Original Article
VOLUME: 38 | ISSUE: 2 | Jun 20, 2022 | PAGE: (94 - 98) | DOI: 10.51441/BioMedica/5-660
Antibiotics prescribing practices for sore throat in a sub-urban primary care clinic
Authors:
Babra Naveed
, Khadija Amna Arif
, Hina Jawaid
, Zia-ul-Hassan
Article Info
Authors
Babra Naveed
Department of Family Medicine, Fatima Memorial Hospital College of Medicine & Dentistry, Lahore, Pakistan.
Khadija Amna Arif
Department of Family Medicine, Fatima Memorial Hospital College of Medicine & Dentistry, Lahore, Pakistan.
Zia-ul-Hassan
Department of Family Medicine, Fatima Memorial Hospital College of Medicine & Dentistry, Lahore, Pakistan.
Publication History
Received: February 07, 2022
Revised: May 22, 2022
Accepted: June 08, 2022
Published: June 20, 2022
Abstract
Background and Objective: Antimicrobial resistance (AMR) is one of the serious health problems in Pakistan. Excessive use of antibiotics during pandemics has aggravated AMR; hence, rational use in the future is even more important to consider and implement. Clinical audits on antibiotic prescribing in general practice can help improve antimicrobial stewardship. This study was designed as an audit to evaluate if the antibiotics prescribed for Streptococcus pharyngitis at a sub-urban primary care center in Pakistan were in line with the standard and latest guidelines.
Methods: A retrospective audit was carried out at the primary care center located at Nainsukh, Lahore, Pakistan during 1 month period. Both adult and pediatric patients (above 3 years of age) presenting with upper respiratory tract infections were included in the study. A total of 48 consultation cards were identified using International Classification of Diseases 10 coding. The antibiotic prescribing practice of primary care physicians was evaluated against the Modified Centor Criteria (MCC) which was used as a standard. A score of ≤3 required no antibiotic whereas a score of ≥ 3 needed a same-day antibiotic prescription for sore throat.
Results: There were 28 (58.3%) patients presenting with MCC of ≤3 and were not given antibiotics. Antibiotic prescriptions issued on the day of presentation were n = 20; however, only n = 7 (35%) met the standard criteria, i.e., MCC score of ≥3 and among these patients, penicillin remained the first choice with 71% patients receiving amoxicillin, while 28% received co-amoxiclav.
Conclusion: Antibiotic stewardship is lacking among general physicians working at the sub-urban primary health care center in Lahore city. Clinical audits, as a part of clinical governance, may help improving the quality of care provided to the community by the regional primary health care physicians.
Keywords: Antimicrobial drug resistance, antibiotics, sore throat, healthcare, antimicrobial stewardship, Modified Centor Criteria
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(2):94-98
ORIGINAL ARTICLE
Antibiotics prescribing practices for sore throat in a sub-urban primary care clinic
Babra Naveed1*  , Khadija Amna Arif1
, Khadija Amna Arif1  , Hina Jawaid2
, Hina Jawaid2  , Zia-ul-Hassan1
, Zia-ul-Hassan1 
Received: 07 February 2022 Revised date: 22 May 2022 Accepted: 08 June 2022
Correspondence to: Babra Naveed
*Department of Family Medicine, Fatima Memorial Hospital College of Medicine & Dentistry, Lahore, Pakistan.
Email: babra.naveed@fmhcmd.edu.pk
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Antimicrobial resistance (AMR) is one of the serious health problems in Pakistan. Excessive use of antibiotics during pandemics has aggravated AMR; hence, rational use in the future is even more important to consider and implement. Clinical audits on antibiotic prescribing in general practice can help improve antimicrobial stewardship. This study was designed as an audit to evaluate if the antibiotics prescribed for Streptococcus pharyngitis at a sub-urban primary care center in Pakistan were in line with the standard and latest guidelines.
Methods:
A retrospective audit was carried out at the primary care center located at Nainsukh, Lahore, Pakistan during 1 month period. Both adult and pediatric patients (above 3 years of age) presenting with upper respiratory tract infections were included in the study. A total of 48 consultation cards were identified using International Classification of Diseases 10 coding. The antibiotic prescribing practice of primary care physicians was evaluated against the Modified Centor Criteria (MCC) which was used as a standard. A score of ≤3 required no antibiotic whereas a score of ≥ 3 needed a same-day antibiotic prescription for sore throat.
Results:
There were 28 (58.3%) patients presenting with MCC of ≤3 and were not given antibiotics. Antibiotic prescriptions issued on the day of presentation were n = 20; however, only n = 7 (35%) met the standard criteria, i.e., MCC score of ≥3 and among these patients, penicillin remained the first choice with 71% patients receiving amoxicillin, while 28% received co-amoxiclav.
Conclusion:
Antibiotic stewardship is lacking among general physicians working at the sub-urban primary health care center in Lahore city. Clinical audits, as a part of clinical governance, may help improving the quality of care provided to the community by the regional primary health care physicians.
Keywords:
Antimicrobial drug resistance, antibiotics, sore throat, healthcare, antimicrobial stewardship, Modified Centor Criteria.
Introduction
Upper respiratory tract infections (URTIs) of viral origin are among the most common reasons for ambulatory visits in the industrialized world. Approximately 100 million antibiotic prescriptions are written, on an average, every year for URTI, and among them, half are prescribed inappropriately leading to antimicrobial resistance (AMR) worldwide.1
AMR, which was initially referred to as antibiotic resistance or drug resistance, was first highlighted in 1945 by Dr. Alexander Fleming.2 AMR develops when disease-causing microbe, through mutation or gene transfer, acquires the ability to survive exposure to an antimicrobial agent that was previously an effective treatment for that particular disease. Sometimes these resistant microorganisms are called superbugs when they show resistance against a wide range of potent broad-spectrum antimicrobials.3 Therefore, the use of rapid, point-of-care tests to identify pathogens and better-targeted treatment regimens could greatly improve the injudicious use of antibiotics. However, there are many limitations of the sensitivity/ culture tests with subsequent increasing incidence of AMR cases worldwide.4
The Asia Pacific region is home to 60% of the world’s population. Within the region, the World Health Organization (WHO) South-East Asia (SEA) countries were believed to have the highest risk of emergence and spread of AMR.5 Major factors that make SEA a global hub for AMR are easy availability of the antimicrobials, lack of knowledge about AMR among health care workers, the easy access of antibiotics to a common man, self-medication practices, irrational antimicrobial prescribing, especially by quacks and availability of poor-quality drug control.6
AMR is one of the crucial health problems in Pakistan. The rapidly evolving pharmaceutical industry with the massive number of registered products (approximately 50,000) is another leading cause of poor antibiotic prescribing practices in Pakistan. The number of drugs prescribed to a patient at one point is very high, i.e., a combination of minimum three drugs per patient is given as a routine, and among them, 70% of patients have prescribed one or more antibiotics. This unjustified and extensive use is very common among public sector hospitals and general physicians with most of them influenced by the pharmaceutical industries.7 Additional factors are unawareness of surveillance systems, non-availability of experts, and widespread use of antibiotics in poultry, livestock, and agriculture in our country.8
Keeping in view the high prevalence of AMR due to inappropriate antibiotic prescribing practices, an audit at the primary health care center was conducted to evaluate if the antibiotics prescribed for Streptococcus pharyngitis were in line with the Modified Centor Criteria (MCC) and WHO recommendations.
Methods
A retrospective clinical audit was carried out at the primary care center at Nainsukh Lahore by the family physicians working at the Departments of Family Medicine at Fatima Memorial College of Medicine & Dentistry, and University of Health Sciences Lahore, Pakistan during 1 month period from July 1 to August 1, 2021. The primary health center, Nainsukh, is the only training site for family medicine postgraduates in Lahore, Punjab. The ethical approval for this study was taken from the Institutional Review Board of Fatima Memorial Hospital College of Medicine & Dentistry. The sample size was taken according to the total population sampling. The study population included both male and female patients, pediatric and adults, who presented with URTI. Pediatric patients enrolled were above 3 years of age. Exclusion criteria included those who presented with URTI with concurrent infections of other organ systems. Patients’ treatment record cards were used to collect the data. A total of 48 consultation cards were extracted, using International Classification of Diseases 10 (ICD-10) coding for acute nasopharyngitis, acute pharyngitis, recurrent pharyngitis, acute laryngitis, acute tonsillitis, recurrent tonsillitis, and tonsillar hypertrophy. Using the codes described above, a total of 49 patients were identified within that month. Patients who were prescribed antibiotics for any other ICD code were excluded from the study. The temperature of each patient was recorded by a nurse before seeing a physician. The physician documents were checked for the history of cough along with examination for tonsillar exudate and/or swelling and lymph nodes enlargement. Consultation cards were checked to identify whether MCC 9 were recorded or not. In the latter case, the finding was assumed to be absent. MCC were used as a standard to justify antibiotic use in pharyngitis (Table 1). After permission, the National Health Service (England) toolkit was used to gather information.10 Rapid antigen testing was not included in this audit as this test is not routinely carried out in our setup due to nonavailability and nonaffordability.
Furthermore, the WHO manual “The Selection and Use of Essential Medicines 2017” 11 was used to assess the prescriber’s antibiotic selection, including its dose, frequency, and duration. For the purpose of audit, another toolkit for the correct selection of antibiotics was created using WHO guidelines 2017. Consultation cards were checked for compliance with WHO guidelines as follows:
Table 1. MCC for group A 8 haemolytic Streptococcus as the origin of sore throat.
| MCCa | Yes | No |
|---|---|---|
| Absence of cough | 1 | 0 |
| Tonsillar exudates or swelling | 1 | 0 |
| Tender cervical lymphadenopathy or lymphadenitis | 1 | 0 |
| Fever >38°C (axillary) | 1 | 0 |
| Age 3-14 years | 1 | 0 |
| Age 15-44 years | 0 | 0 |
| Age >45 years | -1 | 0 |
Total score: <1; 2-3; >4.
Risk of Streptococcus pharyngitis: Low risk; Moderate risk; High risk.
aInterpretation: No culture or antibiotics necessary, return if worse. Culture all, treat if culture result positive. Culture all, treat empirically with antibiotics.
- Amoxicillin: 125-500 mg (50 mg/kg/day) × TDS × 10 days.
- Amoxicillin/clavulanic acid: 125-500 mg (45 mg/kg/day) × TDS × 10 days.
- Clarithromycin: 125-500 mg (7.5 mg/kg/day) × BD ×
10 days. - Erythromycin: 250-500 mg (20-50 mg/kg/day) × TDS × 10 days.
- Phenoxymethylpenicillin: Not available.
The target for the proportion of patients receiving treatment according to MCC and the proportion of antibiotics prescribed according to WHO recommendations was 100%.
Statistical analysis
Data were entered and analyzed in statistical package for the social sciences version 26.0 Descriptive analysis was performed on all the categorical variables in the form of frequency and percentages. Mean ± standard deviation was given for quantitative variables like dose etc.
Results
There were 20 (41.6%) males and 28 (58.4%) females. Age ranged between 3 and 60 years with a maximum (29, 60.4%) number of cases in the age range of 3-14 years (Figure 1).
Patients managed as per MCC score were 35 (73%) (Table 2). A total of 28 (58.3%) patients who presented with MCC of ≤3 were not given antibiotics. It was encouraging to see that 100% standard was met in those with MCC ≤3. There were 20 (41.6%) antibiotic prescriptions issued on the day of presentation however only 7 (35%) met the standard, i.e., patients had a MCC score of ≥3. Among them, penicillin remained the first choice with 5 (71.4%) patients receiving amoxicillin and 2 (28.6%) co-amoxiclav. In 13 (65%) patients, antibiotics were prescribed against the standard and they all were given amoxicillin. There were 7 (35%) children between ages 3 and 5 years among the 20 (41.6%) patients who received antimicrobials. Four (20%) of these children had MCC scores of >3 while 15% had <3 score. There was no delayed prescribing noted in this 1 month’s retrospective audit. Although dosage and frequency were appropriately prescribed in 100% of cases, the proper duration was not found to be mentioned correctly in any consultation card (Table 3).
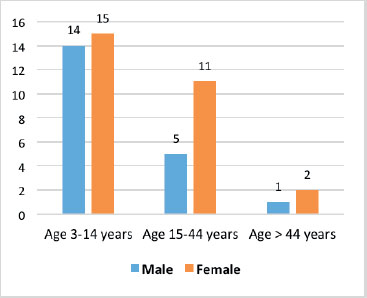
Figure 1. Bar chart showing distribution of patients according to age groups
Of the 48 patients, a record for examination of lymph nodes and tonsils was absent in n = 29 (60.4%) and n = 12 (25%) patients, respectively. History of fever was noted in n = 30 (62.5%) patients while n = 10 (33%) had fever at the time of examination. This audit also identified deficiencies in documentation of medication allergies which was only mentioned in n = 2 (4%) of case notes.
Discussion
AMR is a worldwide phenomenon, and it has the potential to affect anyone, of any age, in any country around the world.12
Higher rates of antibiotic prescribing with an inappropriate selection of antibacterial doses are also observed in other parts of Asian subcontinent too. A nationwide retrospective cross-sectional study conducted in China by Xue et al.13 reporting the antibiotic prescribing practices in children aged less than 5 years with URTIs demonstrated that 27.1% were prescribed injectable antibiotics and that too at a higher dose. This trend was particularly noted in underprivileged areas. In the present study, 35% of children aged 3-5 years were given antibiotics, and 3 had MCC score of <3.
Similarly, a descriptive, nationwide, out-patient based study in Japan reported the proportion of antibiotics prescribed for infectious diseases and observed high prescription rates (56%) for conditions like acute respiratory and gastrointestinal infections which mostly do not require antibiotics treatment. Additionally, in 58.8% of patients with pharyngitis, only 8.8% were given first-line antibiotics (amoxicillin and co-amoxiclav).14
A study observing Spanish general practitioners’ perception of management of a sore throat through a cross-sectional, internet-based questionnaire study, conducted by Llor et al.15 reported interesting findings. Two clinical scenarios were given to the clinicians, a young adult with a sore throat and suffering from cough, coryza with or without fever, depicting a patient with a suspected viral sore throat, with 0 or 1 MCC score while a second scenario comprised of a young adult with a sore throat suffering from fever without cough and coryza with MCC 3. This study reported that antibiotics were considered by 18.8% of the general physicians in the first scenario and by 32% in the second scenario. The most common antibiotics prescribed by the general physicians were amoxicillin and amoxicillin + clavulanic acid (52.7% and 31.2%, respectively). These findings are similar to the present study, however unlike our study, where phenoxymethylpenicillin was not available readily, it was prescribed in 11.9% of the cases in the Spanish study while nearly one-third reported using amoxicillin and clavulanic acid.
Table 2. Antibiotic prescribing practices according to MCC among n = 48 patients.
| MC score 0 n = 1 (2%) | MC score 1 n = 18 (37%) | MC score 2 n = 20 (41%) | MC score 3 n = 8 (16%) | MC score 4 n = 0 (0%) | MC score 5 n = 1 (2%) | Total | |
|---|---|---|---|---|---|---|---|
| Immediate prescribing on the day of the presentation | - | 6 (12) | 7 (14) | 6 (12) | - | 1 (1) | 20 (41.6) |
| No prescribing | 1 (2) | 12 (25) | 13 (27) | 2 (41) | - | - | 28 (58.3) |
| Delayed prescription | - | - | - | - | - | - | - |
Table 3. Antibiotic prescription according to recommended guidelines among n = 7 patients.
| Prescription according to WHO, 2017 | Frequency | Percentage |
|---|---|---|
| Correct choice of antibiotics | 5 (amoxicillin) | 100 |
| 2 (Co-Amoxiclav) | ||
| Appropriate dose prescribed | 7 | 100 |
| Frequency of dose mentioned | 7 | 100 |
| Course length mentioned | 0 | 0 |
Furthermore, our results are comparable to a cross-sectional study from Malaysia involving patients 3 years and above presenting with URTI symptoms. This study revealed that 29.1% of the patients were prescribed antibiotics inappropriately. Amoxycillin and amoxicillin/clavulanic acid was used as the antibiotics of choice in both groups.16 The present study recorded 65% patients who were inappropriately prescribed antibiotics with MC <3 in our audit.
Clinical audit undertaken by Shetty et al.17 to reassess general practice adherence to national guidelines for the management of pharyngitis in Northland, New Zealand involved children and young people aged 3-20 years who attended general practitioners with laboratory-proven streptococcal pharyngitis. Results demonstrated that the management of streptococcal pharyngitis remains substandard with higher rates of amoxicillin prescriptions and inadequate length of treatment. This was similar to the findings of the present study where either the patients were not prescribed antibiotics for reasonable number of days or the data relating to the duration and frequency of doses was not available in the clinical records. Clinical audits as part of clinical governance can help improve the quality of care provided by health care facilities. Continuing medical education, training, and monitoring of clinical practices is crucial to meet standards of care.
Conclusion
Antibiotic stewardship is lacking among general physicians working in the primary care setting in the suburban area of Lahore city. Lack of proper documentation and inappropriate antibiotic prescription, especially among the pediatric population raise serious concern regarding monitoring and quality control of drugs prescribing practices at primary health care units.
Limitation of the study
This audit is a single-center audit. The duration of study was very short. Rapid antigen test for streptococcal pharyngitis was not available at primary care center, Nainsukh, which should be done in patients at MCC score ≥ 3.4. Hence, future large-scale studies with the support of laboratory testing services may be carried out for yielding more conclusive results.
Acknowledgement
The authors would like to acknowledge the staff and the doctors of primary health care center, Nainsukh and Department of Family Medicine, Fatima Memorial College of Medicine & Dentistry Lahore, Pakistan for their logistic and technical support during the execution of the audit.
List of Abbreviations
| ICD-10 | International Classification of Diseases 10 |
| MCC | Modified Centor criteria |
| URTIs | Upper respiratory tract infections |
| WHO | World Health Organization |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The ethical approval was taken from the Institutional Review Board (IRB) of Fatima Memorial Hospital College of Medicine & Dentistry, Lahore, Pakistan vide Letter No. IRB # FMH-05-2021-IRB-904-M dated June 29, 2021.
Authors’ contribution
BN: Concept of the study, acquisition and analysis of data, drafting of manuscript, important intellectual input.
KAA, HJ, ZH: Concept of the study, acquisition of data, drafting of manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Babra Naveed1, Khadija Amna Arif1, Hina Jawaid2, Zia-ul-Hassan1
- Department of Family Medicine, Fatima Memorial Hospital College of Medicine & Dentistry, Lahore, Pakistan
- Department of Family Medicine, University of Health Sciences, Lahore, Pakistan
References
- Aplin-Snider C, Cooper D, Dieleman P, Smith A. Development and implementation of an upper respiratory infection treatment protocol in a primary care health clinic. J Prim Care Community Health. 2020;11:1–6. https://doi.org/10.1177/2150132720966811
- Lammers A, Lalk M, Garbeva P. Air ambulance: antimicrobial power of bacterial volatiles. MDIP. 2022;11(1):109. https://doi.org/10.3390/antibiotics11010109
- Lerminiaux NA, Cameron ADS. Horizontal transfer of antibiotic resistance genes in clinical environments. Can J Microbiol. 2019;65(1):34–44. https://doi.org/10.1139/cjm-2018-0275
- Morel C, McClure L, Edwards S, Sandberg D. Ensuring innovation in diagnostics for bacterial infection: implications for policy. Copenhagen, Denmark: European Observatory on Health Systems and Policies; 2016.
- Yam EL, Hsu LY, Yap EP, Yeo TW, Lee V, Schlundt J, et al. Antimicrobial resistance in the Asia Pacific region: a meeting report. Antimicrob Resist Infect Control. 2019;(8):202. https://doi.org/10.1186/s13756-019-0654-8
- Zellweger RM, Carrique-Mas J, Limmathurotsakul D, Day NP, Thwaites GE, Baker S. Southeast Asia antimicrobial resistance network. A current perspective on antimicrobial resistance in Southeast Asia. J. Antimicrob. Chemother. 2017;72(11):2963–72. https://doi.org/10.1093/jac/dkx260
- Saleem Z, Hassali MA, Hashmi FK. Pakistan's national action plan for antimicrobial resistance: translating ideas into reality. Lancet Infect Dis. 2018;18(10):1066–7. https://doi.org/10.1016/S1473-3099(18)30516-4
- Saeed DK, Farooqi J, Shakoor S, Hasan R. Antimicrobial resistance among GLASS priority pathogens from Pakistan: 2006-2018. BMC Infect. Dis. 2021;21(1):1–6. https://doi.org/10.1186/s12879-021-06795-0
- Palla AH, Khan RA, Gilani AH, Marra F. Over prescription of antibiotics for adult pharyngitis is prevalent in developing countries but can be reduced using McIsaac modification of Centor scores: a cross-sectional study. BMC Pulm Med. 2012;12(1):1–7. https://doi.org/10.1186/1471-2466-12-70
- Gulliford MC, Prevost AT, Charlton J, Juszczyk D, Soames J, McDermott L, et al. Effectiveness and safety of electronically delivered prescribing feedback and decision support on antibiotic use for respiratory illness in primary care: REDUCE cluster randomised trial. BMJ. 2019;364:1236. https://doi.org/10.1136/bmj.l236
- World Health Organization. WHO model list of essential medicines for children: 6th list (March 2017, amended August 2017). Geneva, Switzerland: World Health Organization.
- Global action plan on antimicrobial resistance [Internet]; 2015 [cited 2021 Oct 20]. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R7-en.pdf?ua=1%20
- Xue F, Xu B, Shen A, Shen K. Antibiotic prescriptions for children younger than 5 years with acute upper respiratory infections in China: a retrospective nationwide claims database study. BMC Infect Dis. 2021;21(1):1. https://doi.org/10.1186/s12879-021-05997-w
- Hashimoto H, Saito M, Sato J, Goda K, Mitsutake N, Kitsuregawa M, et al. Indications and classes of outpatient antibiotic prescriptions in Japan: a descriptive study using the national database of electronic health insurance claims, 2012-2015. In J Infect Dis. 2020;91:1–8. https://doi.org/10.1016/j.ijid.2019.11.009
- Llor C, Vilaseca I, Lehrer-Coriat E, Boleda X, Moragas A, Cots JM. Survey of Spanish general practitioners' attitudes toward management of sore throat: an internet-based questionnaire study. BMC Fam Pract. 2017;18(1):1–6. https://doi.org/10.1186/s12875-017-0597-1
- Ahmad A, Nor J, Abdullah AA, Kamauzaman TH, Yazid MB. Patient factors in inappropriate antibiotic prescribing for upper respiratory tract infection in the emergency department. Malays J Med Sci. 2021;28(2):72. https://doi.org/10.21315/mjms2021.28.2.7
- Shetty A, Mills C, Eggleton K. Primary care management of group A streptococcal pharyngitis in Northland. J Prim Health Care. 2014;6(3):189–94. https://doi.org/10.1071/HC14189
