Original Article
VOLUME: 39 | ISSUE: 2 | Jun 25, 2023 | PAGE: (61 - 66) | DOI: 10.24911/BioMedica/5-936
Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore
Authors: Farhan Rasheed , Iqra Jamil , Tahira Tehseen , Ahmad Yar , Farhana Ali , Ameena Ashraf
Article Info
Authors
Farhan Rasheed
Associate Professor, Department of Pathology, Allama Iqbal Medical College, Lahore, Pakistan.
Iqra Jamil
PhD Microbiology Scholar, Department of Industrial Biotechnology, Government College University, Lahore, Pakistan.
Tahira Tehseen
Assistant Professor, Department of Pathology, Wah Medical College, Wah Cantt, Pakistan.
Ahmad Yar
Classified Pathologist, Combined Military Hospital, Sialkot, Pakistan.
Farhana Ali
Assistant Professor, Department of Pathology, University of Child Health Sciences, The Children’s Hospital, Lahore, Pakistan.
Ameena Ashraf
Professor, Department of Pathology, Allama Iqbal Medical College, Lahore, Pakistan.
Publication History
Received: March 27, 2023
Revised: May 01, 2023
Accepted: June 04, 2023
Published: June 25, 2023
Abstract
Background and Objective: Typhoid fever caused by Salmonella typhi (S. typhi) is an important cause of morbidity and mortality worldwide. The emergence of resistance against the first and second line of drugs has limited the range of drug choices for its treatment. Therefore, the present study was designed to assess the status of drug resistance in S. typhi isolated from the blood samples of pediatric patients reporting at a leading tertiary care hospital in Lahore.
Methods: This descriptive study was conducted at the Pathology Department of Allama Iqbal Medical College, Lahore, Pakistan, over a period of 2 years. A total of 1,306 blood samples were aseptically collected from the pediatric population of Jinnah Hospital, Lahore, Pakistan, after obtaining informed assent from the parents/guardians. The samples were transferred into a Bact/Alert blood culture bottle. After the detection of microbial growth by the Bact/Alert 3-D system, bacterial isolates were identified by standard microbiological procedures. VITEK 2 compact automated identification and antimicrobial susceptibility testing instrument (bioMerieux) was used for the antimicrobial sensitivity testing. Data were entered and analyzed by using Statistical Package for the Social Sciences version 21.0.
Results: A total of 235 out of 1,306 (17.9%) blood culture samples yielded bacterial growth, among which 62.5% (n = 147) were S. typhi. Among 147 S. typhi isolates, 70.6% were multidrug resistant, while 63% were extensively drug resistant (XDR). Maximum resistance against first-line drugs observed was for ampicillin (79.4) and co-trimoxazole (67.2).
Conclusion: The emergence and spread of XDR S. typhi with a high level of resistance are quite alarming, leaving limited treatment options for the pediatric population. Moreover, increasing resistance to antibiotics demonstrates the quick waning of the efficacy of available first and second-line drugs in the treatment of typhoid fever.
Keywords: Salmonella typhi, multidrug resistant (MDR), extensive-drug resistant (XDR), typhoid fever, antibiotics.
Pubmed Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf. Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore. BioMedica. 2023; 25 (June 2023): 61-66. doi:10.24911/BioMedica/5-936
Web Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf. Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore. https://biomedicapk.com/articles/online_first/936 [Access: July 27, 2024]. doi:10.24911/BioMedica/5-936
AMA (American Medical Association) Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf. Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore. BioMedica. 2023; 25 (June 2023): 61-66. doi:10.24911/BioMedica/5-936
Vancouver/ICMJE Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf. Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore. BioMedica. (2023), [cited July 27, 2024]; 25 (June 2023): 61-66. doi:10.24911/BioMedica/5-936
Harvard Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf (2023) Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore. BioMedica, 25 (June 2023): 61-66. doi:10.24911/BioMedica/5-936
Chicago Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf. "Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore." 25 (2023), 61-66. doi:10.24911/BioMedica/5-936
MLA (The Modern Language Association) Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf. "Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore." 25.June 2023 (2023), 61-66. Print. doi:10.24911/BioMedica/5-936
APA (American Psychological Association) Style
Farhan Rasheed, Iqra Jamil, Tahira Tehseen, Ahmad Yar, Farhana Ali, Ameena Ashraf (2023) Trend of Antimicrobial Resistance Among Salmonella Typhi Isolated from Pediatric Population Presenting at a Tertiary Care Hospital in Lahore. , 25 (June 2023), 61-66. doi:10.24911/BioMedica/5-936
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 39(2):61-66
ORIGINAL ARTICLE
Trend of antimicrobial resistance among Salmonella typhi isolated from the pediatric population presenting at a tertiary care hospital in Lahore
Farhan Rasheed1, Iqra Jamil2*, Tahira Tehseen3, Ahmad Yar4, Farhana Ali5, Ameena Ashraf6
Received: 27 March 2023 Revised date: 01 May 2023 Accepted: 04 June 2023
Correspondence to: Iqra Jamil
*PhD Microbiology Scholar, Department of Industrial Biotechnology, Government College University, Lahore, Pakistan.
Email: iqrajameel@hotmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Typhoid fever caused by Salmonella typhi (S. typhi) is an important cause of morbidity and mortality worldwide. The emergence of resistance against the first and second line of drugs has limited the range of drug choices for its treatment. Therefore, the present study was designed to assess the status of drug resistance in S. typhi isolated from the blood samples of pediatric patients reporting at a leading tertiary care hospital in Lahore.
Methods:
This descriptive study was conducted at the Pathology Department of Allama Iqbal Medical College, Lahore, Pakistan, over a period of 2 years. A total of 1,306 blood samples were aseptically collected from the pediatric population of Jinnah Hospital, Lahore, Pakistan, after obtaining informed assent from the parents/guardians. The samples were transferred into a Bact/Alert blood culture bottle. After the detection of microbial growth by the Bact/Alert 3-D system, bacterial isolates were identified by standard microbiological procedures. VITEK 2 compact automated identification and antimicrobial susceptibility testing instrument (bioMerieux) was used for the antimicrobial sensitivity testing. Data were entered and analyzed by using Statistical Package for the Social Sciences version 21.0.
Results:
A total of 235 out of 1,306 (17.9%) blood culture samples yielded bacterial growth, among which 62.5% (n = 147) were S. typhi. Among 147 S. typhi isolates, 70.6% were multidrug resistant, while 63% were extensively drug resistant (XDR). Maximum resistance against first-line drugs observed was for ampicillin (79.4) and co-trimoxazole (67.2).
Conclusion:
The emergence and spread of XDR S. typhi with a high level of resistance are quite alarming, leaving limited treatment options for the pediatric population. Moreover, increasing resistance to antibiotics demonstrates the quick waning of the efficacy of available first and second-line drugs in the treatment of typhoid fever.
Keywords:
Salmonella typhi, multidrug resistant (MDR), extensive-drug resistant (XDR), typhoid fever, antibiotics.
Introduction
Typhoid fever caused by Salmonella enterica serovar typhi is a systemic infection resulting in an increased morbidity and mortality rate throughout the world. About 10.9 million new cases and 116,800 typhoid fever-related deaths are reported to be occurring per year globally.1,2 According to the World Health Organization (WHO), typhoid is a serious public health issue that primarily affects children and young people.3 The third-highest typhoid rate in the world is reported in Pakistan. In 2020, the prevalence rate of typhoid fever affecting children between the ages of 2 and 5 years was 573.2 per 100,000 population per year in Pakistan.4 Route of transmission is mainly oral-fecal for enteric fever; therefore, the consumption of fecal-contaminated water and food plays a major role in its spread.5
Ampicillin, co-trimoxazole, and chloramphenicol were considered to be the first-line antibiotics for typhoid fever treatment,6 but during the last few decades, the emergence of multidrug resistance (MDR) in S. typhi strains, particularly in developing countries, has been reported in escalation. MDR S. typhi strains are generally regarded to be resistant against at least one of the three or more than three categorically differentiated antimicrobials, such as ampicillin, sulfonamides (trimethoprim-sulfamethoxazole), and chloramphenicol, whereas extensively drug-resistant (XDR) are those which are observed to be resistant to all but one or two antimicrobials, demonstrating resistance against several types of antibiotics, such as chloramphenicol, ampicillin, sulfonamides, fluoroquinolones (ciprofloxacin), and third-generation cephalosporins (ceftazidime, cefuroxime, and ceftriaxone), leaving out few options, such as piperacillin/tazobactam, azithromycin, and carbapenems, as efficient treatment options.7,8 Acquisition of resistant genes in S. typhi strains is mainly caused by transmissible plasmids. The first isolate of MDR S. typhi was reported between 1970 and 1980, which exhibited resistance to first-line drugs (ampicillin, co-trimoxazole, and chloramphenicol).9 Thereafter, ciprofloxacin became the preferred drug for S. typhi infections, but resistance developed quickly. The first case of ciprofloxacin resistance was reported in 1991.10 However, the incidence of MDR-S. typhi increased from 34.2% to 48.5% during the period from 2001 to 2006 as reported by the Aga Khan University in Pakistan. During this period, ciprofloxacin resistance also raised from 1.6% to 64.1%.11
Third-generation cephalosporins, macrolides, and carbapenems have been used more frequently to treat typhoid fever since the development of MDR S. typhi and fluoroquinolone resistance. In Pakistan, the first case of XDR S. typhi was reported in Hyderabad in 2016. XDR strain showed resistance against first-line drugs, a fluoroquinolone, and a third-generation cephalosporin.12,13 Since then, more than 10,365 infections with XDR S. typhi have been reported from Pakistan, as per WHO reports.14 Despite the efforts made by infection control programs to control the disease, there was a gradual increase in documented cases over a 2-year period (2017 to 2018).14 Therefore, the present study was designed to determine the frequency and current status of drug resistance of S. typhi isolated from the blood samples of pediatric patients with septicemia presenting at one of the largest tertiary care hospitals in Lahore, Pakistan.
Methods
The present study was conducted at the Pathology Department of Allama Iqbal Medical College, Lahore, Pakistan, over a period of 2 years, from January 1, 2021 to December 31, 2022. Samples were collected from the college associated with Jinnah Hospital, Lahore. Samples from both genders of pediatric patients, suspected of bacterial sepsis and presenting with fever,15 within the age group of 0-12 years, were included in the study. Repetitive samples from the same patient were excluded. Also, patients with bleeding disorders, multiple co-morbidities, having any malignancy, or who were already on antibiotic therapy were excluded. A total of 1,306 blood cultures from suspected cases of bacterial sepsis were analyzed. Blood samples (4 ml) were collected in Bact/Alert blood culture bottles from each patient by an experienced staff nurse. The samples were transported to the Microbiology Laboratory. Blood culturing was done through automation in the Bact/Alert 3-D culture system (bioMerieux, Durham, NC).16 After the detection of microbial growth, Gram staining was performed on the positive samples. Samples were sub-cultured on blood agar (Oxoid Ltd., Basingstoke, UK), chocolate agar (Oxoid Ltd., Basingstoke, UK), and MacConkey agar (Oxoid Ltd., Basingstoke, UK). After sub-culturing, the inoculated culture plates were incubated for 18-24 hours at 37°C aerobically. After overnight incubation, different microbiological procedures were used to identify bacterial isolates.17 For the identification of Gram-negative bacteria, Analytical Profile Index 20E was used.18 VITEK 2 compact automated identification and antimicrobial susceptibility testing instruments (bioMerieux) were used for the antimicrobial sensitivity testing.19 The isolates were labeled “multidrug-resistant” (MDR), which was resistant to first line drugs, and “extensively drug-resistant” (XDR), which showed resistance to more than two classes of antibiotics.20
Statistical analysis
Data were entered and analyzed by using Statistical Package for the Social Sciences version 21.0. Sensitivity patterns were presented as frequency and percentages. Cross tabulation was done for gender and age. The chi-square test was used to assess statistical significance with a p-value < 0.05 taken as statistically significant.
Results
Out of 1,306 blood cultures, 235 (17.9%) were positive for bacterial growth. Out of these 235 positive samples, 62.5% yielded S. enterica species (72.1% were S. typhi while 27.9% were S. paratyphi A). The sensitivity pattern of all the isolates (n = 147) indicated 70.6% were MDR while 63% were XDR S. enterica isolates (Figure 1).
Antimicrobial susceptibility testing revealed that 79.4%, 74.7%, and 67% of S. typhi were resistant to ampicillin, ciprofloxacin, and co-trimoxazole, respectively, while 65.4% isolates were resistant to chloramphenicol. All isolates of S. paratyphi A tested for azithromycin were susceptible (Table 1).
Discussion
Enteric fever is a serious public health issue across the world, putting a significant burden on healthcare system, especially in developing countries. In Pakistan, an alarming situation regarding antibiotic resistance has been developed because of the increase in the emergence of MDR and XDR strains.5 In the present study, 72.1% (n = 106) isolates were of S. typhi out of 147 S. enterica species. Similar results were reported by Khanal et al.21 from B. P. Koirala Institute of Health Sciences Hospital, Nepal, in which S. typhi was the most common serotype isolated from the blood samples from the patients with enteric fever. Another study by Zakir et al.22 from Pakistan in 2021 also reported S. typhi as the most common serotype (90%) isolated from patients with enteric fever. In accordance with our study, Fatima et al.23 and Qamar et al.24 from Pakistan also reported similar results.
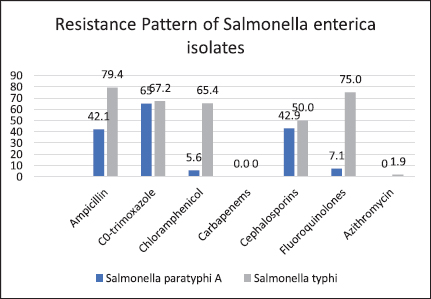
Figure 1. Resistance pattern of S. enterica serovars against different classes of antimicrobial drugs. Resistance of S. typhi against ampicillin was 79.4%, while 75% and 67.2% of isolates were resistant to fluoroquinolones and co-trimoxazole, respectively. 65% S. paratyphi A isolates were resistant to co-trimoxazole. Carbapenems showed 100% sensitivity against S. typhi and S. paratyphi A.
Table 1. Antimicrobial sensitivity pattern of S. typhi among 147 isolates.
| Antibiotics | Sensitive (%) | Resistant (%) |
|---|---|---|
| First line drugs 1. Ampicillin 2. C0-trimoxazole 3. Chloramphenicol |
22 (20.6) 35 (32.8) 37 (34.6) |
85 (79.4)a 72 (67.2) 70 (65.4) |
| Second line drugs 1. Ciprofloxacin 2. Ceftriaxone 3. Cefipime |
27 (25.3) 54 (46.8) 62 (58) |
80 (74.7) 53 (53.2) 45 (42) |
| Third line drugsa 1. Imipenem 2. Meropenem |
107 (100) 107 (100) |
0 (0) 0 (0) |
aMaximum resistance was observed against ampicillin (79.4%), while 100% isolates were sensitive against third line of drugs.
Various studies from all over Pakistan have documented the presence of MDR S. typhi.21-23 MDR S. typhi are found to be resistant against first-line antibiotics, which include ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazole. In the present study, 70.6% of isolates were found to be MDR. A retrospective study conducted by Klemm et al.,12 conducted over a period of 9 years, also reported a high burden of MDR and fluoroquinolones-resistant strains. Blood samples were collected from tertiary care hospitals of Karachi and Hyderabad from the Sindh region of Pakistan Similar results were also reported by Park et al.,25 who showed a rapid increase in MDR S. typhi in Ghana, Kenya, and Tanzania, and reported 52% MDR S. typhi isolates among the total number of S. typhi strains across the samples collected from 11 countries of Sub Saharan Africa. Misuse or uncontrolled use of antimicrobials that are sold over the counter without a prescription or medical supervision may be the root cause of the emergence of MDR strains.
In Pakistan, the majority of MDR strains of S. typhi have attained additional resistance to fluoroquinolones and beta-lactams, which marked them as XDR.12 In the current study, 63% isolates were found to be XDR, which were in accordance with another study conducted in Pakistan which reported 54% XDR strains.26 Similar to our results, many local and international studies also reported a high prevalence of XDR strains.25-29 In the current study, 79.4% and 67% of S. typhi were resistant to ampicillin and co-trimoxazole, respectively. A study conducted in China documented ascending trends in resistance to ampicillin (91%) and co-trimoxazole (88%) in S. typhi isolated from blood samples from patients with enteric fever.30 The two drugs ceftriaxone and ciprofloxacin are regarded as the main pillars of typhoid treatment, especially in developing countries, but in the present study, high resistance was also observed against these antibiotics. A total of 75% of isolates showed resistance against ciprofloxacin in the current study, which is in accordance with other similar studies published locally and internationally.12,29,31,32 Similar results were also reported in a study conducted in Taiwan, which showed 69% resistance against ciprofloxacin.33 Association of the resistance pattern of S. typhi with gender and age was found to be statistically insignificant in the present study (Tables 2 and 3), which depicts that gender and age are independent of the antimicrobial resistance pattern in the study population.
Table 2. Antimicrobial sensitivity pattern of S. typhi with respect to gender (cross tabulation).
| Category | Drugs | Male | Female | p-value* | ||
|---|---|---|---|---|---|---|
| Sensitive (%) | Resistant (%) | Sensitive (%) | Resistant (%) | |||
| First line drugs | Ampicillin | 19.8% | 80.2% | 21.5% | 78.5% | 0.08 |
| Co-trimoxazole | 36.6% | 63.4% | 29% | 71% | ||
| Chloramphenicol | 35.8% | 64.2% | 33.4% | 66.6% | ||
| Second line drugs | Ciprofloxacin | 24.3% | 75.7% | 26.3% | 73.7% | 0.06 |
| Ceftriaxone | 45.8% | 54.2% | 47.8% | 52.2% | ||
| Cefipime | 54.5% | 45.5% | 61.5% | 38.5% | ||
| Third line drugs | Imipenem | 100% | 0% | 100% | 0% | 0.1 |
| Meropenem | 100% | 0% | 100% | 0% |
*Statistically insignificant results reflect no association between gender and resistance pattern of S. typhi.
Table 3. Antimicrobial sensitivity pattern of S. typhi with respect to age (cross tabulation).
| Category | Drugs | <10 years | >10 years | p-value* | ||
|---|---|---|---|---|---|---|
| Sensitive (%) | Resistant (%) | Sensitive (%) | Resistant (%) | |||
| First line drugs | Ampicillin | 18.8 | 81.2 | 22.4 | 77.6 | 0.07 |
| Co-trimoxazole | 34.6 | 65.4 | 31 | 69 | ||
| Chloramphenicol | 36.8 | 63.2 | 32.4 | 67.6 | ||
| Second line drugs | Ciprofloxacin | 24.8 | 75.2 | 25.9 | 74.1 | 0.06 |
| Ceftriaxone | 44.8 | 55.2 | 48.8 | 51.2 | ||
| Cefipime | 53.8 | 46.2 | 62.2 | 37.8 | ||
| Third line drugs | Imipenem | 100 | 0.0 | 100 | 0.0 | 0.12 |
| Meropenem | 100 | 0.0 | 100 | 0.0 |
*Statistically insignificant results depict no association between age and resistance pattern of S. typhi.
Regarding third-line drugs for enteric fever treatment, carbapenems showed 100% sensitivity against S. enterica serovars. Azithromycin was also highly sensitive against S. enterica isolates. A study conducted by Sjölund-Karlsson et al.34 also reported 93.6% sensitivity to azithromycin against S. typhi isolated from the blood samples of enteric fever patients. Nowadays, azithromycin is the drug of choice for treating uncomplicated enteric fever. The prospect of antibiotic resistance, however, necessitates continuous monitoring of its sensitivity patterns.
While focusing on increasing antimicrobial resistance, actions must be taken to raise health and hygiene awareness among health practitioners as well as for the general population. In developing countries such as Pakistan, where antibiotic stewardship programs are not up to date, this should be a serious concern for organizations working on it. Various practices, including good hand hygiene, improved sanitation, and effective antibiotic policy, can help to control the disease and thereby reduce antimicrobial resistance in the community. To reduce the burden of disease caused by S. typhi, effective surveillance, improved diagnostics, more rational antimicrobial usage, and effective mass vaccination will all be crucial.
Conclusion
The emergence and spread of XDR S. typhi with a high level of resistance are quite alarming, leaving limited treatment options for the pediatric population in Pakistan. Moreover, increasing resistance to antibiotics demonstrates the quick waning of the efficacy of available first- and second-line drugs in the treatment of typhoid fever. Antibiotic stewardship, continuous surveillance, and vaccination on a mass level should be the priority areas to reduce the spread of this deadly disease.
Limitations of the Study
This was a single-center study; because of the extensive spread of XDR S. typhi, a multicenter study should be conducted to determine a more exploratory and representative picture of the resistance pattern in our region.
Acknowledgement
The authors would like to acknowledge all the respondents who participated in the study, including the staff of the Pathology department of Allama Iqbal Medical College Lahore, Pakistan, who processed the samples.
List of Abbreviations
| ID/AST | Identification and antimicrobial susceptibility testing |
| MDR | Multidrug resistant |
| S. typhi | Salmonella typhi |
| WHO | World Health Organization |
| XDR | Extensively drug resistant |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The study was approved by the Ethical Review Board of Allama Iqbal Medical College/Jinnah Hospital, Lahore, Pakistan, vide reference no: 47/ERB/2019, dated March 13th, 2019.
Authors’ contributions
FR: Concept and design of study, analysis of data, critical intellectual input to the manuscript.
IJ, TT, AY: Drafting the manuscript, acquisition of data.
FA, AA: critical intellectual input to the manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Farhan Rasheed1, Iqra Jamil2, Tahira Tehseen3, Ahmad Yar4, Farhana Ali5, Ameena Ashraf6
- Associate Professor, Department of Pathology, Allama Iqbal Medical College, Lahore, Pakistan
- Ph.D Microbiology Scholar, Department of Industrial Biotechnology, Government College University, Lahore, Pakistan
- Assistant Professor, Department of Pathology, Wah Medical College, Wah Cantt, Pakistan
- Classified Pathologist, Combined Military Hospital, Sialkot, Pakistan
- Assistant Professor, Department of Pathology, University of Child Health Sciences, The Children’s Hospital, Lahore, Pakistan
- Professor, Department of Pathology, Allama Iqbal Medical College, Lahore, Pakistan
References
- Stanaway JD, Reiner RC, Blacker BF, Goldberg EM, Khalil IA, Troeger CE, et al. The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis. 2019 Apr 1;19(4):369–81. https://doi.org/10.1016/S1473-3099(18)30685-6.
- Marchello CS, Hong CY, Crump JA. Global typhoid fever incidence: a systematic review and meta-analysis. Clin Infect Dis. 2019 Mar 7;68(Supplement_2):S105–16. https://doi.org/10.1093/cid/ciy1094
- Steele AD, Hay Burgess DC, Diaz Z, Carey ME, Zaidi AK. Challenges and opportunities for typhoid fever control: a call for coordinated action. Clin Infect Dis. 2016 Mar 15;62(suppl_1):S4–8. https://doi.org/10.1093/cid/civ976
- Akram J, Khan AS, Khan HA, Gilani SA, Akram SJ, Ahmad FJ, et al. Extensively drug-resistant (XDR) typhoid: evolution, prevention, and its management. BioMed Res Int. 2020 May 2;2020:6432580. https://doi.org/10.1093/cid/civ976
- Radhakrishnan A, Als D, Mintz ED, Crump JA, Stanaway J, Breiman RF, et al. Introductory article on global burden and epidemiology of typhoid fever. Am J Trop Med Hyg. 2018 Sep;99(3 Suppl):4. https://doi.org/10.4269/ajtmh.18-0032
- Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of invasive Salmonella infections. Clin Microbiol Rev. 2015 Oct;28(4):901–37. https://doi.org/10.1128/cmr.00002-15
- Basak S, Singh P, Rajurkar M. Multidrug resistant and extensively drug resistant bacteria: a study. J Pathog. 2016 Oct;2016:4065603. https://doi.org/10.1155/2016/4065603
- Saeed M, Rasool MH, Rasheed F, Saqalein M, Nisar MA, Imran AA, et al. Extended-spectrum beta-lactamases producing extensively drug-resistant Salmonella typhi in Punjab, Pakistan. J Infect Dev Ctries. 2020 Feb 29;14(02):169–76. https://doi.org/10.3855/jidc.12049
- Dyson ZA, Klemm EJ, Palmer S, Dougan G. Antibiotic resistance and typhoid. Clin Infect Dis. 2019 Mar 7;68(Supplement_2):S165–70. https://doi.org/10.1093/cid/ciy1111
- Umasankar S, Wall RA, Berger J. A case of ciprofloxacin-resistant typhoid fever. Commun Dis Rep CDR Rev. 1992 Nov 1;2(12):R139–40.
- Hasan R, Zafar A, Abbas Z, Mahraj V, Malik F, Zaidi A. Antibiotic resistance among Salmonella enterica serovars typhi and paratyphi A in Pakistan (2001-2006). J Infect Dev Ctries. 2008 Aug 1;2(04):289–94. https://doi.org/10.3855/jidc.224
- Klemm EJ, Shakoor S, Page AJ, Qamar FN, Judge K, Saeed DK, et al. Emergence of an extensively drug-resistant Salmonella enterica serovar typhi clone harboring a promiscuous plasmid encoding resistance to fluoroquinolones and third-generation cephalosporins. mBio. 2018 Mar 7;9(1):e00105–18. https://doi.org/10.1128/mbio.00105-18
- Qamar FN, Yousafzai MT, Khalid M, Kazi AM, Lohana H, Karim S, et al. Outbreak investigation of ceftriaxone-resistant Salmonella enterica serotype typhi and its risk factors among the general population in Hyderabad, Pakistan: a matched case-control study. Lancet Infect Dis. 2018 Dec 1;18(12):1368–76. https://doi.org/10.1016/S1473-3099(18)30483-3
- Majeed MM, Munir A. Pakistan: country report on children’s environmental health. Rev. Environ Health. 2020 Mar 26;35(1):57–63. https://doi.org/10.1515/reveh-2019-0087
- Al-Mulla NA, Taj-Aldeen SJ, El Shafie S, Janahi M, Al-Nasser AA, Chandra P. Bacterial bloodstream infections and antimicrobial susceptibility pattern in pediatric hematology/oncology patients after anticancer chemotherapy. Infect Drug Resist. 2014 Nov 6:289–99.
- Butt T, Afzal RK, Ahmad RN, Salman M, Mahmood A, Anwar M. Bloodstream infections in febrile neutropenic patients: bacterial spectrum and antimicrobial susceptibility pattern. J Ayub Med Coll Abbottabad. 2004;16(1):18–22.
- Kara Ö, Zarakolu P, Aşçioğlu S, Etgül S, Uz B, Büyükaşik Y, et al. Epidemiology and emerging resistance in bacterial bloodstream infections in patients with hematologic malignancies. Infect Dis Rev. 2015 Oct 3;47(10):686–93. https://doi.org/10.3109/23744235.2015.1051105
- Wasihun AG, Wlekidan LN, Gebremariam SA, Dejene TA, Welderufael AL, Haile TD, et al. Bacteriological profile and antimicrobial susceptibility patterns of blood culture isolates among febrile patients in Mekelle Hospital, Northern Ethiopia. Springerplus. 2015 Dec;4(1):1–7. https://doi.org/10.1186/s40064-015-1056-x
- Gupta S, Kashyap B. Bacteriological profile and antibiogram of blood culture isolates from a tertiary care hospital of North India. Trop J Med Res. 2016 Jul 1;19(2):94–9.
- Sharma P, Dahiya S, Manral N, Kumari B, Kumar S, Pandey S, et al. Changing trends of culture-positive typhoid fever and antimicrobial susceptibility in a tertiary care North Indian Hospital over the last decade. Indian J Med Microbiol. 2018 Jan 1;36(1):70–6. https://doi.org/10.4103/ijmm.IJMM_17_412
- Khanal B, Sharma SK, Bhattacharya SK, Bhattarai NR, Deb M, Kanungo R. Antimicrobial susceptibility patterns of Salmonella enterica serotype typhi in eastern Nepal. J Health Popul Nutr. 2007 Mar;25(1):82.
- Zakir M, Khan M, Umar MI, Murtaza G, Ashraf M, Shamim S. Emerging trends of multidrug-resistant (MDR) and extensively drug-resistant (XDR) Salmonella typhi in a tertiary care Hospital of Lahore, Pakistan. Microorganisms. 2021 Nov 30;9(12):2484. https://doi.org/10.3390/microorganisms9122484
- Fatima G, Kazmi SS, Kainat S. XDR/MDR Salmonella: an experience from a tertiary care hospital, Karachi, Pakistan. Int J Infect Dis. 2020 Dec 1;101:37. https://doi.org?10.1016/j.ijid.2020.09.131
- Qamar FN, Yousafzai MT, Dehraj IF, Shakoor S, Irfan S, Hotwani A, et al. Antimicrobial resistance in typhoidal Salmonella: surveillance for enteric fever in Asia project, 2016–2019. Clin Infect Dis. 2020 Nov 1;71(Supplement_3):S276–84. https://doi.org/10.1093/cid/ciaa1323
- Park SE, Pham DT, Boinett C, Wong VK, Pak GD, Panzner U, et al. The phylogeography and incidence of multi-drug resistant typhoid fever in sub-Saharan Africa. Nat Commun 2018 Nov 30;9(1):5094. https://doi.org/10.1038/s41467-018-07370-z
- Batool A, Yunus N, Yaqoob A, Lone D, Khalid A, Ejaz H, et al. Prevalence of multi-drug resistant and extensively drug-resistant Salmonella enterica serovar typhi recovered from pediatrics’ septicemia patients in Lahore. Pak J Med Health Sci. 2021;15(4):843–5.
- Ejaz A, Khawaja A, Fatima K, Alavi N, Asif M. Frequency and antimicrobial resistance patterns of Salmonella enterica isolates in a tertiary care setting. Pak J Health Sci. 2022 May 26;16(05):11–3. https://doi.org/10.53350/pjmhs2216511
- Jain S, Chugh TD. Antimicrobial resistance among blood culture isolates of Salmonella enterica in New Delhi. J Infect Dev Ctries. 2013 Nov 15;7(11):788–95. https://doi.org/10.3855/jidc.3030
- Ramachandran A, Shanthi M, Sekar U. Detection of blaCTX-M extended spectrum beta-lactamase producing Salmonella enterica serotype typhi in a tertiary care centre. J Clin Diagn Res. JCDR. 2017 Sep;11(9):DC21. https://doi.org/10.7860/JCDR/2017/30150.10637
- Chen HM, Wang Y, Su LH, Chiu CH. Nontyphoid Salmonella infection: microbiology, clinical features, and antimicrobial therapy. Pediatr Neonatol. 2013 Jun 1;54(3):147–52. https://doi.org/10.1016/j.pedneo.2013.01.010
- Ali A, Ali HA, Shah FH, Zahid A, Aslam H, Javed B. Pattern of antimicrobial drug resistance of Salmonella typhi and paratyphi A in a Teaching Hospital in Islamabad. J Pak Med Assoc. 2017 Mar 1;67(3):375–9.
- Qamar FN, Azmatullah A, Kazi AM, Khan E, Zaidi AK. A three-year review of antimicrobial resistance of Salmonella enterica serovars typhi and paratyphi A in Pakistan. J Infect Dev Ctries. 2014 Aug 13;8(08):981–6. https://doi.org/10.3855/jidc.3817
- Lee CJ, Su LH, Huang YC, Chiu CH. First isolation of ciprofloxacin-resistant Salmonella enterica serovar typhi in Taiwan. J Microbiol Immunol Infect. 2013 Dec 1;46(6):469–73. https://doi.org/10.1016/j.jmii.2013.01.002
- Sjölund-Karlsson M, Joyce K, Blickenstaff K, Ball T, Haro J, Medalla FM, et al. Antimicrobial susceptibility to azithromycin among Salmonella enterica isolates from the United States. Antimicrob Agents Chemother. 2011 Sep;55(9):3985–9. https://doi.org/10.1128/aac.00590-11
