to greater or lesser extent in the diagnosis of palpable breast mass.1 Owing to its simplicity, cost effectiveness, and efficiency, FNAC has been a method of choice for early diagnosis of the breast lumps along with mammograms and physical examination since a long time. However, it is extremely difficult to differentiate between invasive and non-invasive carcinomas, false negative results and insufficient samples.1
CNB, also known as trucut biopsy (TCB) is a useful method for histopathological diagnosis of a breast lump. The biopsy is done by inserting the needle into the breast mass by making a very small cut in overlying skin under local anesthesia. A biopsy specimen is obtained by means of four successive insertions with different angulations of the needle into the core of the lesion.4,5 The TCB is considered superior to FNAC of breast lesions as it provides sufficient tissue for pathologists to get reliable information about the histological type and prognostic parameters (receptor status, proliferative activity, ploidy, and expression of oncogenes and anti-oncogenes such as c-erbB-2 and p53).1 It thus provides useful information to both oncologists and surgeons regarding further management.1 Moreover, it is a less invasive procedure when compared to incisional and excisional biopsy and can be performed in an outpatient setting.1,6 TCB of breast mass should be preferred over FNAC whenever the mass appears clinically and radiologically [breast imaging-reporting and data system (BIRADS) score 3 to 5] equivocal or suspicious.7,8
The role of FNAC is debatable with respect to the CNB in the management of breast lesions. Some studies favor FNAC over CNB, while others are of the different opinion. Some authors also recommend combining the two techniques.9 The aim of this study was to determine the sensitivity and specificity of TCB in the diagnosis of equivocal or suspicious breast masses in female patients presenting at the tertiary care hospital of Khyber Pukhtunkhwa.
Methods
This descriptive cross-sectional study was conducted at the Surgery department of Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan, Pakistan from September 2015 to December 2020. Purposive sampling was used to recruit 80 patients with clinically and radiologically equivocal or suspicious breast masses (BIRADS score 3 to 5). The study was approved by the institutional ethical review committee. All patients who gave their written, informed consent were included in the study.
All patients were admitted to the surgical unit and routine workup was done. TCB was performed using a trucut gun with needles ranging from 14 guage (G) to 18 G. The biopsies were performed by consultant surgeons under local anesthesia using lignocaine. The biopsy specimens were sent for histopathological analyses and diagnosis on TCB was recorded.
The patients were reassessed for further surgical intervention and readmitted in the surgical unit for follow-up surgery. The breast mass removed during the surgery (like modified radical mastectomy, wide local excision and lumpectomy) was sent for post-surgical histopathology (PSH) according to recommended protocols.
The histopathology reports of TCB were then compared with the histopathological reports of the postsurgical specimens. The patients who did not undergo follow up procedure were excluded from the study. The TCB outcomes were classified as follows: True positive - both TCB and PSH had positive results for malignancy; True Negative - both TCB and PSH had negative results for malignancy; False Positive - TCB result was positive while that of PSH was negative and False Negative - TCB result was negative while that of PSH was positive.
Specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for the TCB as per standard formulas taking the post-surgery histopathology as gold standard for diagnosis.
Results
A total number of 80 patients having mean age of 47.7 +/- 10.92 years (range 30 to 80 years) were included in the study. Right breast was involved in 42 (52.5%) cases, while in 38 (47.5%) cases, left breast was involved.
Out of 80 patients, 66 (82.5%) were diagnosed as invasive ductal carcinoma, 2 (2.5%) were diagnosed with malignant phyllodes, 2 (2.5%) as benign phyllodes tumor, 10 patients (12.5%) had benign changes like fibrosis, adenosis and usual ductal hyperplasia. Thus, 68 biopsies (85%) showed malignant changes, while 12 (15%) were non-malignant (Figure 1).
The patients underwent follow up/definitive procedures like modified radical mastectomy, wide local excision or lumpectomy. The histopathology of the postsurgical specimen gave the same diagnosis as after TCB except for two cases. In these two cases, the histopathology following lumpectomy revealed invasive ductal carcinoma instead of benign changes suggested by TCB report. Thus, there were two false negative results while there was no false positive (Table 1).
The sensitivity of TCB in diagnosing malignant lesions was 97%, while specificity was 100%. The PPV was 100% and the NPV was 85.7%.
Discussion
In the present study, the sensitivity of TCB in diagnosing malignant conditions was 97%, while specificity was 100%. These results are comparable to results by Shashirekha et al.1 (97.1% and 100%), Rikabi et al.5 (95.1% and 100%), Altintas et al.7 (95.4% and 100%), and Samantara et al.10 (97%). Another local study by Nisar et al.11 conducted at a tertiary hospital of Khyber Pukhtunkhwa showed sensitivity of 81.48% for TCB in the diagnosis of malignant lesions that is far too low as compared to the present study and other international studies. There were only two false negative cases in the present study that were apparently due to sampling error.
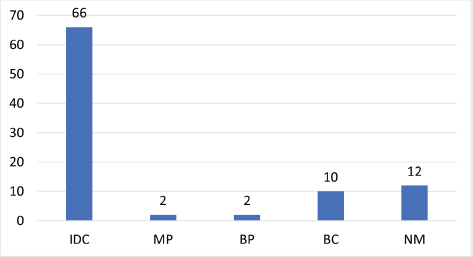
Figure 1. Breast lesions identified on trucut biopsy. IDC = Invasive ductal carcinoma; MP = Malignant phyllodes; BP = Benign phyllodes; BC = Benign changes; NM = Non-malignant.
Table 1. TCB and PSH results (n = 80).
| TCB + | TCB - | Total | |
|---|---|---|---|
| PSH + | 66 (82.5%) | 2 (2.5%) | 68 (85%) |
| PSH - | 0 | 12 (15%) | 12 (15%) |
| Total | 66 (82.5%) | 14 (17.5%) | 80 (100%) |
In a study conducted by Kurita et al.12 on the roles of FNAC and CNB in diagnosing breast cancers, they found no significant difference between the absolute sensitivity of FNAC alone (93%) and CNB alone (86%). Moreover, they observed that in cases where fine needle aspiration produced inadequate smears, CNB alone and FNAC alone demonstrated sensitivity of 63% and 42%, respectively, while their combination significantly improved the sensitivity to 72% (p < 0.05). Thus Kurita et al.12 concluded that FNAC and CNB should be considered complimentary to each other. Rikabi et al.5 on the other hand, there are certain studies that advocate use of TCB as the initial investigative method of first choice for preoperative diagnosis of breast lesions. Altintas et al.7 highlighted the importance of TCB in the evaluation of suspected breast lesions. In the present study, TCB was taken (as an initial test for tissue diagnosis) from selected cases of breast mass that were clinically and radiologically equivocal or suspicious.
Samantary et al.10 suggested that TCB should be performed by experienced surgeons so that the biopsy is taken from proper site. In the present study, the TCB in all the patients was performed by the senior and experienced consultants.
The trucut needles used in our study were 14 G, 16 G, or 18 G in size, depending on the mass and size of breast. Different surgeons have used biopsy needles of different sizes ranging from 14 G to 18 G with comparable results in various studies. Shashirekha et al.1, Rikabi et al.5 and Altintas et al.7 used narrow bore 18 G needle to prevent massive displacement and minimize bleeding during biopsy, whereas Samantary et al.10 used a 14 G needle as it produces higher quality, more intact cores and improved accuracy of diagnosis without increasing the morbidity. There were no procedure related complications during or following TCB in the study cases.
Conclusion
TCB is a sensitive and highly specific procedure to obtain the tissue diagnosis of breast masses. Being minimally invasive and with a good feasibility in performing, TCB may be used as a first-line diagnostic modality in all those breast masses that are clinically and radiologically (BIRADS 3 to 5) equivocal or suspicious.
Limitations of the study
The data is limited to a single center. Comparison with FNAC could be included for a better ascertainment of the two minimally invasive investigative modalities.
Acknowledgement
The authors would like to thank the staff members of Mufti Mehmood Memorial Teaching Hospital (MMMTH), Dera Ismail Khan, Pakistan for their cooperation in the data collection.
List of Abbreviations
| BIRADS | Breast imaging-reporting and data system |
| CNB | Core needle biopsy |
| FNAC | Fine needle aspiration cytology |
| G | Guage |
| MMMTH | Mufti Mehmood Memorial Teaching Hospital |
| NPV | Negative predictive value |
| PPV | Positive predictive value |
| TCB | Trucut biopsy |
Conflict of interest
None to declare.
Grant support & financial disclosure
None to disclose.
Ethical approval
The study was approved by the ethical review committee of Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan, Pakistan vide Reference No. 171/AD/Research/GMC dated 27/07/2021.
Author’s contribution
SQF: Conception and design of the study, critical analysis with intellectual input, review of literature, analysis and interpretation of data, drafting the manuscript.
IB: Data Collection, Analysis and interpretation of data.
AAM, AS: Data collection, review of literature.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Author details
Sheikh Qais Falah1, Iram Bashir2, Arshad Ali Marwat3, Asif Shams4
- Associate Professor, Department of Surgery, Gomal Medical College, Dera Ismail Khan, Pakistan
- Senior Registrar, Surgical Unit, Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan, Pakistan
- Professor of Surgery, Gomal Medical College, Dera Ismail Khan, Pakistan
- Medical Officer, Surgical Unit, Mufti Mehmood Memorial Teaching Hospital, Dera Ismail Khan, Pakistan
References
- Shashirekha CA, Rahul SR, Ravikiran HR, Sreeramulu PN, Krishna P. Fine needle aspiration cytology versus trucut biopsy in the diagnosis of breast cancer: a comparative study. Int Surg J. 2017;4(11):3718. https://doi.org/10.18203/2349-2902.isj20174893
- Zaheer S, Shah N, Maqbool SA, Soomro NM. Estimates of past and future time trends in age specific breast cancer incidence among women in Karachi, Pakistan: 2004 - 2025. BMC Public Health. 2019;19:1001. https://doi.org/10.1186/s12889-019-7330-z
- Mahmood S, Faraz R, Yousaf A, Quader AU, Asif H, Atif A, et al. Annual cancer registry report - 2020: Shaukat Khanum Memorial Cancer Hospital & Research Center, Pakistan [Internet] [cited 2021 Sep]. Available from: https://shaukatkhanum.org.pk/health-care-professionals-researchers/cancer-statistics/skm-cancer-registry/
- Carioli G, Malvezzi M, Rodriguez T, Bertuccio P, Negri E, La Vecchia C. Trends and predictions to 2020 in breast cancer mortality in Europe. Breast. 2017;36(7):89–95. https://doi.org/10.1016/j.breast.2017.06.003
- Rikabi A, Hussain S. Diagnostic usefulness of tru-cut biopsy in the diagnosis of breast lesions. Oman Med J. 2013;28 (2):125. https://doi.org/10.5001/omj.2013.32
- Joulaee A, Kalantari M, Kadivar M, Joulaee S, Bahrani N, Mangual M, et al. Trucut biopsy of breast lesions: the first step toward international standards in developing countries. Eur J Cancer. 2012;48(5):648–54. https://doi.org/10.1016/j.ejca.2011.11.038
- Altintas Y, Bayrak M. Diagnostic utility of tru-cut biopsy in the assessment of breast lesions. Ann Med Res. 2019;26 (3):505–9. https://doi.org/10.5455/annalsmedres.2019.02.077
- Hashemzadeh SH, Kumar PV, Malekpour N, Hashemi Z, Fatahi F, Malekpour F. Diagnostic accuracy of fine needle aspiration cytology: comparison of results in Tabriz Imam Khomeini Hospital and Shiraz University of Medical Sciences. Iran J Cancer Prev. 2009;2:133–6.
- Mitra S, Dey P. Fine-needle aspiration and core biopsy in the diagnosis of breast lesions: a comparison and review of the literature. Cytojournal. 2016;13(4):18. https://doi.org/10.4103/1742-6413.189637
- Samantaray S, Panda N, Besra K, Pattanayak L, Samantara S, Dash S. Utility of tru-cut biopsy of breast lesions-an experience in a regional cancer center of a developing country. J Clin diagnostic Res. 2017;11(3):36–9. https://doi.org/10.7860/JCDR/2017/23572.9548
- Nisar S, Amin A, Iqbal Z, Tauseefuddin M, Sharif G. Sensitivity of fine needle aspiration vs core biopsy in the diagnosis of palpable breast lesions. Ophthalmol Update. 2016;14(3):71–3
- Kurita T, Tsuchiya S, Watarai Y, Yamamoto Y, Harada O, Yanagihara K, et al. Roles of fine-needle aspiration and core needle biopsy in the diagnosis of breast cancer. Breast Cancer. 2012;19(1):23–9. https://doi.org/10.1007/s12282-010-0251-4
