Original Article
VOLUME: 37 | ISSUE: 2 | Jun 30, 2021 | PAGE: (93 - 99) | DOI: 10.51441/BioMedica/5-266
Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers
Authors: Mehnaz Munir , Hamza Nadeem Malik , Muhammad Jareer Alam , Ammara Arif , Fiza Khalid
Article Info
Authors
Mehnaz Munir
FCPS Resident - Department of Community Medicine, Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore - Pakistan.
Hamza Nadeem Malik
Final Year MBBS Student - Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore - Pakistan.
Muhammad Jareer Alam
Final Year MBBS Student - Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore - Pakistan.
Ammara Arif
Final Year MBBS Student - Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore - Pakistan.
Fiza Khalid
Final Year MBBS Student - Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore - Pakistan.
Publication History
Received: February 04, 2021
Revised: April 10, 2021
Accepted: June 02, 2021
Published: June 30, 2021
Abstract
Background and Objective: Obesity leads to multiple complications that in turn increase mortality worldwide. There is a rapid rise in obesity in the last decade, especially among physicians. The objective of this study was to find out the frequency and relationship of obesity with socio-economic factors among faculty of a local medical college in Lahore, Pakistan.
Methods: A descriptive cross-sectional study was conducted on 162 medical and paramedical staff of Fatima Memorial College of Medicine and Dentistry, Lahore for a duration of 7 months from February 2019 to August 2019. Data were collected by filling the questionnaires and standard tools were used for height and weight measurement. Overweight/obesity was defined as a body mass index of ≥25 kg/m2.
Results: In this study, out of 86 males and 76 females, the majority of the respondents were between the ages of 21 and 35 years. Seventy three (45.1%) and thirty (18.5%) respondents were overweight and obese, respectively. Out of a total 162 subjects, 38 (24%) were hypertensive and 18 (11%) were suffering from diabetes. There was a statistically significant association of obesity with age (p < 0.05), marital status (p < 0.001), family history of obesity (p < 0.001), and smoking (p < 0.05).
Conclusion: Risk factors like age, marital status, family history of obesity, and smoking have a strong correlation with obesity in faculty members of a medical school.
Keywords: Obesity, Body mass index, Lifestyle, Risk factors, Overweight, Socio-demographic factors.
Pubmed Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid. Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers. BioMedica. 2021; 30 (June 2021): 93-99. doi:10.51441/BioMedica/5-266
Web Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid. Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers. https://biomedicapk.com/articles/online_first/266 [Access: July 03, 2024]. doi:10.51441/BioMedica/5-266
AMA (American Medical Association) Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid. Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers. BioMedica. 2021; 30 (June 2021): 93-99. doi:10.51441/BioMedica/5-266
Vancouver/ICMJE Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid. Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers. BioMedica. (2021), [cited July 03, 2024]; 30 (June 2021): 93-99. doi:10.51441/BioMedica/5-266
Harvard Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid (2021) Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers. BioMedica, 30 (June 2021): 93-99. doi:10.51441/BioMedica/5-266
Chicago Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid. "Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers." 30 (2021), 93-99. doi:10.51441/BioMedica/5-266
MLA (The Modern Language Association) Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid. "Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers." 30.June 2021 (2021), 93-99. Print. doi:10.51441/BioMedica/5-266
APA (American Psychological Association) Style
Mehnaz Munir, Hamza Nadeem Malik, Muhammad Jareer Alam, Ammara Arif, Fiza Khalid (2021) Body Mass Index and its Relation with Socio-Demographic Factors among Healthcare Workers. , 30 (June 2021), 93-99. doi:10.51441/BioMedica/5-266
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 37(2):93-99
ORIGINAL ARTICLE
Body mass index and its relation with socio-demographic factors among healthcare workers
Mehnaz Munir1*, Hamza Nadeem Malik2, Muhammad Jareer Alam2, Ammara Arif2, Fiza Khalid2
Received: 04 February 2021 Revised date: 10 April 2021 Accepted: 02 June 2021
Correspondence to: Mehnaz Munir
*Department of Community Medicine, Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore, Pakistan.
Email: mehnaz.munir@yahoo.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Obesity leads to multiple complications that in turn increase mortality worldwide. There is a rapid rise in obesity in the last decade, especially among physicians. The objective of this study was to find out the frequency and relationship of obesity with socio-economic factors among faculty of a local medical college in Lahore, Pakistan.
Methods:
This descriptive cross-sectional study recruited 162 medical and paramedical staff of Fatima Memorial College of Medicine and Dentistry, Lahore for a duration of 7 months from February 2019 to August 2019. Data were collected by filling the questionnaires and standard tools were used for height and weight measurement. Overweight/obesity was defined as a body mass index of ≥25 kg/m2.
Results:
In this study, the majority of the respondents were between the ages of 21 and 35 years. There were 86 males and 76 females. Seventy-three (45.1%) and thirty (18.5%) respondents were overweight and obese, respectively. Out of a total of 162 subjects, 38 (24%) were hypertensive and 18 (11%) were suffering from diabetes. There was a statistically significant association of obesity with age (p < 0.05), marital status (p < 0.001), family history of obesity (p < 0.001), and smoking (p < 0.05).
Conclusion:
Risk factors like age, marital status, family history of obesity, and smoking have a strong correlation with obesity in faculty members of a medical school.
Keywords:
Obesity, body mass index, lifestyle factors, risk factors, overweight, socio-demographic factors.
Introduction
According to World Health Organization (WHO), overweight and obese are classified as having a body mass index (BMI) from 25 to 29.9 kg/m2 and ≥30.0 kg/m2, respectively. Obesity is now considered as an epidemic with the number of obese people in 2014 almost twice as in 1980. According to WHO, overweight and obese adults reached almost 1.9 billion and 600 million, respectively [1].
Obesity is the leading cause of mortality and morbidity. It is estimated that the obesity is the leading cause of 2.6 million deaths and 2.3% of many systemic diseases worldwide obesity [2,3]. Not every obese person develops chronic complications. In this regard, body fat distribution, especially intra-abdominal adipose tissue is a key factor of metabolic syndrome including atherosclerosis, thromboembolism, and vascular inflammatory abnormalities, increasing the risk of Type 2 diabetes and cardiovascular disease [4].
Obesity is emerging as an epidemic in Pakistan as it copes with the dual burden of non-communicable diseases such as diabetes mellitus, hypertension, ischemic heart disease (IHD), etc. as well as communicable/infectious diseases [5]. There is a marked increase in the prevalence of obesity over the last few years; according to the National Nutrition Survey of Pakistan 2018, the prevalence of overweight and obesity in urban areas was 26.5% and 17.2%, respectively, among women of reproductive age while the Pakistan Demographic Health Survey 2017-2018 reported 30% of Pakistani population being overweight, and 22% obese [6,7]. Obesity among doctors and paramedical staff is increasing to an alarming level [8].
The WHO aims to halt the rise in obesity by 2025 which is unlikely to be attained without concerted action and further research. The increasing number of fast-food chains and westernized dietary habits seem to be the major cause of the increasing prevalence of obesity [9]. Obesity can be prevented by regular exercise and increasing the eating frequency of relatively small caloric meals as compared to taking a large meal with very high calories at a single time [10].
This study was carried out to determine the frequency of obesity and its relationship with lifestyle risk factors among physicians and paramedic staff working at Fatima Memorial College of Medicine and Dentistry (FMCM&D) Lahore, Pakistan them.
Methods
A descriptive cross-sectional study was conducted at FMCM&D, Lahore, Pakistan from February 2019 to August 2019. Probability systematic random sampling technique was employed by getting the list of regular employees working in FMCM&D from the human resource department. Total 162 physicians and paramedic staff were chosen as participants, considering the prevalence of the disease as 14% [5].
Employees of both genders between the age range of 18 and 69 years were included in the study. Pregnant women, part time employees, and participants that were not willing to participate in the study were excluded from this study.
Data collection was started after the approval from the institutional ethical review board and written informed consent from each participant reassuring full confidentiality of data, was obtained. Self-structured questionnaires were filled by interviewing the participants. Weight and height using a digital weighing scale and inches tape with 0.5 kg and 1cm margin of error, respectively, were measured.
Statistical analysis
Variables like gender, age, education, marital status, income per capita, physical activity (minimum 30 minutes’ walk), smoking, sleep, and alcohol habits were considered to be independent variables, and obesity was considered as the dependent variable. For the sake of simplicity, a person with a BMI equal to or more than 25 was considered as overweight or obese in this study. The tools of measurement were a weighing machine for measuring weight, measuring tape for height measurement, and a questionnaire. For analysis, quantitative variables were calculated by mean and standard deviation and for qualitative variables frequency and percentages were calculated. Bivariate analysis for qualitative variables was done by Chi-square test and Fischer’s exact test (for smaller frequencies) was applied, considering p-value less than 0.05 to be statistically significant.
Results
This cross-sectional study included 162 participants, out of which, 69 (43%) participants were aged between 21 and 35 years and the mean age among males and females was 41.17 ± 12.52 years and 37.58 ± 10.22 years, respectively. A total of 86 (57%) respondents were males and 76 (43%) were females. The majority of the participants were graduates (31%) whereas (59%) had post-graduate qualifications (Table 1). Also, the mean weight and height among participants was 74.81 ± 10.97 kg and 1.70 ± 0.06 m for males and 67.19 ± 10.64 kg and 1.58 ± 0.11 m for females, respectively, and the mean BMI was 26.49 ± 4.99 kg/m2 (Figure 1), out of which 73 (45.1%) participants were overweight (BMI ≥ 25.00 kg/m2) (Table 1).
Most of the participants were married 128 (79%) while, 47 (29%) of respondents had family members more than 5, and 61 (38%) had an income per capita per month below 2,180 PKR. Thirty-eight (24%) out of a total of 162 candidates were hypertensive and 18 (11%) were suffering from diabetes. Among risk factors, 73 (45%) participants had some regular physical activity, only 24 (15%) were smokers, and only 1 (1%) stated he consumed alcohol. The majority 106 (65.4%) of the participants complained of sleep deprivation and stress was present in 104 (64%). Evaluating the sedentary lifestyle, 50 (31%) admitted they sat more than 6 hours/day at work. Family history of obesity was present in 43% (69) participants and the majority of participants 152 (94%) used to take 3 or less than 3 meals per day (Table 1).
There appeared to be a relationship between increased BMI with increasing age (p = 0.047) (Figure 2). Gender and educational level were not linked with BMI (p = 0.229 & 0.083 respectively), however, most married participants (91) were obese (p = 0.000), while there was no association of BMI with income per capita (p = 0.682) and regular physical activity (p = 0.076) found in the study. The BMI was higher in smokers as compared to nonsmokers (p = 0.029). There is no statistical association found between the number of sleeping hours (p = 0.216), level of stress (p = 0.470), sitting hours (p = 0.669), alcohol use (p = 1.000), and having three meals per day (p = 0.172), and BMI. However, there was a direct relationship between BMI and family history of obesity (p = 0.000) (Table 2).
Discussion
Pakistan had a reported frequency of 46%-48% of obese people and ranked 9 out of 188 according to the Global Burden of Disease statistics [11,12]. This study showed that 64% of participants were either overweight or obese and there was a statistically significant relationship of young age, marital status, history of smoking, and family history of obesity. However, obesity was not related to gender, educational status, income per capita, physical activity, sleep, stress, sitting hours during work, alcohol use, and the number of meals per day.
This study fits into the trend that obesity is a growing problem, emerging at an even younger age in our population. The results revealed a statistically significant association between age and obesity (p = 0.047), with people grouped between the age of 36 and 50 years were most likely to be obese. Traditionally in developing countries, obesity was seen to be highest at the age of 55 years for women and 45 years for men [13]. This is a major concern, as South Asians are already at higher risk for IHD at a younger age than other populations [14].
Table 1. Frequency distribution of study subjects according to clinical and socio-demographic factors.
| Characteristics | Frequency | Percent | |
|---|---|---|---|
| Age | 21-35 years | 69 | 42.6 |
| 36-50 years | 64 | 39.5 | |
| 51-65 years | 26 | 16 | |
| 66 and above years | 3 | 1.9 | |
| Gender | Male | 86 | 53.1 |
| Female | 76 | 46.9 | |
| Level of education | Primary | 5 | 3.1 |
| Matric / Intermediate | 11 | 6.8 | |
| Graduate | 50 | 30.9 | |
| Post-graduate | 96 | 59.3 | |
| BMI | Underweight (<18.5 kg/m2) | 6 | 3.7 |
| Normal (18.5-24.99 kg/m2) | 53 | 32.7 | |
| Overweight (25.0-29.9 kg/m2) | 73 | 45.1 | |
| Obesity (≥30 kg/m2) | 30 | 18.5 | |
| Marital status | Married | 128 | 79 |
| Unmarried | 33 | 20.4 | |
| Divorced/widowed | 1 | 0.6 | |
| Family members | ≤5 members | 115 | 71 |
| >5 members | 47 | 29 | |
| Income/capita/month (≥2180 PKR) | 101 | 62.3 | |
| Hypertension | 38 | 23.5 | |
| Diabetes | 18 | 11.1 | |
| Regular physical activity | 73 | 45.1 | |
| Smoking | 24 | 14.8 | |
| Alcohol use | 1 | 0.6 | |
| Sleep/day (≥7 hours) | 56 | 34.6 | |
| Stress | 104 | 64.2 | |
| Hours of sitting at work (>6 hours) | 50 | 30.9 | |
| Family history of obesity | 69 | 42.6 | |
| Meals per day (>3 meals) | 10 | 6.2 | |
Many studies showed that women were more likely to be overweight or obese than men in the developing countries [13]. This is somewhat different from this research, which showed an almost equal division of obesity amongst men and women (p = 0.229). However, another study showed an increasing tendency of obesity amongst the male population [15].
Although the literacy rate plays a very important role in the prevalence of obesity, but results showed no relationship (p = 0.083). However, another study endorsed that high educational status was related to obesity [16]. A possible reason for this is that people with a low level of academic achievement are more likely to engage in manual labor and hence are more likely to have a lean body type while higher education demands prolonged sitting time [16].
There was a significant correlation between marital status and obesity with married people most likely to be obese (p = 0.000). Eighty-eight percent of our obese participants were married. This was also demonstrated in a study on Chinese twins and possible reasons cited for this association included a possible reduction in weight perception or increase in appetite after marriage [17].
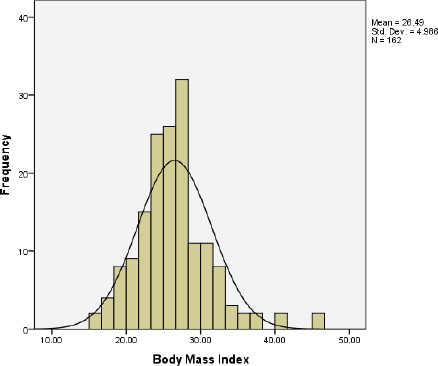
Figure 1. Frequency distribution of study subjects according to BMI in kg/m2.
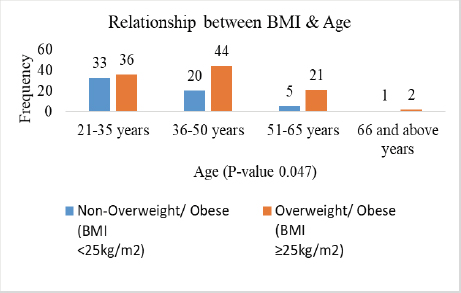
Figure 2. Relationship of BMI (kg/m2) with age (years).
Also, in this study, 61.2% of the participants categorized as obese had a higher per capita income but did not show a significant relationship (p = 0.682). However, Dinsa et al. [16] showed that higher income and higher educational status were related to a higher prevalence of obesity.
Obesity is associated with multiple chronic diseases. Weight is gained through a combination of excessive caloric intake and lack of physical activity. The research indicates that physical activity played a significant role in the prevention of obesity [18]. Regular moderate to high-intensity physical activity is recommended in the management of obesity [19]. While our study failed to find a significant relationship between physical activity and obesity (p = 0.076), the results do indicate that 54.20% of non-obese participants engaged in regular physical activity compared to 39.80% of obese participants, indicating that regular physical activity is somewhat helpful in staving off weight gain. Moreover, another study supported our results [20].
Other lifestyle factors associated with obesity include smoking, sleep, and stress. Smoking was observed to have a protective role in developing obesity (p = 0.029). Nicotine and tobacco contained in cigarettes were associated with weight loss. Smoking cessation was often associated with a moderate degree of weight gain [21,22].
Table 2. Relationship between BMI and socio-demographic and risk factors.
| Socio-demographic & risk factors | BMI | p value | |||
|---|---|---|---|---|---|
| Non-obese (BMI < 25 kg/m2) | Obese (BMI ≥ 25 kg/m2) | Total | |||
| Relationship between BMI and socio-demographic factors | |||||
| Age | 21-35 years | 33 (55.9%) | 36 (35.0%) | 69 (42.6%) | 0.047 (Chi square) |
| 36-50 years | 20 (33.9%) | 44 (42.7%) | 64 (39.5%) | ||
| 51-65 years | 5 (8.5%) | 21 (20.4%) | 26 (16.0%) | ||
| ≥66 years | 1 (1.7%) | 2 (1.9%) | 3 (1.9%) | ||
| Gender | Male | 35 (59.3%) | 51 (49.5%) | 86 (53.1%) | 0.229 |
| Female | 24 (40.7%) | 52 (50.5%) | 76 (46.9%) | ||
| Education | Up to intermediate | 9 (15.3%) | 7 (6.8%) | 16 (9.9%) | 0.083 |
| Graduate & above | 50 (84.7%) | 96 (93.2%) | 146 (90.1%) | ||
| Marital status | Married | 37 (62.7%) | 91 (88.3%) | 128 (79.0%) | 0.000 (Chi square) |
| Single | 22 (37.3%) | 12 (11.7%) | 34 (21.0%) | ||
| Income/capita/month | <2180 PKR | 21 (35.6%) | 40 (38.8%) | 61 (37.7%) | 0.682 |
| ≥2180 PKR | 38 (64.4%) | 63 (61.2%) | 101 (62.3%) | ||
| Relationship between BMI and risk factors | |||||
| Regular physical activity | 32 (54.2%) | 41 (39.8%) | 73 (45.1%) | 0.076 | |
| Smoking | 4 (6.8%) | 20 (19.4%) | 24 (14.8%) | 0.029 | |
| Sleep/day | <7 hours | 35 (59.3%) | 71 (68.9%) | 106 (65.4%) | 0.216 |
| ≥7 hours | 24 (40.7%) | 32 (31.1%) | 56 (34.6%) | ||
| Stress present | 40 (67.8%) | 64 (62.1%) | 104 (64.2%) | 0.470 | |
| Sitting work | ≤6 hours | 42 (71.2%) | 70 (68.0%) | 112 (69.1%) | 0.669 |
| >6 hours | 17 (28.8%) | 33 (32.0%) | 50 (30.9%) | ||
| Family history of obesity | 13 (22.0%) | 56 (54.4%) | 69 (42.6%) | 0.000 | |
| BMI | p value | ||||
| Non obese | Obese | Total | |||
| Alcohol use | 0 (0.0%) | 1 (1.0%) | 1 (0.6%) | 1.000 | |
| Meals/day | ≤3 meals | 53 (89.8%) | 99 (96.1%) | 152 (93.8%) | 0.172 |
| >3 meals | 6 (10.2%) | 4 (3.9%) | 10 (6.2%) | ||
Traditionally, obesity had been associated with shorter sleep duration. Obese individuals experienced more fatigue as a result of carrying more weight. as compared to normal individuals. However, this study showed the opposite results (p = 0.216) [23].
Stress affects self-regulation and can lead to overeating and consumption of calorie-dense food. It also leads to a decrease in physical activity and sleep. Besides, due to weight stigmatization, obesity itself can also cause stress [24]. But, this study did not show any association (p = 0.47). Concordantly, sitting hours of work (p = 0.669) were not related to increased BMI, supported by another study [20]. However, sitting hours and obesity have direct relation, as a study shows a 62% increase in obesity for the daily ≥8 hour increment of sitting in working hours as compared to <4 hours per day [25].
In addition to lifestyle and environmental factors affecting weight, there was also a genetic predisposition toward obesity in certain individuals [26]. Genome-wide studies have identified more than 300 single nucleotide polymorphism traits linked with BMI, waist to hip ratio, and other adiposity traits [27]. Clinically, this is exhibited in the form of a strong family history of obesity. Our study also found a significant correlation between family history of obesity and obesity (p = 0.000).
Alcohol consumption, in contrast, can lead to weight gain. But in this study alcohol consumption was not related (p = 0.576) to obesity. This is probably due to religious prohibitions leading to Muslims avoiding alcohol. However, the stigma associated with its consumption can also lead to underreporting of its use [28].
In this study, the number of meals was not related to obesity (p = 0.172), in contrast, to a study done by Peltzer et al. [20] in which irregular meals and multiple snacking was associated with obesity.
Lifestyle modifications such as increasing physical activity and decreasing sedentary habits could diminish some of the genetic predispositions with obesity [26]. All of this has significant public health implications as targeted interventions at risk factors can help reduce weight and thus assist in both prevention and management of chronic diseases such as diabetes mellitus, metabolic syndromes, IHD, etc. Government, policy-making bodies, communities, and health care professionals including general practitioners, nursing staff, rural health workers, etc. all need to play their part. There should be an increase in the need for better surveillance and lifestyle interventions aimed at major causes of obesity such as calorie-dense food intake and physical activity. Primary and secondary prevention of obesity helps reduce the complication of obesity among smokers, married people, and those with a family history of obesity.
Conclusion
Increasing age, marital and smoking status, and family history of obesity are significant risk factors of obesity in our population. Targeting these determinants can play a very important role in reducing the prevalence of obesity by using effective interventional measures.
Limitations of the study
This study had some limitations. First, the relatively small sample size was used in a major urban city so our results cannot be generalized for the entire population of Pakistan. Secondly, there might be an inter-observer error in measuring weights and heights to calculate BMI ratios to categorize people as overweight or obese.
Acknowledgement
The authors would like to thank the the staff members of FMCM&D Lahore for their cooperation in the data collection.
Conflict of interest
None to declare.
Grant support & financial disclosure
None to disclose.
Ethical approval
The protocol of this research was approved by the Institutional Ethical Review Board of Fatima Memorial College of Medicine and Dentistry Lahore (Letter No. FMH-01-2019-IRB-708-M). All participants have agreed and signed the informed consent form.
Author’s contribution
MMr: Conception and design of the study, critical analysis with intellectual input, analysis and interpretation of data.
HNM: Analysis and interpretation of data
MJA, AA, FK: Acquisition of data, drafting the manuscript, conception and design of the study
All AUTHORS: Approval of the final version of the manuscript to be published.
Author details
Mehnaz Munir1, Hamza Nadeem Malik2, Muhammad Jareer Alam2, Ammara Arif2, Fiza Khalid2
- FCPS Resident - Department of Community Medicine, Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore, Pakistan
- Final Year MBBS Student - Fatima Memorial Hospital/College of Medicine & Dentistry, Lahore, Pakistan
References
- World Health Organization. Obesity; 2015 [cited 2015 June 26]. Available from: http://www.who.int/topics/obesity/en/
- Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161–6. https://doi.org/10.21037/atm.2017.03.107
- Dare S, Mackay DF, Pell JP. Relationship between smoking and obesity: a cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS One. 2015;10(4):e0123579. https://doi.org/10.1371/journal.pone.0123579
- Han TS, Lean ME. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovas Dis. 2016;5(3):2048004016633371. https://doi.org/10.1177/2048004016633371
- Tanzil S, Jamali T. Obesity, an emerging epidemic in Pakistan-a review of evidence. J Ayub Med Coll Abbottabad. 2016;28(3):597–600.
- National Institute of Population Studies (NIPS) [Pakistan] and ICF. Pakistan demographic and health survey 2017-18. Islamabad, Pakistan, and Rockville, Maryland, USA: NIPS and ICF; 2019 [cited 2021 Jan]. Available from: https://dhsprogram.com/pubs/pdf/FR354/FR354.pdf
- Government of Pakistan. National Nutrition Survey 2018 - key findings report. United Nations Children’s Fund (UNICEF) Pakistan; 2019 [cited 2021 Jan]. Available from: https://www.unicef.org/pakistan/reports/national-nutrition-survey-2018-key-findings-report
- Ahmad W, Taggart F, Shafique MS, Muzafar Y, Abidi S, Ghani N, et al. Diet, exercise and mental-wellbeing of healthcare professionals (doctors, dentists and nurses) in Pakistan. Peer J. 2015;3:e1250. https://doi.org/10.7717/peerj.1250
- Chan M. Obesity and diabetes: the slow-motion disaster. The Milbank Q. 2017;95(1):11. https://doi.org/10.1111/1468-0009.12238
- House B, Shearrer G, Miller S, Pasch KE, Goran M, Davis JN. Increased eating frequency linked to decreased obesity and improved metabolic outcomes. Int J Obes. 2015;39(1):136–40. https://doi.org/10.1038/ijo.2014.81
- Ali AA, Yamin F, Kumar S, Khan N, Paracha H, Batool S. Screening of BMI in biomechenical parameters of gait in young adults. Indian J Physiother Occup Ther. 2017; 11(3):104–8. https://doi.org/10.5958/0973-5674.2017.00083.1
- World Health Organization. World Health Organization obesity and overweight fact sheet; 2016 [cited 2021 Jan]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. https://doi.org/10.1016/S0140-6736(14)60460-8
- Ahmed ST, Rehman H, Akeroyd JM, Alam M, Shah T, Kalra A, et al. Premature coronary heart disease in South Asians: burden and determinants. Curr Atheroscler Rep. 2018;20(1):1–8. https://doi.org/10.1007/s11883-018-0706-1
- Zhang H, Xu H, Song F, Xu W, Pallard-Borg S, Qi X. Relation of socioeconomic status to overweight and obesity: a large population-based study of Chinese adults. Ann Hum Biol. 2017;44(6):495–501. https://doi.org/10.1080/03014460.2017.1328072
- Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev. 2012;13(11):1067–79. https://doi.org/10.1111/j.1467-789X.2012.01017.x
- Liao C, Gao W, Cao W, Lv J, Yu C, Wang S, et al. Association of educational level and marital status with obesity: a study of chinese twins. T Twin Res Hum Genet. 2018;21(2):126–35. https://doi.org/10.1017/thg.2018.8
- Chin SH, Kahathuduwa C, Binks M. Physical activity and obesity: what we know and what we need to know. Obes Rev. 2016;17(12):1226–44. https://doi.org/10.1111/obr.12460
- Audet M, Baillot A, Vibarel-Rebot N. Female obesity and physical activity: a better understanding of the stakes linked to stigmatization. Santé Publique. 2016;1(HS):127–34.
- Peltzer K, Pengpid S. The association of dietary behaviors and physical activity levels with general and central obesity among ASEAN university students. AIMS Public Health. 2017;4(3):301–6. https://doi.org/10.3934/publichealth.2017.3.301
- Kabat GC, Heo M, Allison M, Johnson KC, Ho GY, Tindle HA, et al. Smoking habits and body weight over the adult lifespan in postmenopausal women. Am J Prev Med. 2017;52(3):e77–e84. https://doi.org/10.1016/j.amepre.2016.10.020
- Calarco CA, Lee S, Picciotto MR. Access to nicotine in drinking water reduces weight gain without changing caloric intake on high fat diet in male C57BL/6J mice. Neuropharmacology. 2017;123:210–20. https://doi.org/10.1016/j.neuropharm.2017.06.012
- St-Onge MP. Sleep–obesity relation: underlying mechanisms and consequences for treatment. Obes Rev. 2017;18:34–9. https://doi.org/10.1111/obr.12499
- Razzoli M, Pearson C, Crow S, Bartolomucci A. Stress, overeating, and obesity: insights from human studies and preclinical models. Neurosci Biobehav Rev. 2017;76:154–62. https://doi.org/10.1016/j.neubiorev.2017.01.026
- Bullock VE, Griffiths P, Sherar LB, Clemes SA. Sitting time and obesity in a sample of adults from Europe and the USA. Ann Hum Biol. 2017;44(3):230–6. https://doi.org/10.1080/03014460.2016.1232749
- Moon J-Y, Wang T, Sofer T, North KE, Isasi CR, Cai J, et al. Objectively measured physical activity, sedentary behavior, and genetic predisposition to obesity in US Hispanics/Latinos: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes. 2017;66(12):3001–12. https://doi.org/10.2337/db17-0573
- Goodarzi MO. Genetics of obesity: what genetic association studies have taught us about the biology of obesity and its complications. Lancet Diabetes Endocrinol. 2018;6(3):223–36. https://doi.org/10.1016/S2213-8587(17)30200-0
- Traversy G, Chaput J-P. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4(1):122–30. https://doi.org/10.1007/s13679-014-0129-4
