Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 40(1):18-25
ORIGINAL ARTICLE
Turmeric gel as an alternative non-vital pulpotomy medicament in primary teeth- a randomized controlled trial
Mashal Mazhar1*, Shazia Naz2, Ambreen Zahra3, Nazia Bashir4, Rabia Dastgeer5
Received: 25 January 2024 Revised date: 02 March 2024 Accepted: 15 March 2024
Correspondence to: Mashal Mazhar
*Senior Demonstrator, Department of Operative Dentistry, University College of Dentistry, The University of Lahore, Lahore, Pakistan.
Email: mashalmazhar91@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Formocresol is a gold standard medicament in both vital and non-vital pulpotomies due to its potent antibacterial potential but, it has a controversial nature due to its side effects. Therefore, the demand for natural alternatives of Formocresol as a pulp dressing material, with few or no side effects, became imperative. The purpose of the study was to introduce turmeric gel as a non-vital pulpotomy (NVP) medicament in primary teeth by evaluating its antibacterial effect against Streptococcus mutans and Lactobacillus acidophilus.
Methods:
It was a multiarm parallel randomized controlled trial in which sixty patients aged between 4 and 8 years, each containing at least one non-vital primary molar, were selected and randomly divided into group A (Formocresol) and group B (Turmeric gel). NVP was performed by removing the coronal necrotic pulp. Sterile paper points were dipped in the root canals and taken to the laboratory. Cotton pellets soaked in the respective medicaments were placed over the root canal orifices and filled temporarily. Patients were recalled after 1 week. Samples were again taken, and the tooth was restored. A comparison between bacterial count at baseline and after 1 week of treatment was made and expressed as Colony-Forming Units/ml. Data were entered and analyzed by using Statistical Package for Social Sciences version 25.0.
Results:
There was a significant reduction in median S. mutans and L. acidophilus bacterial count in each group after 1 week of treatment (p < 0.001). Formocresol showed a higher average reduction than turmeric gel. However, statistically, the difference was insignificant indicating that both the medicaments possessed comparable antibacterial effects.
Conclusion:
Turmeric gel was found as an effective alternative to Formocresol for its use as a non-vital pulpotomy medicament.
Keywords:
Formocresol, turmeric (curcuma), pulpotomy, non-vital, primary (deciduous) teeth, randomized controlled trial.
Introduction
Preservation of cariously exposed primary teeth till their physiological exfoliation is one of the major problems in pediatric dentistry.1 If primary teeth are left untreated, bacterial invasion from the coronal to radicular pulp and then beyond the root canal into the adjacent soft tissue occurs. This leads to an aggressive and painful inflammatory reaction rendering the tooth irreversibly inflamed or non-vital.2 Retention of primary teeth is imperative as their untimely loss can lead to undesirable consequences.3
Bacteria present in primary teeth with necrosed pulp are poly-microbial, predominantly Streptococcus mutans (S. mutans) and Lactobacillus acidophilus (L. acidophilus).4 Streptococcus mutans is commonly regarded as the dental caries initiator,5 and L. acidophilus as the dental caries progressor.6
Treatment of choice to save cariously exposed non-vital yet restorable primary teeth is pulpectomy, as the damaged pulp is unable to heal itself.7 Despite its high success rate, pulpectomy is often impractical in some pediatric patients such as, when there is difficulty in obtaining adequate access due to small mouth openings in children, severe gag-reflex, possible damage to permanent tooth germ, complex (ribbon-shaped) non-negotiable root canals, and limited patient’s cooperation.1,7 Extraction is another option for the management of non-vital primary teeth, where the tooth is non-restorable due to extensive caries and severe mobility.8
Non-vital pulpotomy (NVP) also known as mortal pulpotomy, is regarded as a quick, least invasive alternative with predictable outcomes for the decayed non-vital, yet restorable primary teeth. NVP is performed when neither pulpectomy nor extraction is feasible. In NVP, the infected non-vital radicular pulp is dressed with a strong antiseptic material that combats infection, mummify, fix, and sterile the necrotic pulp tissue so that it can stay in situ till the tooth exfoliates.9
Several conventional materials have been used in pulpotomy, commonly mineral trioxide aggregate,10 Glutaraldehyde, and Ferric sulfate. However, the “gold standard” material due to its potent antibacterial and fixative properties is Formocresol. Its constituents, formaldehyde, and cresol, are responsible for harmful effects11 such as mutagenicity, carcinogenicity, allergenicity, systemic distribution,12 tissue changes in internal organs, and enamel defects in permanent successors.1 Due to the controversial nature of Formocresol, it seemed imperative to do research to find clearly and reproducibly safer, superior alternatives to Formocresol.11
Despite the advancements in modern medicine, a viable health alternative for large under-developed and underprivileged sections of the world continues to be traditional medicine.13 In dentistry, several herbal medicaments have been used in pulpotomy procedures in pediatric patients14 because of their wide therapeutic properties, minimum side effects, low cost, easy availability, and long-lasting therapeutic effects with the added benefit of minimum bacterial resistance.15
Turmeric (Curcuma longa) possesses potent antibacterial potential,16 being anti-inflammatory, analgesic, antioxidant, and anti-cariogenic.17 Turmeric has only been used in vital pulpotomy.18,19
There is a lack of international literature, and to the authors’ best knowledge, no evidence of local study has been found on the NVP procedure and medicaments used in this procedure.
There was a need for further analysis, research, and randomized controlled trials (RCTs) on turmeric to promote its usage in dental practice as an alternative to Formocresol and the applicability of the NVP procedure itself in local patients.
The study aimed to find a suitable herbal alternative (Turmeric gel), to replace the routinely used conventional medicament, Formocresol, in the NVP procedure with a hypothesis that there was no difference in the antibacterial effect of turmeric gel compared with gold standard Formocresol, against S. mutans and L. acidophilus, in NVP of primary molars in terms of average reduction of bacterial count (Colony-Forming Units/ml - CFU/ml).
Methods
It was a double-blinded, randomized controlled trial (Fig:1) The sample size in each group was 20. The study was conducted at the Pediatric Dentistry Department, Punjab Dental Hospital, Lahore, Pakistan, in collaboration with the Microbiology Department of Lahore General Hospital, Lahore. The study was done from October 2022 to February 2023. Forty cariously exposed non-vital primary molars from forty pediatric patients (one tooth from each patient) of both sexes aged between 4 and 8 years were selected from the Outpatient Department of Pedodontics, de’Montmorency College/Punjab Dental Hospital, Lahore. Ethical approval was obtained from the Institutional Ethical Review Committee and consent from the parents of the patients was taken before enrollment of the study participants.
The patients were randomly allocated into two groups using the lottery method. The participants were blinded to which medicament group they belonged.
Group A = Formocresol (control group, standard medicament) (n = 20)
Group B = Turmeric gel (n = 20)
Formocresol
Premade Formocresol (Tricresol & Formalin) was used composed of Tricresol 35%, Formaldehyde (40%) 19%, excipient additive 100% (PD, Switzerland, ISO9001/ISO9001_2000/ ISO13485/CE_MARK), (Universal Dental Pvt, Ltd).
Turmeric gel
Turmeric gel was self-prepared at the Institute of Microbiology and Molecular Genetics, Punjab University, Lahore, Pakistan. A total of 2 kgs of turmeric rhizomes were purchased from a local market in Lahore and verified by a taxonomist, Botany Department, Government College University, Lahore, Pakistan (voucher number: GC.Herb.Bot.3693). The rhizomes were then washed, cut, and sun-dried for 3 days then oven-dried at 60°C for 30 minutes, and then grounded into powdered form. Turmeric powder (180 g) was obtained which was then transferred into sterilization pouches and autoclaved at 121°C for 30 minutes. Approximately 170 g powder along with 550 ml distilled water was taken in a Soxhlet extractor. After 96 hours, ~30% aqueous turmeric extract was collected and filtered repeatedly through the Whatman No.1 filter paper. The obtained filtrate (Turmeric extract) was then mixed with 6% Sodium Carboxy-Methyl Cellulose (NaCMC) (Genevex Chem, Hyderabad, India) to form a gel. Four Vitamin C grounded tablets (500 mg of ascorbic acid per tablet) and 12 Vitamin E capsules (200 IU per capsule) (Evion, Martin Dow Pharmaceuticals, Ltd. Karachi, Pak) then added in 100 g of gel as antioxidants. The prepared gel had 21 days shelf-life.20
Preparation of cavity and NVP
For ease of procedure, local anesthesia with 2% lidocaine containing 1:100000 epinephrine was injected, and a rubber dam was applied. Cavity outline and caries removal were done using #330 pear-shaped carbide bur (Meisinger, Germany) using a high-speed handpiece with constant water spray. The pulp chamber was accessed, and de-roofing was done using non-end cutting steel straight fissure bur (Meisinger, Germany). Removal of the coronal pulp tissue (if any) was achieved with a sterile, sharp spoon excavator type-A (Humayun Dental Supplies, Pakistan).7
Sample collection
The samples were collected for in-vitro evaluation. One sample was taken from each root canal by dipping #20 sterile paper points 2-3 mm into the root canal for 10 seconds. These paper points were then immediately placed into plastic calibrated screw-capped tubes containing 5 ml of autoclaved Fluid Thioglycollate Transport Medium (CM0173 Oxoid, UK),21 labeled with laboratory code and transported to the laboratory as soon as possible.7,22
Placement of dressings
For group A (Formocresol), the radicular pulp was dressed with #4 (3 mm) cotton pellet which was dipped in respective medicament. For group B, approximately 3-4 mm of turmeric gel matching the size of #4 cotton pellets was placed over root canals’ orifices with plastic instrument type-A. The tooth was then restored temporarily with a thin layer of Cavit (Detax, Germany), followed by a thick hard mix of zinc oxide and eugenol type II (Shanghai New Century Dental Materials Co., Ltd). The patient was then recalled after 1 week. Again, sample collection was done and transported to the laboratory. In addition, the patient was clinically assessed according to criteria by Mohammad and Baroudi7.
Processing and culturing of bacterial samples
Blood agar (CM0055 Oxoid, UK) was used for culturing S. mutans and de Man, Rogosa, Sharpe (MRS) agar (CM0361 Oxoid, UK) was used for L. acidophilus. Culture media plates were prepared according to the manufacturer’s instructions by a laboratory technician. Tubes containing the specimen were vortexed for 60 seconds. 1 μl portion of the sample was taken with 1 μl disposable plastic loop (Oxoid, UK) and spread on respective culture media plates. The inoculated plates were then placed in an anaerobic jar with a gas pack (AN0025A Oxoid, UK) and incubated for 2 days (48 hours) at 37°C.7
Streptococcus mutans and L. acidophilus identification
Bacterial colonies were identified by the naked eye, Gram-staining, and catalase test. Further identification was done under a light microscope (Olympus CH-2) with 100× magnification.
Rapid bacterial identification kits and software
For species level identification, Analytical Profile Index kit (API 20 STREP kit, bioMérieux Ref 20 690), and API 50 CHL kit (bioMérieux Ref 50 410 and 50 300) were used for S. mutans and L. acidophilus identification respectively according to the company’s instructions. The results were entered in licensed API software with database V7.0 for S. mutans and V5.1 for L. acidophilus (bioMérieux apiwebTM identification software - Ref 40 011) for interpretation.
Counting of bacterial colonies
To quantify the antibacterial effect, S. mutans and L. acidophilus colonies counted with the naked eye were expressed as CFU/ml.
Statistical analysis
Data were entered in Statistical Package for Social Sciences® version 25. The study was set at 90% power and 95% confidence level with a 5% margin of error. The normality of data was assessed by the Shapiro-Wilk test. Mann-Whitney U test was used to compare the median reduction of bacterial count between the groups. Fisher’s exact test was used to compare clinical outcomes among different groups. A p ≤ 0.05 was considered as significant.
Results
Bacterial colonies of the S. mutans appeared grayish-white, smooth, glossy, and translucent with zones of alpha hemolysis (partial hemolysis with greenish-brown discoloration) on blood agar plates (Figure 2a). They were Gram-positive, catalase negative, and appeared cocci-shaped, present in pairs and chains, without spores under a light microscope (Figure 2b). Bacterial colonies of L. acidophilus appeared compact, smooth, medium, opaque, and white mucoid on the MRS agar plate (Figure 3a). They were Gram-positive, catalase catalase-negative and appeared as round-ended single, pairs, and chains of rods without spores under a light microscope (Figure 3b). Further biochemical testing using the API 20 STREP kit for S. mutans and API 50 CHL kit for L. acidophilus was done, and the results were analyzed through API software.
The data were not normally distributed according to Shapiro-Wilk test so the median bacterial count for both groups was calculated. Results of the Mann-Whitney U test showed statistically no significant difference in the average reduction of S. mutans bacterial count as well as L. acidophilus bacterial count among the groups. For analysis of the combined bacterial count among the groups, the data were normally distributed so the mean bacterial count for both the groups was calculated. Results of Mann-Whitney U test showed statistically no significant difference in the mean reduction of combined bacterial count among the groups (p = 0.640) (Table 1) indicating that the overall antibacterial effect of both the medicaments was similar. Clinical outcome was analyzed through Fisher’s exact test which revealed that there was a statistically insignificant difference in the clinical outcome among the groups (p = 0.487) (Table 2).
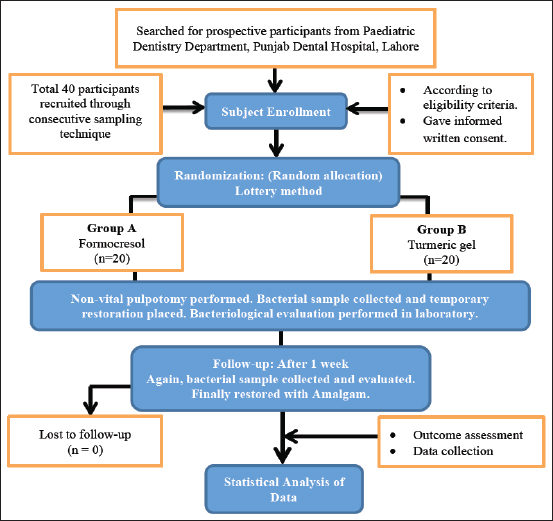
Figure 1. Study flow chart according to CONSORT guidelines.
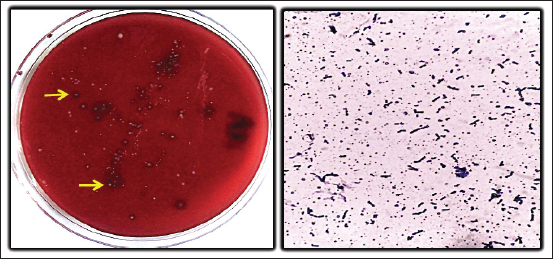
Figure 2. (a): Streptococcus mutans colonies on blood agar plate, (b): Microscopic view of S. mutans.
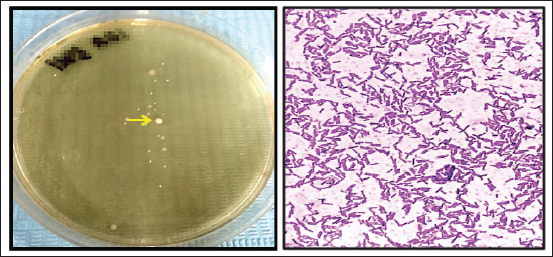
Figure 3. (a): Lactobacillus acidophilus on MRS agar plate, (b): Microscopic view of L. acidophilus.
Table 1. Comparison of mean reduction of combined bacterial count among group.
| Group | Mean reduction of overall bacterial count (CFU/ml) | |||
|---|---|---|---|---|
| Mean ± SD | Minimum | Maximum | p-value # | |
| Group A | 30,300 ± 14,060 | 13,000 | 60,000 | 0.640 |
| Group B | 29,300 ± 7,399 | 14,000 | 44,000 | |
Group A: Formocresol, Group B: Turmeric gel, #Mann-Whitney U test.
Discussion
The study was designed to evaluate the antibacterial effect of Formocresol (Group A), and turmeric gel (Group B) against S. mutans and L. acidophilus in pediatric NVP as bacteria are the main cause of tooth decay leading to irreversible damage and hence necrosis of tooth. A combined clinical laboratory study was performed to assess the clinical outcome as well as the antibacterial effect of each medicament.
Non-vital (Mortal) pulpotomy procedure was opted for in this study as it is often used as a quick, least invasive alternative for the decayed, irreversibly inflamed/non-vital, yet restorable primary teeth. It is performed when neither pulpectomy nor extraction is feasible.9 Pulpectomy is impractical in some pediatric patients with inadequate access, limited cooperation, and possible damage to permanent tooth germ.1,7 Extraction is another option but is an invasive procedure and can lead to space maintenance issues.23
The most significant finding of the present study was that both the medicaments showed a significant reduction of S. mutans and L. acidophilus bacterial count after 1 week of treatment. Statistically, there was no significant difference in the individual average reduction (p = 0.718 and 0.968) as well as combined mean reduction (p = 0.640) of S. mutans and L. acidophilus bacterial count among the groups. This indicated that both the medicaments possessed comparable overall antibacterial effects.
Table 2. Comparison between the effects of all three medicaments on the clinical outcome of non-vital primary teeth after 1 week (1st follow-up visit).
| Clinical findings after 1 week | Group A n = 20 (%) | Group B n = 20 (%) | p-value* |
|---|---|---|---|
| Post-operative pain | (+) 2 (10.0%) | (-) | 0.487 |
| Tenderness to percussion | (-) | (-) | |
| Gingival inflammation | (-) | (-) | |
| Draining sinus | (-) | (-) | |
| Increased mobility (Grade II and III) | (-) | (-) |
Group A: Formocresol, Group B: Turmeric gel, *Fisher’s exact test
+ (having signs and symptoms), - (without signs and symptoms).
In addition, in this study, Formocresol exhibited a higher antibacterial effect against S. mutans than L. acidophilus. Turmeric gel exhibited an equal antibacterial effect against both S. mutans and L. acidophilus. This finding adds up to the effectiveness of herbal medicament in irreversibly inflamed/necrotic primary teeth.
In the present study, the antibacterial effect of Formocresol was strong, especially against S. mutans and L. acidophilus. This finding is concomitant with other studies where Formocresol exhibited potent antibacterial and fixative properties,24,25 but as an intracanal medicament on extracted primary canines.
In dentistry, turmeric is famous for its inhibitory potential specifically against caries-causing bacteria.26 In the present study, the antibacterial potential of aqueous turmeric gel made from turmeric rhizomes has been concluded to be potent, especially against S. mutans and L. acidophilus. This finding is similar to other studies, even when combined with photodynamic therapy,27 as well as when compared with Aloe vera and Nutmeg28 and with Chlorhexidine.29
The antibacterial effect of methanol Curcumin extracts against S. mutans and Streptococcus pyogenes,30 and aqueous Curcumin extract against S. mutans as well as Staphylococcus aureus, and anaerobic bacteria31 has been reported in the literature.
The similarity in the antibacterial finding is because of constituents of turmeric i.e Curcuminoids mainly Curcumin, bisdemethoxycurcumin, and demethoxycurcumin, which are responsible for the antibacterial nature of turmeric leading to disruption of the cell wall and ultimately death of the specific bacteria.32
However, turmeric leaf extract exhibited a potent antibacterial effect against a wide range of bacteria but not against L. acidophilus which is not concomitant with the present study. This might be due to the use of leaf extract of turmeric which allegedly contains oligosaccharide compounds. These oligosaccharides provide media for the growth of Lactobacillus instead of its inhibition.33
In the present study, turmeric gel showed better clinical outcomes compared to Formocresol as an NVP medicament in primary molar teeth of pediatric patients. However, statistically, the difference was insignificant among the two, i.e., p-value = 0.487 (Table 2). This finding is supported by a study in which turmeric gel showed clinical success as a vital pulpotomy medicament comparable to Formocresol, Propolis, and Calcium Hydroxide.18 Turmeric powder also showed significantly promising clinical results in pulpotomy of primary molars.19 Although the above studies were carried out on vital teeth, the results were concomitant with the present study.
Conclusion
The antibacterial effect and clinical outcomes of turmeric gel are comparable to the conventional medicament, Formocresol, against S. mutans and L. acidophilus, in terms of bacterial count (CFU/ml) in NVP of primary molars of pediatric patients. Therefore, turmeric gel can be used as a safe, cost-effective herbal alternative to Formocresol in the NVP of primary molars.
Limitations of the study
The limitations of the study were the small sample size and short clinical follow-up period that may have an effect on the generalizability of the study results. Furthermore, longer and variable sample transportation time might have an influence on the viability of bacterial colonies which can be standardized by adopting more sensitive techniques for determination of colony counts.
Acknowledgement
The authors would like to give their special appreciation to Dr. Jalees Khalid Khan (Associate Professor of Pathology, Head of Pathology Department, Post Graduate Medical Institute/Ameer-ud-Din Medical College/Lahore General Hospital) for being helpful during the execution of this study. The authors would also like to thank Dr. Tooba, Dr. Fareeha, Mr. Ashfaaq, and Mr. Islam at the Microbiology laboratory pf Lahore General Hospital, Lahore, for facilitating in culture media preparation, plating, and processing of samples.
The authors also convey their regards Mr. Waqas Latif, Biostatistician, University of Health Sciences Lahore, for helping them in the statistical analysis of data.
List of Abbreviations
| AMC | Ameer Uddin Medical College |
| CFU/ml | Colony Forming Units/ml |
| LGH | Lahore General Hospital |
| NaCMC | Sodium Carboxy-Methyl Cellulose |
| NVP | Non-vital pulpotomy |
| PGMI | Postgraduate Medical Institute |
| SPSS | Statistical Package for Social Sciences |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical consideration
Ethical approval was obtained from the Institutional Ethical Review Committee of Postgraduate Medical Institute; Lahore Pakistan vide Letter No: AMC/ PGMI/ LGH/ Synopsis No./ 0081-19 dated 19-04-2019. This is an article derived from the thesis of Masters of Dental Surgery, which has been recently approved for award of degree (Ref # No: UHS/CE-23/T-Exam/6329).
Clinical trial registration
The study was registered as a RCTs in ClinicalTrials.gov: NCT05801354 dated April 6, 2023.
Authors’ contributions
AZ, NB, RD: Drafting of the manuscript, acquisition of data
MM: Principal investigator, concept and design of study
SN: Supervisor, conception of study, critical intellectual input, data analysis and interpretation.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Mashal Mazhar1, Shazia Naz2, Ambreen Zahra3, Nazia Bashir4, Rabia Dastgeer5
- Senior Demonstrator, Department of Operative Dentistry, University College of Dentistry, The University of Lahore, Lahore, Pakistan
- Associate Professor, Department of Operative Dentistry, de’ Montmorency College of Dentistry, Lahore, Pakistan
- Demonstrator, Department of Operative Dentistry, Avicenna Medical and Dental College, Lahore, Pakistan
- Dental Surgeon, Jinnah Burn and Reconstructive Surgery Center, Jinnah Hospital, Lahore, Pakistan
- Senior Demonstrator, Department of Dentistry, Al Aleem Medical College, Lahore, Pakistan
References
- Mohammad SG, Baroudi K. Assessment of the potential of Allium sativum oil as a new medicament for non-vital pulpotomy of primary teeth. J Int Soc Prev Community Dent. 2015;5(4):314. https://doi.org/10.4103/2231-0762.161762
- Hargreaves KM. Cohen’s pathways of the pulp: South Asia edition E-Book. 12th ed. India: Elsevier Health Sciences; 2020 Dec 24.
- Nadelman P, Bedran N, Magno MB, Masterson D, de Castro AC, Maia LC. Premature loss of primary anterior teeth and its consequences to primary dental arch and speech pattern: a systematic review and meta‐analysis. Int J Paediatr Dent. 2020 Nov;30(6):687–712. https://doi.org/10.1111/ipd.12644
- Ritter V, Boushell W, Walter RS. Sturdevant’s art and science of operative dentistry. 7th ed. St. Louis, MO: Elsevier; 2019.
- Ghazal TS, Levy SM, Childers NK, Carter KD, Caplan DJ, Warren JJ, et al. Mutans streptococci and dental caries: a new statistical modeling approach. Caries Res. 2018;52(3):246–52. https://doi.org/10.1159/000486103
- Mitrakul K, Vongsawan K, Watcharakirin W, Khererat P. Quantitative analysis of Lactobacillus and Enterococcus faecalis between irreversible pulpitis and pulp necrosis in primary teeth. Dent Res Oral Health. 2019;2(2):017–31.
- Mohammad SG, Baroudi K. Bacteriological evaluation of Allium sativum oil as a new medicament for pulpotomy of primary teeth. J Int Soc Prev Community Dent. 2015b;5(2):125–30. https://doi.org/10.4103/2231-0762.155738
- Sebourn S, YU Q, Ritwik P. Pulpectomy versus extraction for the treatment of non-vital primary second molars: a retrospective chart review. J Clin Pediatr Dent. 2020;44(5):302–6. https://doi.org/10.17796/1053-4625-44.5.3
- Singh PH, Naorem H. Diagnosis and concepts of vital pulp therapy in primary teeth. EC Clin Med Case Rep. 2020;3(10):19–26.
- Surana P, Khandelwal A, Gopal R, Koppalkar RR, Aafreen S, Gupta S. Recent advances in pulpotomy medicament. Int J Med Oral Res. 2021;6:22–3. https://doi.org/10.4103/ijmo.ijmo_11_20
- Pannu R. Formocresol in dental domain: a review. Int J Sci Res (IJSR). 2018;8(9):ISSN: 2319-7064.
- Lee Y, Choi HG, Park S, Park J. Percutaneous absorption and pharmacokinetics of tetrabromo-o-cresol after topical administration in rats. Drug Metab Pharmacok. 2017;32(1):S94. https://doi.org/10.1016/j.dmpk.2016.10.362
- Salman BN, Vahabi S, Rad MM. Use of herbs and medicinal plants in dentistry: a review. J Dent Sch. 2017;35(2):133–49.
- Park JS, Jasani B, Patel J, Anthonappa RP, King NM. Efficacy of alternative medicaments for pulp treatment in primary teeth in the short term: a meta-analysis. J Evid Based Dent Pract. 2019;19(4):101309. https://doi.org/10.1016/j.jebdp.2019.01.005
- Cruz Martinez C, Diaz Gómez M, Oh MS. Use of traditional herbal medicine as an alternative in dental treatment in Mexican dentistry: a review. Pharm Biol. 2017;55(1):1992–8. https://doi.org/10.1080/13880209.2017.1347188
- Teow SY, Liew K, Ali SA, Khoo ASB, Peh SC. Antibacterial action of curcumin against Staphylococcus aureus: a brief review. J Trop Med. 2016;2016:2853045. https://doi.org/10.1155/2016/2853045
- Elgamily H, Safy R, Makharita R. Influence of medicinal plant extracts on the growth of oral pathogens Streptococcus mutans and Lactobacillus acidophilus: an in-vitro study. Open Access Maced J Med Sci. 2019;7(14):2328–34. https://doi.org/10.3889%2Foamjms.2019.653
- Hugar SM, Kukreja P, Hugar SS, Gokhale N, Assudani H. Comparative evaluation of clinical and radiographic success of formocresol, propolis, turmeric gel, and calcium hydroxide on pulpotomized primary molars: a preliminary study. Int J Clin Pediatr Dent. 2017;10(1):18–23. https://doi.org/10.5005/jp-journals-10005-1400
- Purohit RN, Bhatt M, Purohit K, Acharya J, Kumar R, Garg R. Clinical and radiological evaluation of turmeric powder as a pulpotomy medicament in primary teeth: an in vivo study. Int J Clin Pediatr Dent. 2017;10(1):37–40. https://doi.org/10.5005/jp-journals-10005-1404
- Rahman M, Ahmed S, Rabbi M. Low cost home-made turmeric (hydro) gel: preparation, rheology and prediction of safe period for using. J Dermat Cosmetol. 2019;3(6):145–50.
- Roshan N, Shigli AL, Deshpande SD. Microbiological evaluation of salivary Streptococcus mutans from children of age 5-7 years, pre-and post-atraumatic restorative treatment. Contemp Clin Dent. 2010;1(2):94–7. https://doi.org/10.4103/0976-237X.68602
- Sánchez-Romero MI, Moya JMGL, López JJG, Mira NO. Collection, transport and general processing of clinical specimens in microbiology laboratory. Enferm Infecc Microbiol Clin (Engl Ed). 2019;37(2):127–34. https://doi.org/10.1016/j.eimce.2017.12.005
- Bhujel N, Duggal M, Saini P, Day P. The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment. Eur Arch Paediatr Dent. 2016;17(6):423–34. http://doi.org/10.1007%2Fs40368-016-0247-7
- Mahmood MAK, Ali HE, Abdul-Kadher HK. The role of intracanal medicaments in inhibition of bacteria isolated from root canals of infected primary molars. Mustansiriya Dent J (MDJ). 2018;14(1):92–8.
- Imani Z, Imani Z, Basir L, Shayeste M, Montazeri EA, Rakhshan V. Antibacterial effects of chitosan, formocresol and CMCP as pulpectomy medicament on Enterococcus faecalis, Staphylococcus aureus and Streptococcus mutans. Iran Endod J. 2018;13(3):342–50. https://doi.org/10.22037/iej.v13i3.20791
- Basir L, Kalhori S, Javid AZ, Masjedi MK. Anticaries activity of curcumin on decay process in human tooth enamel samples (in vitro study). J Natl Med Assoc. 2018;110(5):486–90. https://doi.org/10.1016/j.jnma.2017.12.005
- Araújo NC, Fontana CR, Bagnato VS, Gerbi ME. Photodynamic antimicrobial therapy of curcumin in biofilms and carious dentine. Lasers Med Sci. 2014 Mar;29:629–35. https://doi.org/10.1007/s10103-013-1369-3
- Soundarajan S, Malaippan S. Antibacterial activity of Aloe vera, curcumin & nutmeg against Streptococcus mutans & Lactobacillus-a novel trio in-vitro study. Plant Cell Biotechnol Mol Biol:2020;24(8):32-44
- Li B, Li X, Lin H, Zhou Y. Curcumin as a promising antibacterial agent: effects on metabolism and biofilm formation in S. mutans. BioMed Res Int. 2018;2018(3):1-11. https://doi.org/10.1155/2018/4508709
- Mohammed NA, Habil NY. Evaluation of antimicrobial activity of curcumin against two oral bacteria. Autom Control Intell Syst. 2015;3(2):18. https://doi.org/ 10.11648/j.acis.s.2015030201.14
- Al-Sharifi EA, Al-Mahmood AA, Al-Mahmood SU. Estimation the antibacterial effect of curcumin and rosemary among patients with dental caries in vitro. Asian J Pharm Clin Res. 2019;12(3):277–9. https://doi.org/10.22159/ajpcr.2019.v12i3.30378
- Singh N, Gupta S, Rathore V. Comparative antimicrobial study of ethanolic extract of leaf and rhizome of Curcuma longa Linn. Pharmacogn J. 2017;9(2):208-12. https://doi.org/10.5530/pj.2017.2.35
- Ilham LA, Herla R, Dwi S, DewiRestuana S. Antimicrobial activity of turmeric leaf extract against Escherichia coli, Staphylococcus aureus, Shigella dysenteriae, and Lactobacillus acidophilus. IOP Conf Ser: Earth Environ Sci. 2018 Nov 1;205(1):012048. https://doi.org/10.1088/1755-1315/205/1/012048
Keywords: Formocresol, Turmeric (curcuma), pulpotomy, non-vital pulpotomy, Primary (deciduous) teeth, Randomized controlled trial.
Publication History
Received: January 25, 2024
Revised: March 02, 2024
Accepted: March 15, 2024
Published: March 25, 2024
Authors
Mashal Mazhar
Senior Demonstrator, Dept of Operative Dentistry, University College of Dentistry, The University of Lahore, Lahore, Pakistan.
Shazia Naz
Associate Professor, Department of Operative Dentistry, de’ Montmorency College of Dentistry, Lahore, Pakistan.
Ambreen Zahra
Demonstrator, Department of Operative Dentistry, Avicenna Medical and Dental College, Lahore, Pakistan.
Nazia Bashir
Dental Surgeon, Jinnah Burn and Reconstructive Surgery Center, Jinnah Hospital, Lahore, Pakistan.
Rabia Dastgeer
Senior Demonstrator, Department of Dentistry, Al Aleem Medical College, Lahore, Pakistan.
