Case Report
VOLUME: 38 | ISSUE: 1 | Mar 30, 2022 | PAGE: (7 - 9) | DOI: 10.51441/BioMedica/5-617
Appendico-cutaneous fistula - a case report with a review of the literature
Authors: Haseeb Mehmood Qadri , Aroosa Zia , Fahad Qayyum , Muhammad Imran , Muhammad Kareem Ullah , Saeed Mahmood
Article Info
Authors
Haseeb Mehmood Qadri
Department of General Surgery, Lahore General Hospital, Lahore, Pakistan
Aroosa Zia
Department of General Surgery, Lahore General Hospital, Lahore, Pakistan
Fahad Qayyum
Department of General Surgery, Jinnah Hospital, Lahore, Pakistan
Muhammad Imran
Department of Pathology, Allama Iqbal Medical College, Lahore, Pakistan
Muhammad Kareem Ullah
Department of General Surgery, Lahore General Hospital, Lahore, Pakistan
Saeed Mahmood
Department of General Surgery, Lahore General Hospital, Lahore, Pakistan
Publication History
Received: December 27, 2021
Revised: February 19, 2022
Accepted: March 03, 2022
Published: March 30, 2022
Abstract
Acute appendicitis is one of the most common surgical emergencies. The clinical diagnosis augmented with the laboratory and radiology reports qualifies the patient for appendectomy. Mistreated patients in emergency, during the acute episode, sometimes present with a mass in the right iliac fossa with adhesions of the omentum and associated peritonitis. Appendico-cutaneous fistula is an uncommon presentation of appendicitis. It may present as a sinus with discharge. We report a case of a young female who presented with appendicocutaneous fistula.
Keywords: Appendico-cutaneous, appendicitis, fistula, right iliac fossa
Pubmed Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood. Appendico-cutaneous fistula - a case report with a review of the literature. BioMedica. 2022; 30 (March 2022): 7-9. doi:10.51441/BioMedica/5-617
Web Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood. Appendico-cutaneous fistula - a case report with a review of the literature. https://biomedicapk.com/articles/online_first/617 [Access: July 03, 2024]. doi:10.51441/BioMedica/5-617
AMA (American Medical Association) Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood. Appendico-cutaneous fistula - a case report with a review of the literature. BioMedica. 2022; 30 (March 2022): 7-9. doi:10.51441/BioMedica/5-617
Vancouver/ICMJE Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood. Appendico-cutaneous fistula - a case report with a review of the literature. BioMedica. (2022), [cited July 03, 2024]; 30 (March 2022): 7-9. doi:10.51441/BioMedica/5-617
Harvard Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood (2022) Appendico-cutaneous fistula - a case report with a review of the literature. BioMedica, 30 (March 2022): 7-9. doi:10.51441/BioMedica/5-617
Chicago Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood. "Appendico-cutaneous fistula - a case report with a review of the literature." 30 (2022), 7-9. doi:10.51441/BioMedica/5-617
MLA (The Modern Language Association) Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood. "Appendico-cutaneous fistula - a case report with a review of the literature." 30.March 2022 (2022), 7-9. Print. doi:10.51441/BioMedica/5-617
APA (American Psychological Association) Style
Haseeb Mehmood Qadri, Aroosa Zia, Fahad Qayyum, Muhammad Imran, Muhammad Kareem Ullah, Saeed Mahmood (2022) Appendico-cutaneous fistula - a case report with a review of the literature. , 30 (March 2022), 7-9. doi:10.51441/BioMedica/5-617
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(1):7-9
CASE REPORT
Appendico-cutaneous fistula - a case report with a review of the literature
Haseeb Mehmood Qadri1*, Aroosa Zia1, Fahad Qayyum2, Muhammad Imran3, Muhammad Kareem Ullah1, Saeed Mahmood1
Received: 27 December 2021 Revised date: 19 February 2022 Accepted: 03 March 2022
Correspondence to: Haseeb Mehmood Qadri
*Department of General Surgery, Lahore General Hospital, Lahore, Pakistan.
Email: haseebmehmood18@yahoo.com
Full list of author information is available at the end of the article.
ABSTRACT
Acute appendicitis is one of the most common surgical emergencies. The clinical diagnosis augmented with the laboratory and radiology reports qualifies the patient for appendectomy. Mistreated patients in emergency, during the acute episode, sometimes present with a mass in the right iliac fossa with adhesions of the omentum and associated peritonitis. Appendico-cutaneous fistula is an uncommon presentation of appendicitis. It may present as a sinus with discharge. We report a case of a young female who presented with appendico-cutaneous fistula.
Keywords:
Appendico-cutaneous, appendicitis, fistula, right iliac fossa.
Introduction
Acute appendicitis has a lifetime risk of 7%-8%, implying the prevalence of this surgical condition.1 Acute appendicitis is the most common cause of emergency abdominal surgery. The diagnosis of acute appendicitis is mainly based on clinical examination; however, 30%-40% of the cases may present with atypical symptoms. Alvarado’s score and radiologic imaging techniques are used to enhance the diagnostic accuracy.2 The unusual presentation of acute appendicitis as appendico-cutaneous fistula is an important yet uncommon differential diagnosis for clinicians considering entero-cutaneous fistulae. It is a rare but recognized condition, which, as cited by McCrystal et al.3 was first described in 1846. Later, in 1957, it was defined as “the primary perforation of the appendix to an adjacent hollow viscus or to the skin.”4 Spontaneous appendico-cutaneous fistula is characterized by the presence of primary perforation of the appendix to an overlying area of skin, excluding fistulae arising as a sequela of surgically treated appendicitis. The diagnosis of this condition is often delayed due to its gradual onset and symptoms of an abscess in the abdominal wall. Signs of systemic sepsis may be seen. Appendico-cutaneous fistula is managed with laparotomy, appendectomy, drainage of the collection of pus, and excision of the fistulous track.5 As being an uncommon complication of acute appendicitis, the challenges it presents to the surgeon in diagnosis and management, and the scarce literature published on this entity, we describe here a report of an appendico-cutaneous fistula in a young female.
Report of a Case
A 27-year-old fertile female was referred from the gynecology unit to the surgical unit of Lahore General Hospital, Lahore, Pakistan, in June 2021, with an initial complaint of abdominal swelling in the right iliac fossa for 1.5 months. There was no associated history of fever, weight loss, or changes in bowel habits. On physical examination, there was a 20 × 10 cm swelling involving the right lumbar and right iliac regions of the abdomen, with a negative cough impulse. It was painless, erythematous, and fluctuant. Ultrasound (USG) of the abdomen and pelvis revealed a heterogeneous mass 8 × 7 cm in the right iliac fossa. While the report of computed tomography (CT) was awaited, the patient was sent home with conservative management. The patient presented to the surgical outdoor unit a week later with a sinister clinical picture of continuous, undocumented fever, a pustule of 4 × 2 cm present in the right lumbar region with quite a tender abdomen. She was shifted to the surgical emergency. USG of the abdomen and pelvis revealed an ill-defined heterogeneous area measuring 2.9 × 2.1 cm in the right lower abdomen, which was stated as “most likely a collection, suggestive of peritoneal inflammation.” The CT scan of the abdomen and pelvis with contrast showed the presence of an appendico-cutaneous fistula in the right iliac fossa (Figure 1). Complete blood count analysis ordered on the same day in emergency was suggestive of neutrophilic leukocytosis. Exploratory laparotomy was planned to manage the intraperitoneal abscess. Peroperatively, 500 ml pus was drained and a 2 × 2 cm defect was noted in the anterior abdominal wall. The tip of the appendix was adherent to the defect. Appendectomy was performed and the fistulous track was excised. The wound was thoroughly irrigated with normal saline, and alginate dressings were placed around the drain. The wound on the anterior abdominal wall was left open to heal secondarily (Figure 2). A week later, the patient was sent home after intravenous antibiotics therapy and removal of drain. She was later followed-up in the surgical outdoor unit for her wound. A CT scan of the abdomen and pelvis with contrast postoperatively showed the complete resolution of pus collection. The histopathology report of the surgical specimen revealed features of appendicitis and the fistulous tract showed inflamed granulation tissue. No granulomatous inflammation or any malignancy was identified. The patient was followed-up for a month in the surgical outpatient department. The fistulous tract and the laparotomy wound healed without complications.
Discussion
Appendectomy is a frequently performed operation in surgical emergency. Complications of acute appendicitis are mostly associated with perforation. Appendiculo-cutaneous fistula is a tract between appendicular mucosa and the skin presenting as a discharging sinus.6 These fistulae may be primary or secondary with relevance to the cause. Primary appendico-cutaneous fistulae occur spontaneously following a perforation of appendix, appendicular Crohn’s disease, or an appendicular carcinoid tumor.1 Secondary appendico-cutaneous fistulae are a consequence of incomplete appendectomy or appendiceal stump breakdown.2 According to Kjellman,4 the main process involved in the formation of appendico-cutaneous fistula is the spontaneous rupture of the appendix into the adjacent bowel or the skin leading to the erosion and the persistence of fistulous tract is appendix. However, in our case, no appendicolith was found. There was no history of any systemic disease. Various types of fistulous communications reported are appendico-rectal, appendico-intestinal, appendico-uterine, and appendico-renal fistulae.3,7,8 The appendico-cutaneous fistula may present as a discharging sinus on the skin, but the pustule present over the tip of the appendix, communicating with the anterior abdominal wall, leads to the masking of fistulous tract in our case. The fistula was confirmed preoperatively with CT scan, and an intraperitoneal collection of pus was noted. The management may be conservative or surgical.6 Appendiceal fistulae persisting beyond 3 months are treated by surgery if the conservative management of entero-cutaneous fistula fails.9 In our report, the patient was initially treated conservatively. Later, the surgical option was chosen as the pus collection was confirmed on radiological investigation and signs of acute abscess started to appear. Postoperative follow-up for a month revealed secondary healing of the fistulous tract. The recovery was uneventful.
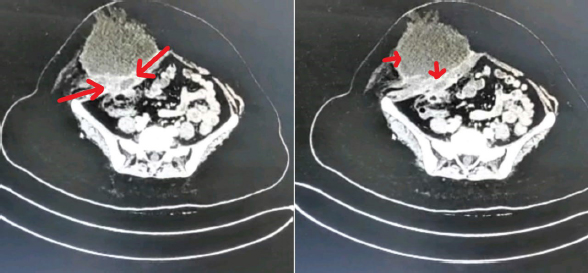
Figure 1. CT scan showing the path of the appendico-cutaneous fistula. There is a collection of pus in the abdominal wall in the left upper part (arrows).

Figure 2. The fistulous tract in the right iliac fossa was kept open to heal with secondary intention. Midline laparotomy scar (arrows) is also visible in the picture.
Conclusion
For clinicians, it is important to consider appendicular abscesses in the list of differential diagnoses for anterior abdominal wall masses. A perforated appendix can present in a very atypical manner, hence it is important to investigate the underlying pathology.
Limitations of the Case Report
The patient was followed-up in the surgical outdoor unit for 1 month. No surgical complication was reported. The patient was lost to contact after a month postoperatively, hence she could not be followed-up for a further period of time.
Acknowledgement
The authors acknowledge the senior colleagues from the General Surgery Department of Lahore General Hospital and Pathology Department of Allama Iqbal Medical College, Lahore, Pakistan, for their logistic and technical support to the case study.
List of Abbreviations
| CT | Computed tomography |
| USG | Ultrasonography |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
Ethical approval was taken from the institutional review board at Allama Iqbal Medical College on 30 July 2021 vide Letter No. 11/CR/AIMC/2021.
Authors’ contributions
All authors: Conception and design of study, acquisition of data, drafting of the manuscript, and approval of the final version of the manuscript to be published.
Authors’ Details
Haseeb Mehmood Qadri1, Aroosa Zia1, Fahad Qayyum2, Muhammad Imran3, Muhammad Kareem Ullah1, Saeed Mahmood1
- Department of General Surgery, Lahore General Hospital, Lahore, Pakistan
- Department of General Surgery, Jinnah Hospital, Lahore, Pakistan
- Department of Pathology, Allama Iqbal Medical College, Lahore, Pakistan
References
- Beaumont O, Miller R, Guy R. Atypical presentation of appendicitis. BMJ Case Rep. 2016;2016:bcr2016217293. https://doi.org/10.1136/bcr-2016-217293
- Souza IMAG, Nunes DAA, Massuqueto CMG, Veiga MAM, Tamada H. Complicated acute appendicitis presenting as an abscess in the abdominal wall in an elderly patient: a case report. Int J Surg Case Rep. 2017;41:5–8. https://doi.org/10.1016/j.ijscr.2017.09.023
- McCrystal S, Kong J, Gourlas P, Morris B, Lutton N. Appendicorectal fistula with a novel solution: first case report and review of the literature. Clin Case Rep. 2019;7(10):1885–9. https://doi.org/10.1002/ccr3.2380
- Kjellman T. Appendiceal fistulae and calculi; review of the literature and a report of three cases. Acta Chir Scand. 1957;113(2):123–39.
- Faulkner G, Pettit SH. Post-traumatic appendicular-cutaneous fistula: a case report. Ann R Coll Surg Engl. 2010;92(1):W6–7. https://doi.org/10.1308/147870810X476665
- Agostinho N, Bains HK, Sardelic F. Enterocutaneous fistula secondary to stump appendicitis. Case Rep Surg. 2017;2017:6135251. https://doi.org/10.1155/2017/6135251
- Parsons SR, Bennett JE, Kaloo P, Scott M. Appendicitis and uterine abscess: presentation of an unusual fistula between the gynaecological and gastrointestinal tracts. BMJ Case Rep. 2012;2012:bcr0920114795. https://doi.org/10.1136/bcr.09.2011.4795
- Nayyar R, Kumar P. Spontaneous appendico-renal fistula: clinical presentation and management of a previously unreported entity. BMJ Case Rep. 2019;12(3):e228278. https://doi.org/10.1136/bcr-2018-228278
- McDonald SJ, Lee F, Dean N, Ridley LJ, Stewart P. Fistulae involving the appendix: a systematic review of the literature. ANZ J Surg. 2020;90(10):1878–87. https://doi.org/10.1111/ans.15805
