Review Article
VOLUME: 38 | ISSUE: 1 | Mar 30, 2022 | PAGE: (3 - 6) | DOI: 10.51441/BioMedica/5-648
Glymphatics and brain fog – the post-COVID-19 phenomenon
Authors: Mulazim Hussain Bukhari , Shumaila Liaqat , Nadia Naseem
Article Info
Authors
Mulazim Hussain Bukhari
Professor of Pathology, Principal, Azad Jammu Kashmir Medical College, Muzaffarabad, Pakistan
Shumaila Liaqat
Department of Pathology, Fatima Jinnah Medical University, Lahore, Pakistan
Nadia Naseem
Professor of Morbid Anatomy and Histopathology, University of Health Sciences, Lahore, Pakistan
Publication History
Received: December 06, 2021
Revised: February 18, 2022
Accepted: March 03, 2022
Published: March 30, 2022
Abstract
Since the COVID-19 pandemic and now since the vaccination has emerged as a success, many new signs and symptoms are being observed. Although most people with COVID-19 get better within weeks of illness, there is a wide range of new, relapsing, or ongoing health problems that many people may experience for weeks or more after being infected with the virus that causes COVID-19. Even people who did not have symptoms when they were infected can have post-COVID conditions. The most commonly reported of these symptoms are related to the neurological system, including brain fog, fatigue, anxiety, anosmia, and depression. The role of glymphatics in post-COVID brain fog is a widely studied phenomenon. This review will also explore the possible etio-pathogenesis of brain fog in post-COVID-19 patients.
Keywords: Glymphatics, SARS-CoV-2, COVID-19, brain fog, neurological symptoms.
Pubmed Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem. Glymphatics and brain fog – the post-COVID-19 phenomenon. BioMedica. 2022; 30 (March 2022): 3-6. doi:10.51441/BioMedica/5-648
Web Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem. Glymphatics and brain fog – the post-COVID-19 phenomenon. https://biomedicapk.com/articles/online_first/648 [Access: July 27, 2024]. doi:10.51441/BioMedica/5-648
AMA (American Medical Association) Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem. Glymphatics and brain fog – the post-COVID-19 phenomenon. BioMedica. 2022; 30 (March 2022): 3-6. doi:10.51441/BioMedica/5-648
Vancouver/ICMJE Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem. Glymphatics and brain fog – the post-COVID-19 phenomenon. BioMedica. (2022), [cited July 27, 2024]; 30 (March 2022): 3-6. doi:10.51441/BioMedica/5-648
Harvard Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem (2022) Glymphatics and brain fog – the post-COVID-19 phenomenon. BioMedica, 30 (March 2022): 3-6. doi:10.51441/BioMedica/5-648
Chicago Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem. "Glymphatics and brain fog – the post-COVID-19 phenomenon." 30 (2022), 3-6. doi:10.51441/BioMedica/5-648
MLA (The Modern Language Association) Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem. "Glymphatics and brain fog – the post-COVID-19 phenomenon." 30.March 2022 (2022), 3-6. Print. doi:10.51441/BioMedica/5-648
APA (American Psychological Association) Style
Mulazim Hussain Bukhari, Shumaila Liaqat, Nadia Naseem (2022) Glymphatics and brain fog – the post-COVID-19 phenomenon. , 30 (March 2022), 3-6. doi:10.51441/BioMedica/5-648
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(1):3-6
MINI REVIEW
Glymphatics and brain fog - the post-COVID-19 phenomenon
Mulazim Hussain Bukhari1*, Shumaila Liaqat2, Nadia Naseem3
Received: 06 December 2021 Revised date: 18 February 2022 Accepted: 03 March 2022
Correspondence to: Mulazim Hussain Bukhari
*Professor of Pathology, Principal, Azad Jammu Kashmir Medical College, Muzaffarabad, Pakistan.
Email: mulazim.hussain.bukhari111@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Since the COVID-19 pandemic and now since the vaccination has emerged as a success, many new signs and symptoms are being observed. Although most people with COVID-19 get better within weeks of illness, there is a wide range of new, relapsing, or ongoing health problems that many people may experience for weeks or more after being infected with the virus that causes COVID-19. Even people who did not have symptoms when they were infected can have post-COVID conditions. The most commonly reported of these symptoms are related to the neurological system, including brain fog, fatigue, anxiety, anosmia, and depression. The role of glymphatics in post-COVID brain fog is a widely studied phenomenon. This review will also explore the possible etio-pathogenesis of brain fog in post-COVID-19 patients.
Keywords:
Glymphatics, SARS-CoV-2, COVID-19, brain fog, neurological symptoms.
Introduction
Neurological complications are widely reported after COVID-19 infection. The development of neurological symptoms in these patients may directly point toward the malfunctioning of glymphatic drainage; a network of lymphatic vessels that clear waste from the central nervous system (CNS), mostly during sleep.1 This results in the abnormal accumulation of fluid, waste products, and inflammatory cytokines in the brain parenchyma, leading to nervous system symptoms like fatigue, depression, myalgias, anosmia, and, in particular, brain fog.2
A study from Northwestern University Feinberg School of Medicine, Chicago, IL, included 100 consecutive patients [50 severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) laboratory-positive and 50 laboratory-negative individuals] presenting between May and November, 2020. The mean age of patients was 43.2 years (±11.3 years); 70% were female and 48% were male. The patients were evaluated post-COVID-19 infection using telemedicine. The most common comorbidities included depression/anxiety (42%) and autoimmune disease (16%), while “brain fog” (81%), headache (68%), numbness/tingling (60%), dysgeusia (59%), anosmia (55%), and myalgias (55%) were also frequently reported in COVID-19-positive patients. The brain fog was characteristically reported more in females.3
The presence of persistent and worsening symptoms in patients with a clinically mild initial course is termed as COVID-19 “long haulers.” Long haulers can be due to mild infections as well, and is not a consequence of severe disease only.4 It has been seen from the laboratory record of these patients that tumor necrosis factor-alpha, interleukin-6 and 8, and other inflammatory markers are persistently high. A low count of CD8+ cells and high levels of chemokine receptor-5 on T cells may help the virus to attach with these receptors, thus migrating them to the sites of inflammation.5 Viral persistence and direct cytopathic effect, immune system dysregulation, and endothelial damage of the blood vessels all lead to the hypoxia of the brain. This results in a low blood supply and metabolic de-arrangements within the brain tissue. In addition, myelin sheath damage, like in multiple sclerosis , has also been reported, which leads to an array of neurological symptoms.6
The underlying pathogenesis, after the infection with the virus ends in the brain tissue, may be as follows:
- It may be immune system hyperactivity, microglial activation with formation of microglial nodules, and destruction of neurons.7
- It may be due to slow clearance of the virus after infecting the monocytes, which delays the recovery of the patients from post-COVID-19 syndrome.8
- Angiotensin-converting enzyme 1 and 2 imbalances leading to grave consequences.9
- Disruption of glymphatics and failure in cleansing system of wastes and proinflammatory cytokines.1
- Damage of blood-brain barrier due to cytokine storm.10
- Damage by mimicry or tissue-mimicking effect of autoantibodies.11
- This may be due to other viruses sitting around and reactivating, e.g., Epstein-Barr virus which, in turn, can cause fatigue.12
Main Symptoms of Long Haulers
There are about more than 200 reported symptoms, but the following are the commonest:1,3,13,14
- Chill
- Sweat
- Respiratory symptoms
- Cough breathlessness
- Gastrointestinal tract (GIT)
- Fatigue
- Post-exertional malaise
- Neurological symptoms (including brain fog, recalling loss, cognitive loss, myalgias, encephalopathy, headache, anosmia, ataxia, seizures, or anosmia and stroke in some patients.
- Body aches
Why Brain Fog, Myalgia, Fatigue, and Depression After COVID-19
Brain fog is a state of confusion when one is not fully alert and engaged (Figure 1). The exact pathogenesis is yet to be explored; however, the abovementioned factors may play a key role in the development of this condition. There are four fluids in the brain, such as:
- Intracellular fluid;
- Interstitial fluid bathing the neuron;
- Blood in the blood vessels;
- Cerebrospinal fluid (CSF), which is formed by choroid plexus by ultrafiltration of blood and circulates in a closed system of lateral ventricles, third ventricle, and fourth ventricle. From the fourth ventricle, it goes to subarachnoid space. From these meninges, the CSF goes back to the venous sinuses.15
What is the Role of Glymphtics in the Brain
The glymphatic system is a connecting system that covers the whole brain tissue. It connects the perivascular spaces where CSF floating around the brain exchanges with the interstitial fluid. When these spaces are filled, the CSF starts oozing out slowly from the periarterial spaces into the brain tissue.1 The role of microchannels, called aquaporins (AQPs), has also been explained. The CSF oozes out of these microchannels toward the interstitial fluid to bathe the neurons and other important brain cells. AQPs are water channel proteins that increase cell membrane water permeability and assemble in cell membranes as tetramers.16 The fluid washes all the metabolic end product, and if there is any inflammation, the inflammatory cells, debris, or any injurious agent present around the neurons flows toward the venous system. From there, through perivenous spaces, the fluid flows toward the cervical and olfactory lymphatic system and gets drained, thus keeping the brain free from damage by the waste products.17
The problem in long haulers is the disruption of this lymphatic system, and the inflammatory end products are not washed out and start accumulating and compressing, thus resulting in a brain fog. Majority of this drainage is near the olfactory nerves with a resultant inflammation of the olfactory nerve in COVID-19 infection, leading to altered or loss of sense of smell.18 The ongoing volume overload and inflammation blocks the lymphatics, thus hampering the drainage of fluid to the venous sinuses. As a result, the fluid and the debris start accumulating in the brain. These end products, which affect the hypothalamus, cause fever, metal confusion, loss of sensation, and disturbance of the emotional system (three main jobs of this area are control of temperature, sensation, and emotion). So, the patients develop fatigue, myalgia, and fever.1,17
The COVID-19 pandemic has become an alarming global issue after its appearance since December 2019 from Wuhan, China. It has shown multisystemic demonstration from SARS-CoV-2 to renal, gastrointestinal, cardiovascular, and neurological manifestations through interacting with the CNS. Clinical and radiological analysis reveals multifocal lesions in the brain; the precise underlying pathogenic pathways are yet to be explored.20
List of Abbreviations
| AQPs: | Aquaporins |
| CNS: | Central nervous system |
| CSF: | Cerebrospinal fluid |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
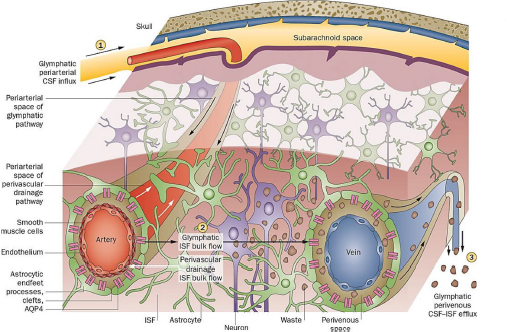
Figure 1. Perivascular clearance comprising perivascular drainage and glymphatic pathways.19
Authors’ contributions
MHB and SL: Conception and design of study, acquisition of data, and drafting of the manuscript.
NN: Acquisition of data, drafting of the manuscript, and important intellectual input.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Mulazim Hussain Bukhari1, Shumaila Liaqat2, Nadia Naseem3
- Professor of Pathology, Principal, Azad Jammu Kashmir Medical College, Muzaffarabad, Pakistan
- Department of Pathology, Fatima Jinnah Medical University, Lahore, Pakistan
- Professor of Morbid Anatomy and Histopathology, University of Health Sciences, Lahore, Pakistan
References
- Neuronline. Understanding the glymphatic system. 2018. Available from: https://neuronline.sfn.org/scientific-research/understanding-the-glymphatic-system#:~:text=The%20glymphatic%20system%20is%20a,some%20diseases%20of%20the%20brain
- Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: post-viral syndrome post COVID-19. Med Hypotheses. 2020;144(17):110055. https://doi.org/10.1016/j.mehy.2020.110055
- Graham EL, Clark JR, Orban ZS, Lim PH, Szymanski AL, Taylor C, et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized COVID-19 “long haulers.” Ann Clin Transl Neurol. 2021;8(5):1073–85. https://doi.org/10.1002/acn3.51350
- Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–5. https://doi.org/10.1001/jama.2020.12603
- Patterson J, Guevara C, Ram Y, Edgar BF, Emily L, Amruta P, et al. Immune-based prediction of COVID-19 severity and chronicity decoded using machine learning. Front Immunol. 2021. https://doi.org/10.3389/fimmu.2021.700782
- Østergaard L. Related microvascular damage and symptoms during and after COVID-19: consequences of capillary transit‐time changes, tissue hypoxia and inflammation. Physiol Rep. 2021;9(3):e14726.2021. https://doi.org/10.14814/phy2.14726. SARS CoV-2
- Ifeoluwa O, Benneth BA, Babatunde AO, Elizabeth T, Akinluyi P, Adeniyi A, Therese DP microglial implications in SARS-CoV-2 infection and COVID-19: lessons from viral RNA neurotropism and possible relevance to Parkinson’s disease. Front Cell Neurosci. 2021;15(6):670298. https://doi.org/10.3389/fncel.2021.670298
- Meidaninikjeh S, Sabouni N, Marzouni HZ, Bengar S, Khalili A, Jafari R. Monocytes and macrophages in COVID-19: friends and foes. Life Sci. 2021;15(269):119010. https://doi.org/10.1016/j.lfs.2020.119010
- Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;13;24(1):422–8. https://doi.org/10.1186/s13054-020-03120-0
- Yarlagadda A, Preston SL, Jeyadhas RP, Lang AE, Hammamieh R, Clayton AH. Blood-brain barrier: COVID-19, pandemics, and cytokine norms. Innov Clin Neurosci. 2021;18(1–3):21–3.
- Gupta M, Weaver DF. COVID-19 as a trigger of brain autoimmunity. ACS Chem Neurosci. 2021;12(14):2558–61. https://doi.org/10.1021/acschemneuro.1c00403
- Gold JE, Okyay RA, Licht WE, Hurley DJ. Investigation of long COVID prevalence and its relationship to Epstein-Barr virus reactivation. Pathogens. 2021;17;10(6):763–9. https://doi.org/10.3390/pathogens10060763
- Ernst J. Most common neurologic symptoms in COVID-19 ‘long-haulers’ include ‘brain fog,’ headache. Available from: https://www.healio.com/news/neurology/20210331/most-common-neurologic-symptoms-in-COVID19-longhaulers-include-brain-fog-headache
- Rita R. As their numbers grow, COVID-19 “long haulers” stump experts. JAMA. 2020;324(14):1381–3. https://doi.org/10.1001/jama.2020.17709
- Telano LN, Baker S. Physiology, cerebral spinal fluid. [Updated 2021 Jul 9]. Treasure Island FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519007/
- Agre P, King LS, Yasui M, Guggino WB, Ottersen OP, Fujiyoshi Y, et al. Aquaporin water channels--from atomic structure to clinical medicine. J Physiol. 2002;542(Pt 1):3–16. https://doi.org/10.1113/jphysiol.2002.020818
- Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The glymphatic system: a beginner’s guide. Neurochem Res. 2015;40(12):2583–99. https://doi.org/10.1007/s11064-015-1581-6
- Wostyn P. COVID-19 and chronic fatigue syndrome: is the worst yet to come? Med Hypotheses. 2021;146(1):110469. https://doi.org/10.1016/j.mehy.2020.110469
- Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, et al. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015;11(8):457–70. https://doi.org/10.1038/nrneurol.2015.119
- Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382(23):2268–70. https://doi.org/10.1056/NEJMc2008597
