Original Article
VOLUME: 38 | ISSUE: 1 | Mar 30, 2022 | PAGE: (10 - 17) | DOI: 10.51441/BioMedica/5-593
Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard
Authors: Mariam Saeed Kalim , Arslan Ahmed , Waseem Sadiq Awan , Saulat Sarfraz
Article Info
Authors
Mariam Saeed Kalim
Department of Radiology, Mayo Hospital, Lahore, Pakistan
Arslan Ahmed
Department of Surgery, Sir Ganga Ram Hospital, Lahore, Pakistan
Waseem Sadiq Awan
Chairman, Department of Surgery and Allied, Sargodha Medical College, Sargodha, Pakistan
Saulat Sarfraz
Department of Radiology, Sheikh Zayed Postgraduate Medical Institute, Lahore, Pakistan
Publication History
Received: December 21, 2021
Revised: February 17, 2022
Accepted: March 10, 2022
Published: March 30, 2022
Abstract
Background and objective: Breast cancer is the most common malignancy in females. Early diagnosis can help in reducing the morbidity and mortality associated with this disease. Sonoelastography has shown to be a valuable tool in early detection of breast cancer. The aim of the study was to evaluate the diagnostic accuracy of combining sonoelastography with mammography in diagnosing malignant solid breast lesions taking histopathology as a gold standard.
Methods: A descriptive cross-sectional study was carried out at the Department of Radiology, Shaikh Zayed Medical Complex/Federal Post-Gradaute Medical Institute (FPGMI), Lahore, Pakistan during six months period from 1st September, 2018 to 31st March, 2019. Female patients > 35 years of age and presenting with suspected malignant breast masses were included. Mammography and sonoelastography of the lesions were done. Finally, the patients were referred for tru cut biopsy. Diagnostic accuracy was calculated for mammography, sonoelastography and their combination.
Results: A total of 200 female patients were enrolled with a mean age of 50.8 (± 8.6) years. Mammographic findings suggestive of malignancy (BI-RADS category IV and V) were present in 96 (48%) cases. Elastography showed finding of malignancy (Score 4 and 5) in 96 (48%) cases. Combined sonoelastography and mammography diagnosed malignancy in 112 (56%) cases. Histopathologically confirmed malignancy was seen in 110 (55%) cases. The sensitivity and specificity of mammography (76.3 % and 77.7%) and sonoelastography (77.3% and 87.7%), were comparable. The combination of mammography and sonoelastography showed a higher sensitivity (90.9%) and specificity (86.6%). The combination showed a diagnostic accuracy of 89% followed by sonoelastography (82%) and mammography (77%) alone.
Conclusion: Combination of sonoelastography and mammography can significantly enhance the diagnostic accuracy of breast carcinoma. Females may be offered mammography or ultrasonography in combination with sonoelastography for routine testing.
Keywords: Sonoelastography, breast carcinoma, mammography, ultrasonography, diagnostic accuracy.
Pubmed Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz. Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard. BioMedica. 2022; 30 (March 2022): 10-17. doi:10.51441/BioMedica/5-593
Web Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz. Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard. https://biomedicapk.com/articles/online_first/593 [Access: July 03, 2024]. doi:10.51441/BioMedica/5-593
AMA (American Medical Association) Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz. Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard. BioMedica. 2022; 30 (March 2022): 10-17. doi:10.51441/BioMedica/5-593
Vancouver/ICMJE Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz. Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard. BioMedica. (2022), [cited July 03, 2024]; 30 (March 2022): 10-17. doi:10.51441/BioMedica/5-593
Harvard Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz (2022) Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard. BioMedica, 30 (March 2022): 10-17. doi:10.51441/BioMedica/5-593
Chicago Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz. "Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard." 30 (2022), 10-17. doi:10.51441/BioMedica/5-593
MLA (The Modern Language Association) Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz. "Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard." 30.March 2022 (2022), 10-17. Print. doi:10.51441/BioMedica/5-593
APA (American Psychological Association) Style
Mariam Saeed Kalim, Arslan Ahmed, Waseem Sadiq Awan, Saulat Sarfraz (2022) Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard. , 30 (March 2022), 10-17. doi:10.51441/BioMedica/5-593
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(1):10-17
ORIGINAL ARTICLE
Diagnostic Accuracy of Combining Sonoelastography with Mammography in Solid Breast Lesions Keeping Histopathology as Gold Standard
Mariam Saeed Kalim1, Arslan Ahmed2, Waseem Sadiq Awan3. Saulat Sarfraz4
Received: 21 December 2021 Revised date: 17 February 2022 Accepted: 10 March 2022
Correspondence to: Dr. Arslan Ahmed
Senior Registrar, Department of Surgery, Sir Ganga Ram Hospital, Lahore, Pakistan.
Email: drarslanahmed@outlook.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and objective:
Breast cancer is the most common malignancy in females. Early diagnosis can help in reducing the morbidity and mortality associated with this disease. Sonoelastography has shown to be a valuable tool in early detection of breast cancer. The aim of the study was to evaluate the diagnostic accuracy of combining sonoelastography with mammography in diagnosing malignant solid breast lesions taking histopathology as a gold standard.
Methods:
A descriptive cross-sectional study was carried out at the Department of Radiology, Shaikh Zayed Medical Complex/Federal Post-Gradaute Medical Institute (FPGMI), Lahore, Pakistan during six months period from 1st September, 2018 to 31st March, 2019. Female patients > 35 years of age and presenting with suspected malignant breast masses were included. Mammography and sonoelastography of the lesions were done. Finally, the patients were referred for tru cut biopsy. Diagnostic accuracy was calculated for mammography, sonoelastography and their combination.
Results:
A total of 200 female patients were enrolled with a mean age of 50.8 (± 8.6) years. Mammographic findings suggestive of malignancy (BI-RADS category IV and V) were present in 96 (48%) cases. Elastography showed finding of malignancy (Score 4 and 5) in 96 (48%) cases. Combined sonoelastography and mammography diagnosed malignancy in 112 (56%) cases. Histopathologically confirmed malignancy was seen in 110 (55%) cases. The sensitivity and specificity of mammography (76.3 % and 77.7%) and sonoelastography (77.3% and 87.7%), were comparable. The combination of mammography and sonoelastography showed a higher sensitivity (90.9%) and specificity (86.6%). The combination showed a diagnostic accuracy of 89% followed by sonoelastography (82%) and mammography (77%) alone.
Conclusion:
Combination of sonoelastography and mammography can significantly enhance the diagnostic accuracy of breast carcinoma. Females may be offered mammography or ultrasonography in combination with sonoelastography for routine testing.
Keywords:
Sonoelastography, Breast carcinoma, mammography, ultrasonography, diagnostic accuracy.
Introduction
Breast cancer is the most common malignancy in females. It accounts for almost 25% of new cancer cases in females and 15% of the cancer related deaths worldwide.1 It leads to more than 600,000 death annually.2 As per the GLOBOCAN Cancer Tomorrow prediction tool the incidence of breast cancer is expected to rise by more than 46% by the year 2040.3 High incidence of obesity, tobacco exposure, physical inactivity, high fat diet, late age at first pregnancy, increased use of hormonal therapies and oral contraceptives are the main contributing factors for the rise in the incidence of breast cancer.4
Early detection of breast cancer can prevent significant morbidity and mortality associated with this condition. The common radiological evaluating methods include mammography, ultrasonography and sonoelastography. Breast sonoelastography is an emerging technique that helps in assessment of breast deformability by measurement of breast tissue elasticity.5 The World Federation of Ultrasound in Medicine and Biology (WFUMB) has recommended the addition of sonoelastography to other radiological modalities available for the diagnosis of breast lesions.6
Conventional mammography is primary imaging modality with a sensitivity of 71% and specificity of 75% in detecting breast lesions.7 Ultrasonography is widely used due to its availability and its usefulness particularly in younger patients with dense breast tissue. The sensitivity and specificity of ultrasonography for detecting breast lesions is 80% and 88%, respectively.8 Sonoelastography gives better details of the epithelial and connective tissue components based on elasticity, which is property of material to reform back to its original position after stress is removed. The strain ratio is higher for stiffer/malignant lesions and lower for softer/benign lesions.9 In one of the local studies conducted in Combined Military Hospital (CMH), Rawalpindi, Pakistan, using a strain ratio cut-off of 4.8, a high sensitivity and specificity of 88.6% and 90.2%, respectively, was achieved for sonoelastography.10 Thus, the use of sonoelastography in our population may be recommended. Although it may be used independently, but the addition of sonoelastography to the already existing mammography protocol can significantly enhance the diagnostic capabilities.11
Currently, routine use of sonoelastography is not widely practiced in Pakistan. Although literature exists but more local evidence is required to thoroughly understand the utility of sonoelastography in our population. This may be particularly useful in case of indiscriminate lesions where sonoelastography can complement other modalities and provide better identification of lesions. This study was, therefore, designed with the aim to evaluate the diagnostic accuracy of combining sonoelastography with mammography in differentiating benign from malignant solid breast lesions taking histopathology as gold standard.
Methods
A descriptive cross-sectional study was carried out at the Department of Radiology, Shaikh Zayed Medical Complex/Federal Post-Graduate Medical Institute (FPGMI), Lahore, during six months period from 1st September, 2018 to 31st March, 2019. Ethical approval was taken from the Institutional Review Board (IRB) of FPGMI, Sheikh Zayed Medical Complex (IRB # 1537, dated 01/08/2018). The study population included female patients more than 35 years of age and presenting with either breast lumps that on examination were suspected to be malignant or skin changes such as dimpling, peude orange appearance, nipple retraction or those with strong family history and were referred to the radiology department for further work-up. A non-probability consecutive sampling technique was used and 200 cases presenting during the study period and fulfilling the inclusion criteria were included. Lactating and pregnant females, patients with palpable chest wall lesions and those refusing biopsy or not providing consent for the study were excluded. Informed consent was taken from all the participants. Mammography was performed using MAMMOMAT (Siemens electronics) with full field film-screen digital imaging system and two standard views in craniocaudal (CC) projection and mediolateral oblique (MLO) projections were taken. Breast Imaging-Reporting and Data System (BI-RADS) was used to classify lesions. BI-RADS category IV and V were regarded as malignant. All mammographic patients wore thyroid collar shielding around the neck.
Sonoelastography images were obtained using LOGIQ S7 EXPERT (GE Healthcare, Pittsburgh, PA, USA) with a 7.5 MHz linear transducer. Scanning was performed both in longitudinal and transverse planes first in B mode and then further acquisition of images with strain wave elastography. A chromatic scale was used to assign soft tissues, which can be compressed/strained, “green color” and hard tissues, which are not compressible, “blue color”. Tsukuba University Scoring System12, that defines a lesion according to the color variation during compression in the region, was used to further categorize the lesions. A score of 1 to 3 were considered “benign” and a score of 4 and 5 was regarded as “malignant”. Finally, the patients were referred for true cut biopsy. For biopsy conformation of the lesion, core needle biopsy was performed using 14G needle with 20mm cutting length.
Statistical Analysis
The data were entered into SPSS version 23.0 and was analyzed using its statistical package. Descriptive statistics were performed and presented as mean (±S.D) for quantitative variables and frequency and percentages for qualitative variables. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy were calculated using 2 x 2 tables. All the data were entered in to predesigned proforma and confidentiality of the data was maintained.
Results
During the study period of six months, 200 female patients with suspicion of malignant breast lesions were enrolled in the study. The age characteristics of the patients are given in Table I. Mammography results showed that highest number of patients belonged to of BI-RADS category II (29.5%), followed by category V (29%), category III (20%), category IV (19%) and category I (2.5%). The BI-RADS and sonoelastography characteristic of the patients are given in Table-1.
Mammographic findings suggestive of malignancy (BI-RADS category IV and V) were present in 96 (48%) cases. Elastography showed finding of malignancy (Score 4 and 5) in 96 (48%) cases. Combined sonoelastography and mammography diagnosed malignancy in 112 (56%) cases. Histopathologically confirmed malignancy was present in 110 (55%) cases. Figure 1 shows results of sonoelastography in various patients with breast lesions. Table-2 shows the modality-wise diagnosis of all the patients.
Table 1: Baseline characteristics of the study participants (n=200)
| Age (years) | Mean (± S.D) | Minimum | Maximum |
| 50.8 (± 8.6) | 35 | 70 | |
| Age Groups | Age (years) | No. of Patients (n) | Percentage (%) |
| 35-55 | 132 | 66% | |
| 56-65 | 64 | 32% | |
| >65 | 4 | 2% | |
| Total | 200 | 100 | |
| BI-RADS Category | Category | No. of Patients (n) | Percentage (%) |
| I | 5 | 2.5% | |
| II | 59 | 29.5% | |
| III | 40 | 20% | |
| IV | 38 | 19% | |
| V | 58 | 29% | |
| Total | 200 | 100% | |
| SONOELASTOGRAPHY SCORE | Category | No. of Patients (n) | Percentage (%) |
| SCORE 1: | 58 | 29% | |
| SCORE 2: | 20 | 10% | |
| SCORE 3: | 26 | 13% | |
| SCORE 4: | 52 | 26% | |
| SCORE 5: | 44 | 22% | |
| Total | 200 | 100% |
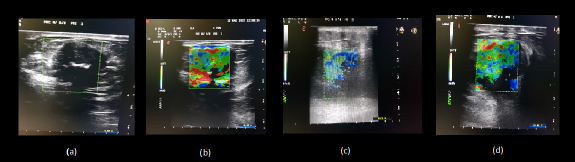
Figure 1. Sonoelastographic images of breast lesions showing, (a) & (b); a benign fibroadenoma with sonoelastography score of 2; red color coding signifies soft benign lesion (c); borderline intermix lesion with score of 3 and (d); a confirmed malignant lesion with sonoelastography score of 5.
Results from the histopathological examination of biopsy sample showed that 90 (45%) cases had benign pathology of which fibroadenoma (39%) was the most common. Among the malignant cases the most common pathology was invasive ductal carcinoma which was present in 95 (47.5%) cases. Table-3 shows the common pathologies diagnosed on histopathology.
Diagnostic accuracy of mammography, sonoelastography and combination was studied against the gold standard histopathology. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of mammography were 76.3%, 77.7%, 87.5% and 67.3%, respectively. The sensitivity, specificity, PPV and NPV of sonoelastography were 77.3%, 87.7%, 88.5% and 76%, respectively. The combination of mammography and sonoelastography showed a higher sensitivity, specificity, PPV and NPV of 90.9%, 86.6%, 89.3% and 88.6%, respectively. The diagnostic accuracy was highest in the combination of mammography and sonoelastography as compared to mammography and sonoelastography alone. The combination showed a diagnostic accuracy of 89% followed by 82% for sonoelastography and 77% for mammography. Table 4-6 show the diagnostic accuracy of the diagnostic modalities in patients with suspicious breast lumps.
Table 2: Modality-wise diagnosis of patients with breast lumps (n=200)
| Mammography diagnosis | Category | No. of Patients (n) | Percentages (%) |
| Benign | 104 | 52% | |
| Malignant | 96 | 48% | |
| Total | 200 | 100% | |
| Sonoelastography Diagnosis | Category | No. of Patients (n) | Percentages (%) |
| Benign | 104 | 52% | |
| Malignant | 96 | 48% | |
| Total | 200 | 100% | |
| Sonoelastography + Mammography Diagnosis | Category | No. of Patients (n) | Percentages (%) |
| Benign | 88 | 44% | |
| Malignant | 112 | 56% | |
| Total | 200 | 100 | |
| Histopathology Diagnosis | Category | No. of Patients (n) | Percentages (%) |
| Benign | 90 | 45% | |
| Malignant | 110 | 55% | |
| Total | 200 | 100 |
Table 3: Histopathological diagnosis of the patients with breast lumps (n=200)
| Diagnosis | No. of Patients (n) | Percentages (%) |
|---|---|---|
| Benign Breast Lesions | ||
| Fibroadenoma | 78 | 39% |
| Ductal Papilloma | 4 | 2% |
| Lipoma | 2 | 1% |
| Gynaecomastia | 2 | 1% |
| Mastitis | 2 | 1% |
| Granulomatous Mastitis | 2 | 1% |
| Total | 90 | 45% |
| Malignant Breast Masses | ||
| Invasive Ductal Adenocarcinoma | 95 | 47.5% |
| Lobular carcinoma | 6 | 3% |
| Medullary Carcinoma | 5 | 2.5% |
| Intra-ductal papillary carcinoma | 4 | 2% |
| Total | 110 | 55% |
Discussion
The results from the current study show that the mean age of patients was 50.8 (±8.6) years with age range from 35 to 70 years. The majority of the patients were between 35-55 years of age (66%). In a study conducted on Pakistani population, the mean age of patients was 38.20 (±10.63) years. The majority of the patients who had malignancy belonged to the 50-60 years age group.10 Similarly, studies from India, South Korea and Japan have shown that the incidence of breast cancer peaks in the fifth and sixth decade of life.13-15 A study from Srilanka reported breast cancer peak in even higher age group of 60-65 years.16 Increasing age is a well-known risk factor for developing breast cancer. As per Pike’s model, breast tissue ageing is associated with increased cumulative exposure to growth factors, hormones and carcinogens.17. In the current study the peak age group was 35-55 years, which is younger than that quoted in most of the studies from around the world. Literature is evident that recently much younger age groups are presenting with breast cancer in Pakistan due to rapid urbanization, western diets, inactivity and increased incidence of smoking.18
Table 4: Diagnostic accuracy of Mammography taking histopathology as gold standard (n = 200)
| Histopathology Diagnosis Cross-tabulation | ||||
|---|---|---|---|---|
| Malignant | Benign | Total | ||
| Mammographic Diagnosis | Malignant | 84 (TP) | 20 (FP) | 96 |
| Benign | 26 (FN) | 70 (TN) | 104 | |
| Total | 110 | 90 | 200 | |
Table 5: Diagnostic accuracy of Sonoelastography taking histopathology as gold standard (n = 200)
| Histopathology Diagnosis Cross-tabulation | |||||
|---|---|---|---|---|---|
| Malignant | Benign | Total | |||
| Sonoelastography Diagnosis | Malignant | 85 (TP) | 11 (FP) | 96 | |
| Benign | 25 (FN) | 79 (TN) | 104 | ||
| Total | 110 | 90 | 200 | ||
Table 6: Diagnostic accuracy of combined Mammography + Elastography taking histopathology as gold standard (n = 200)
| Histopathology Diagnosis Cross-tabulation | ||||
|---|---|---|---|---|
| Malignant | Benign | Total | ||
| Mammography + Elastography Diagnosis | Malignant | 100 (TP) | 12 (FP) | 112 |
| Benign | 10 (FN) | 78 (TN) | 88 | |
| Total | 110 | 90 | 200 | |
Table 7: Diagnostic accuracy of Mammography, Sonoelastography and Combination in diagnosing
malignant breast lesions taking histopathology as gold standard (n = 200)
| Parameters | Mammography | Elastography | Mammography + Sonoelastography |
|---|---|---|---|
| Sensitivity | 76.3 % | 77.3% | 90.9% |
| Specificity | 77.7% | 87.7% | 86.6% |
| PPV | 87.5% | 88.5% | 89.3% |
| NPV | 67.3% | 76% | 88.6% |
| Diagnostic Accuracy | 77% | 82% | 89% |
In the present study the results from the histopathological analysis showed that 45% of the tumors were benign and 55% were malignant. Fibroadenoma was the most common benign pathology and invasive ductal carcinoma was the most common malignancy. In one of the recent local studies conducted on the population of Lahore, Pakistan, fibroadenoma was the most common benign lesion which occurred in more than 50% of the cases. This was followed by fibrocystic disease, breast abscess, granulomatous disease, lipoma and phylloides tumor.19 A similar study from India also showed that fibroadenoma was most common benign condition (66.7%). This was followed by fibroadenosis, breast abscess and mastitis.20 The study population of the current study only comprised of patients with clinically suspicious breast lumps. Therefore conditions like breast abscess, mastitis and lipoma were not included. Nevertheless, fibroadenoma, due to its discrete lump appearance which may resemble malignancy clinically, was referred for histopathology. This is the reason why fibroadenoma was solely the most common benign condition observed in the present study.
Among the malignant condition, invasive ductal carcinoma was the most common malignancy which occurred in 47.5% of all the cases. When considering the malignant cases only, invasive ductal carcinoma was present in more than 86% of the cases, whereas, lobular, medullary and intraductal papillary carcinoma occurred in 3%, 2.5% and 2%, respectively. A review of literature shows that invasive ductal carcinoma is indeed the most common malignancy of breast.21,22 In a study conducted in King Abdul Aziz Hospital in Riyadh, Saudi Arabia, ductal carcinoma was most common (85%) breast malignancy followed by lobular carcinoma (11%).21 A study done in Muzaffarabad, Azad Kashmir, showed that in women with clinically palpable breast lumps, 35% were malignant. Among the malignant cases 95% were invasive ductal carcinoma.22 In the present study, the percentage of malignancy appears higher than the studies quoted above due to the reasons pertaining to the inclusion criteria, as already mentioned earlier. However, among those with malignancy, the results are consistent with most of the studies mentioned in literature.
The results on the diagnostic accuracy of mammography, sonoelastography and the combination showed that the combination had a higher diagnostic accuracy for labeling breast carcinoma. The diagnostic accuracy for the combination was 89% followed by 82% for sonoelastography and 77% for mammography alone. The sensitivity of the combination was markedly increased; however, the specificity was lower than that of elastography alone. In one study conducted in China on eighty nine females with breast lesions, the combination of sonoelastography and mammography showed a high sensitivity of 95.5% and specificity of 94.6%. This was considerably higher than either of the modalities alone and thus it was concluded that compared to the mono detection of either technique, the combination has a superior diagnostic accuracy.23 A study conducted in Romania showed that sonoelastography, when added to mammography, enhanced the detection of smaller lesion which were 17.9% more likely to be missed on mammography alone. Thus the study concluded that elastography can provide value addition to mammography for breast cancer detection.24
Mammography is a widely used screening tool for detection of breast cancer. It has a good diagnostic accuracy for breast lesions. Studies have shown that some limitations such as poor image quality, inappropriate reporting, breast positioning, quality control and equipment related issues, particularly in older analog machines, can adversely affect the accuracy.25,26 Sonoelastography provides information on tissue elasticity, which when combined morphological findings of mammography can lead to enhanced detection of breast cancer.27 In a study conducted at Baskent University Hospital, Turkey showed that the diagnostic accuracy of the combination of sonoelastography and mammography was higher but the specificity was similar to elastography alone.28 The present study has shown similar trends in which the specificity of combination is lower than that of elastography. Sonoelastography is operator dependent and subjective assessment of diverse sonoelastographic images can be a possible limitation for any ultrasonographer. Additionally various brands of sonoelastographic devices can have different cutoff values. These limitations may count towards the difference observed in various studies.29 Nevertheless, results from studies mentioned above show that literature is evident in support of the combined use of sonoelastography with either ultrasound of mammography. Further research in this area can help in formulating local and regional guidelines for screening and diagnosis of breast cancer in our part of the world.
Conclusion
Early and accurate diagnosis of breast cancer can reduce the morbidity and mortality.Results from this study show that addition of sonoelastography to mammography can significantly enhance the diagnostic capabilities of mammography. Thus it is recommended to complement mammography or ultrasonography with sonoelastography in routine breast screening in order to improve the diagnostic accuracy and thus the clinical outcome for the patient.
Limitations of the study
The study is a single center study. A multi centric study involving various cities of Pakistan may provide more generalizability to the result. Additionally, the inclusion criteria of the study included clinically suspicious nodules. Impalpable lumps and locally advanced conditions were excluded. Inclusion of these cases may provide a better depiction of the role of sonoelastography in various types of breast lumps.
List of Abbreviations
| BI-RADS | Breast Imaging-Reporting and Data System |
| CC | Cranio-caudal |
| GLOBOCAN | Global Cancer Observatory |
| IRB | Institutional Review Board |
| MLO | Mediolateral oblique |
| NPV | Negative predictive value |
| PPV | Positive predictive value |
| SD | Standard deviation |
| SPSS | Statistical Package for the Social Sciences |
| WFUMB | World Federation of Ultrasound in Medicine and Biology |
Acknowledgement
The authors would like to acknowledge the staff of the Department of Radiology, Shaikh Zayed Medical Complex/Federal Post-Graduate Medical Institute (FPGMI), Lahore, Pakistan for their logistic and technical support in acquisition of data related to this study. We would also like to acknowledge all those patients whose data was collected with their informed consent.
Ethical approval
The study was approved by the Institutional Ethical Review Board of Federal Post-Graduate Medical Institute (FPGMI), Sheikh Zayed Medical Complex, Lahore Pakistan vide Letter No.IRB # 1537-2018 dated 01/08/2018.
Conflict of interest
None to declare
Grant Support and Financial disclosure
None to disclose
Authors’ Contribution
MSK: Concept of study, acquisition of data and drafting of manuscript.
AA: Acquisition and analysis of data, important intellectual input, drafting of manuscript.
WSA: Acquisition of data, important intellectual input.
SS: Concept and design of study, supervision of data collection and analysis.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin. 2018;68(6):394-424. https://doi.org/10.3322/caac.21492.
- Lei S, Zheng R, Zhang S, Wang S, Chen R, Sun K, et al. Global patterns of breast cancer incidence and mortality: A population‐based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021;41(11):1183-94. https://doi.org/10.1002/cac2.12207.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin. 2021;71(3):209-49. https://doi.org/10.3322/caac.21660.
- Britt KL, Cuzick J, Phillips KA. Key steps for effective breast cancer prevention. Nat Rev Cancer. 2020; 20(8): 417-36. https://doi.org/10.1038/s41568-020-0266-x.
- Mesurolle B, El Khoury M, Chammings F, Zhang M, Sun S. Breast sonoelastography: now and in the future. Diagn Interv Imaging. 2019;100(10):567-77. https://doi.org/10.1016/j.diii.2019.03.009.
- Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol. 2015;41(5):1148-60. https://doi.org/10.1016/j.ultrasmedbio.2015.03.009.
- Zhang Y, Ren H. Meta-analysis of diagnostic accuracy of magnetic resonance imaging and mammography for breast cancer. J Cancer Res Ther. 2017;13(5):862. https://doi.org/10.4103/jcrt.JCRT_678_17.
- Sood R, Rositch AF, Shakoor D, Ambinder E, Pool KL, Pollack E, et al. Ultrasound for breast cancer detection globally: a systematic review and meta-analysis. J Glob Oncol. 2019;5:1-7. https://doi.org/10.1200/JGO.19.00127.
- Hahn S, Lee YH, Lee SH, Suh JS. Value of the strain ratio on ultrasonic elastography for differentiation of benign and malignant soft tissue tumors. J Ultrasound Med. 2017;36(1):121-7. https://doi.org/10.7863/ultra.16.01054.
- Rehman H, Raza S, Aziz S, Ahmad AM, Tahir S. Diagnostic accuracy of sonoelastography in the non-invasive diagnosis of malignant breast cancer compared to histopathology as a gold standard. J Coll Phys Surgeons. 2017;27(5):267-70. https://doi.org/2609. PMID: 28599685.
- Rathore P, Rastogi R, Pratap V, Soni S. Comparative role of x-ray mammography and sonography with sonoelastography in palpable breast lesions. Ann Int Med Dent Res. 2018;4(3):10. https://doi.org/10.21276/aimdr.2018.4.3.RD2.
- Schwab F, Redling K, Siebert M, Schötzau A, Schoenenberger CA, Zanetti-Dällenbach R. Inter-and intra-observer agreement in ultrasound BI-RADS classification and real-time elastography Tsukuba score assessment of breast lesions. Ultrasound Med Biol. 2016;42(11):2622-29. https://doi.org/10.1016/j.ultrasmedbio.2016.06.017.
- Mathew A, George P, Arjunan A, Augustine P, Kalavathy MC, Padmakumari G, et al. Temporal trends and future prediction of breast cancer incidence across age groups in Trivandrum, South India. Asian Pac J Cancer Prev. 2016;17(6):2895-99. https://doi.org/APJCP.2016.17.6.2895.
- Park EH, Min SY, Kim Z, Yoon CS, Jung KW, Nam SJ, et al. Basic facts of breast cancer in Korea in 2014: the 10-year overall survival progress. J Breast Cancer. 2017;20(1):1-11. https://doi.org/10.4048/jbc.2017.20.1.1.
- Toyoda Y, Tabuchi T, Nakayama T, Hojo S, Yoshioka S, Maeura Y. Past trends and future estimation of annual breast cancer incidence in Osaka, Japan. Asian Pac J Cancer Prev. 2016;17(6):2847-52. https://doi.org/APJCP.2016.17.6.2847.
- Fernando A, Jayarajah U, Prabashani S, Fernando EA, Seneviratne SA. Incidence trends and patterns of breast cancer in Sri Lanka: an analysis of the national cancer database. BMC Cancer. 2018;18(1):1-6. https://doi.org/10.1186/s12885-018-4408-4
- Johansson A, Palli D, Masala G, Grioni S, Agnoli C, Tumino R, et al. Epigenome-wide association study for lifetime estrogen exposure identifies an epigenetic signature associated with breast cancer risk. Clin Epigenetics. 2019;11(1):1-12. https://doi.org/10.1186/s13148-019-0664-7.
- Zaheer S, Shah N, Maqbool SA, Soomro NM. Estimates of past and future time trends in age-specific breast cancer incidence among women in Karachi, Pakistan: 2004–2025. BMC Public health. 2019;19(1):1-9. https://doi.org/10.1186/s12889-019-7330-z.
- Mehboob R, Perveen S, Ahmed N. Spectrum of benign breast lesions in a tertiary care hospital of Lahore. Ann King Edw Med Univ. 2018;24(1):605-9. https://doi.org/10.21649/akemu.v24i1.2308.
- Singh SB, Chakrabarti N. A clinicopathological study of benign breast diseases in females. 2020; Med J DY Patil Vidyapeeth [Epub ahead of print] [cited February 5, 2022] https://doi.org/10.4103/mjdrdypu.mjdrdypu_171_20.
- Al-Thoubaity FK. Molecular classification of breast cancer: A retrospective cohort study. Ann Med Surg. 2020;49:44-8. https://doi.org/10.1016/j.amsu.2019.11.021.
- Akhtar N, Sabir F, Zubair M, Ijaz R, Abid R, Kant M, et al. Breast carcinoma in the patients presenting with lump breast, in urban areas of Muzaffarabad, Azad Kashmir. Pak J Surg. 2019;35(3):183-86. http://173.208.131.244:9060/xmlui/handle/123456789/1911.
- Hong’e Li CC, Wang Y, Qin H, Wang J, Zhang S, Teng R, et al. Combined diagnosis of ultrasonic elastography and BI-RADS classification increases diagnostic value in female patients with breast neoplasms. Am J Transl Res. 2021;13(10):11758-763. PMID: 34786104.
- Chiorean AR, Szep MB, Feier DS, Duma M, Chiorean MA, Strilciuc Ș. Impact of Strain Elastography on BI-RADS classification in small invasive lobular carcinoma. Med Ultrason. 2018;20(2):148-53. http://doi.org/10.11152/mu-1272
- Ozsoy A, Aribal E, Araz L, Bora Erdogdu M, Sari A, Sencan I, et al. Mammography quality in Turkey: auditors’ report on a nationwide survey. I J Radiol. 2017;14(1):e13470. https://doi.org/10.5812/iranjradiol.32936
- Strøm B, Jorge JP, Meystre NR, Henner A, Kukkes T, Metsälä E, et al. Challenges in mammography education and training today: the perspectives of radiography teachers/mentors and students in five European countries. Radiography. 2018;24(1):41-6. https://doi.org/10.1016/j.radi.2017.08.008.
- Wang Y, Liu Y, Zheng X, Huang Y, Han J, Li F, et al. Added value of different types of elastography in evaluating ultrasonography detected breast lesions: a compared study with mammography. Clin Breast Cancer. 2020;20(3):e366-72. https://doi.org/10.1016/j.clbc.2019.11.002.
- Arslan S, Uslu N, Ozturk FU, Akcay EY, Tezcaner T, Agildere AM. Can strain elastography combined with ultrasound breast imaging reporting and data system be a more effective method in the differentiation of benign and malignant breast lesions? J Med Ultrason. 2017;44(4):289-96. https://doi.org/10.1007/s10396-017-0772-y.
- Fausto A, Rubello D, Carboni A, Mastellari P, Chondrogiannis S, Volterrani L. Clinical value of relative quantification ultrasound elastography in characterizing breast tumors. Biomed Pharmacother. 2015;75:88-92. https://doi.org/10.1016/j.biopha.2015.08.029
