Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 39(1):33-37
ORIGINAL ARTICLE
Vitamin D levels have a potential role in predicting the disease severity in COVID-19 positive pediatric patients
Maria Hassan1*, Iffat Batool2, Hasan Mujtaba3, Uzma Abid4, Muhammad Mohsin Javaid5
Received: 18 November 2022 Revised date: 13 February 2023 Accepted: 12 March 2023
Correspondence to: Maria Hassan
*Consultant Pediatrician, Primary & Secondary Health Department, THQ Hospital Gujar Khan (Government of Punjab), Rawalpindi, Pakistan.
Email: mariahassan94@yahoo.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
The contagious and invasive nature has made coronavirus disease-19 (COVID-19) a critical health issue for the community. The lower respiratory tract is the major site of inflammation seen in COVID-19-positive individuals. Vitamin D (Vit D) has been proposed to have a positive role in immunomodulation, hence, this study aimed to determine the association between Vit D levels and the severity of COVID-19 in infected pediatric patients presenting at a secondary healthcare hospital in Pakistan.
Methods:
This cross-sectional analytical study was conducted on 100 pediatric patients of the age range 1-18 years from March to December 2021. These patients were hospitalized and diagnosed with coronavirus disease with confirmed results on a real‐time reverse transcription-polymerase chain reaction. Blood samples of the patients were taken to monitor the baseline levels of markers of acute infection and Vit D levels. Patients with serum Vit D levels ≤ 20 ng/ml were labeled with deficiency, those with levels 21-29 ng/ml were presumed to have Vit D insufficiency whereas levels ≥30 ng/ml were considered normal.
Results:
There were 57 (57%) males and 43 (43%) female pediatric patients. The mean age of the patients was 10.46 ± 4.25 years (1-18 years). The deficient Vit D level group had a greater frequency of pyrexia, weakness, cough, anosmia, headache, myalgia, and diarrhea. The levels of Vit D and severity of the disease were significantly associated (p-value = 0.027).
Conclusion:
Pediatric patients with COVID-19 having optimum levels of Vit D were less likely to develop complications associated with the severity of the disease.
Keywords:
COVID-19, pediatric, vitamin D, severity, disease, complications.
Introduction
Coronavirus disease-19 (COVID-19) associated morbidity and fatality has nearly devastated the world population in the preceding year. Coronavirus disease in particular attacks the respiratory tract, however, severe complications including hematological, renal, acute respiratory failure, and/or septic shock have also been well reported in the literature.1 Around 40% of the patients with COVID-19 require admission in the critical care units while the mortality is reported as high as 15%.2 Although due to rapid mutations of the organism still many aspects of the pathogenesis and evolution of the disease process remain debatable; however, the disease severity and complications are few and far reported among the pediatric population.3,4
COVID-19 infection triggers the release of enormous amounts of inflammatory markers especially the cytokines which cause destruction of the lungs’ parenchyma leading to acute respiratory distress syndrome. Recent research has revealed an upsurge of cases and complications in pediatric patients, hence, warranted for the exploration of safe and non-invasive treatment modalities and empirical therapies among this vulnerable group of population.5,6
Vitamin D (Vit D) has a significant role in the development of bones and metabolism at the skeletal level. It also has a significant role in immunomodulation. To enhance innate immunity Vit D is critical for the augmentation of antimicrobial peptides, cathelicidin, and beta-defensin. Cathelicidin and beta-defensin have elucidated pleiotropic ramifications in the induction of immunomodulatory reaction to infectious and pathogenic triggers with a significant impact on f T-lymphocytes by downregulation and upregulation of type 1 and type 2 T cells respectively.7,8 Vit D also plays an indirect stimulatory role in the antigen-presenting capacity of the T-lymphocytes by inducing or inhibiting a cascade of interleukins and cytokines.9,10
On the basis of this immunomodulatory role, the serum Vit D levels are considered a significant biomarker of disease progression and prognostication in COVID-19 patients of both adult and pediatric age groups.11-13 Thus, this study aimed to determine the association between Vit D levels and the severity of COVID-19 in COVID-19-infected pediatric patients presenting at a local secondary health care hospital of Pakistan so as to prescribe this vitamin as a potential empirical treatment in COVID-19 patients.
Methods
This cross-sectional analytical study was performed at the Tehsil Headquarters Hospital Gujar Khan, Rawalpindi, Pakistan from March to December 2021 after approval of the ethical review board. The calculated sample size for the study was 84 with the comparison of two means of Vit D levels with a 95% confidence interval, power of 80%, and margin of error of 5% as per a study conducted by Alpcan et al.13 Sampling was done through non-probability consecutive technique.
A total of 100 patients, of both genders, were recruited in the study with an age range of 1-18 years. The patients were diagnosed with coronavirus disease using polymerase chain reaction as a gold standard test for identification of the virus. Informed assent for the study was taken from the parents. However, patients with non-consenting parents, asymptomatic coronavirus disease, with a history of co-morbidities (e.g., bone metabolism disorders, bleeding disorder, tuberculosis, etc.), and a history of recent Vit D intake as a supplement before the diagnosis of COVID-19, were excluded from the study.
The patient’s demographic profile, medical history, clinical features, and laboratory parameters were recorded. On presentation to the hospital, blood samples were collected to monitor the baseline laboratory investigations including markers of infection [erythrocyte sedimentation rate, C-reactive protein (CRP), D-dimer] and levels of Vit D. Vit D levels in the blood were estimated in Cobas E411 and enzyme-linked immunosorbent assay using the protocol as per available commercial kits. Patients with serum Vit D levels ≤20 ng/ml (Group A) were labeled with deficiency, those with levels 21-29 ng/ml (Group B) were presumed to have Vit D insufficiency, whereas levels ≥30 ng/ml (Group C) were considered as normal.14 Patients were further classified into asymptomatic, mild, moderate, and severe COVID-19 based on the criteria15 as shown in Table 1.
Statistical analysis
Data entry and analysis were done using the data management software IBM SPSS (version 23.0). Frequencies and percentages were used for descriptive variables, while, mean ± SD was given for continuous variables. The chi-square test was used to compare the variables and a p value of ≤0.05 was considered statistically significant.
Table 1. Disease severity criteria.15
| Symptoms | Features |
|---|---|
| Asymptomatic | Positive reverse transcription-polymerase chain reaction test without clinical and radiological features |
| Mild | Infection of the upper respiratory tract without associated findings on respiratory system examination |
| Moderate | Fever, cough, dyspnea, tachypnea, oxygen saturation >90% on room air |
| Severe | Fever, cough, dyspnea, tachypnea, central cyanosis, oxygen saturation >90% on room air, respiratory rate >30 breaths/minute, severe distressful respiration |
| Critical | Acute respiratory distress or respiratory failure or one of the following: septic shock and acute thrombosis |
Results
There were 57 (57%) males and 43 (43%) female pediatric patients. The mean age of the patients was 10.39 ± 4.21 years (1-18 years). Mean Vit D levels in all 100 patients were 16.6515 ± 8.79328 ng/ml. Patients with deficient Vit D levels had a greater frequency of pyrexia, weakness, cough, anosmia, headache, myalgia, and diarrhea, however association was statistically insignificant (p > 0.0.5). Chest X-ray findings and acute respiratory distress were abundantly found in Group A (deficient Vit D levels) as compared to the other groups and were statistically significant (p-value < 0.02). The levels of Vit D and severity of the disease (Table 2) was significantly associated (p-value = 0.027) (Figure 1).
The frequency of symptoms, laboratory parameters, and their association with disease severity is given in Table 2.
Discussion
This study shows a significant association between levels of Vit D and the disease severity in COVID-19 patients. One of the commonest adversity reported with the COVID-19 pandemics in the communities was a hampered natural lifestyle leading to home isolation with subsequent minimal exposure to sunlight causing a decreased Vit D synthesis, especially in the pediatric population.16
Wong et al.17 enrolled (303) infants and toddlers (2-24 months) via random stratification protocol for 6 months to determine the impact of the COVID-19 outbreak on serum Vit D levels in an interrupted time series paradigm. Their analysis concluded a steep decline in Vit D levels with the progression of the pandemic with a rate of -6.32 nmol/l per month, categorically prevalent in the younger age group (2-6 months). The authors thereby proposed a cautious increase in the intake of Vit D by pregnant women during the pandemic.17
Table 2. Association of severity of COVID-19 disease with gender and age groups.
| Asymptomatic | Severity | Total | |||||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | |||||
| Gender | Male | 13 (22.8%) | 29 (50.87%) | 13 (22.8%) | 2 (3.5%) | 57 | 0.061 |
| Female | 11 (25.58%) | 20 (46.51%) | 11 (25.58%) | 1 (2.32%) | 43 | 0.076 | |
| Age groups (years) | 1-5 6-12 13-18 |
9 (37.5%) | 11 (45.83%) | 4 (16.66%) | 0 (%) | 24 (%) | 0.314 |
| 4 (10.81%) | 22 (59.46%) | 9 (24.32%) | 2 (5.40%) | 37 (%) | 0.112 | ||
| 11 (28.20%) | 16 (41.02%) | 11 (28.20%) | 1 (2.56%) | 39 (%) | 0.091 | ||
| Total | 24 | 49 | 24 | 3 | 100 | ||
*Chi square test: No significant association was seen.
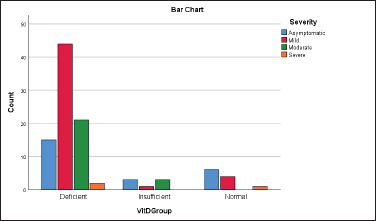
Figure 1. Distribution of Vit D level groups with reference to the severity of the disease (p = 0.027).
Davoudi et al.18 conducted a trial on (153) patients in Iran to ascertain the association between Vit D levels and clinical presentation of coronavirus disease. The reference standard of adequate Vit D was set up at 30 ng/ml. The mean average Vit D levels of the participants were 27.19 ± 20.17 ng/ml with 96 (62.7%) had values below the cutoff.18
Vit D is recognized to play its role as an immunomodulator in inflammatory conditions. Bayramoğlu et al.19 estimated the 25(OH)D levels in (103) pediatric patients with COVID-19 of variable disease severity. They found higher levels of inflammatory markers (CRP, procalcitonin, fibrinogen, and D-dimer) and deficient Vit D levels in 70.6% of patients with moderate-to-severe disease (p < 0.001). Concurrent results were also reported from other studies in adults as well.20,21
Darren et al.22 reported the Vit D status of children with the pediatric inflammatory multisystem syndrome in (18) (0.3-14.6 years) patients in the United Kingdom. Black, Asian, and minority ethnicity were considered to have a greater susceptibility to the syndrome and 72% of the patients with Vit D deficiency had serious complications.
Numerous studies have reported an elaborated prophylactic role of Vit D in the reduction of COVID-19 and respiratory tract infections through major clinical trials. Therefore, a targeted serum evaluation and engagement of Vit D as a prophylactic and treatment modality have been reported in COVID-19 patients.23-25 To date, no standard guidelines for prescribing Vit D to pediatric COVID-19 patients have yet been published from Pakistan. Prophylactic and therapeutic use of Vit D by pediatricians is widely accepted in our country however there is a need for further studies emphasizing the potential utility of these cost-effective nutritional supplements in managing patients with COVID-19.
Conclusion
Pediatric patients with COVID-19 having optimum levels of Vit D are less likely to develop complications related to the severity of the disease.
Limitations of the Study
This study has a small sample size and no intervention is carried out. Further studies with large population size and randomized clinical trials focusing on dose-dependent effects of Vit D in COVID-19 patients are recommended to support the findings of this study.
Acknowledgement
The authors would like to acknowledge the staff of the Pediatric Department of Tehsil Headquarters Hospital Gujar Khan, Rawalpindi, Pakistan, for their logistic support during the study.
List of Abbreviations
| COVID-19 | Coronavirus disease-19 |
| Vit-D | Vitamin D |
| CRP | C-reactive protein |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The study is approved by the Institutional Ethics Committee of the Tehsil Headquarters Hospital Gujar Khan, Rawalpindi, Pakistan vide Letter No. 681/THQ/21, dated 02-02-2021.
Authors’ contributions
MH: Conception and design of study, acquisition of data, and drafting of manuscript with critical intellectual input.
IB: Acquisition and analysis of data and drafting of manuscript.
HM: Critically revised the manuscript with intellectual input.
MJ, UA: Acquisition of data and drafting of manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Maria Hassan1, Iffat Batool2, Hasan Mujtaba3, Uzma Abid4, Muhammad Mohsin Javaid5
- Consultant Pediatrician, Primary & Secondary Health Department, THQ Hospital Gujar Khan (Government of Punjab), Rawalpindi, Pakistan
- Assistant Professor Pediatrics, Foundation University School of Health Sciences, Rawalpindi, Pakistan
- Associate Professor of Pathology, Shaheed Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan
- Senior Registrar, Department of Pediatrics, Holy Family Hospital, Rawalpindi, Pakistan
- Ph.D. Scholar, Health Services Academy, Islamabad, Pakistan
References
- Pimentel GD, Dela Vega MC, Pichard C. Low vitamin D levels and increased neutrophil in patients admitted at ICU with COVID-19. Clin Nutr ESPEN. 2021;44:466–8. https://doi.org/10.1016/j.clnesp.2021.05.021
- Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. 2020;287(17):3693–702. https://doi.org/10.1111/febs.15495
- Adami G, Giollo A, Fassio A, Benini C, Bertoldo E, Bertoldo F, et al. Vitamin D and disease severity in coronavirus disease 19 (COVID-19). Reumatismo. 2021;72(4):189–96. https://doi.org/10.4081/reumatismo.2020.1333
- Demir M, Demir F, Aygun H. Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. J Med Virol. 2021;93(5):2992–9. https://doi.org/10.1002/jmv.26832
- Jain A, Chaurasia R, Sengar NS, Singh M, Mahor S, Narain S. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci Rep. 2020;10(1):20191. https://doi.org/10.1038/s41598-020-77093-z
- Gündüz M, Karaaslan E. COVID-19 reminds us: community vitamin D deficiency. Ann Ital Chir. 2020;91:673–8.
- Karahan S, Katkat F. Impact of serum 25(OH) vitamin D level on mortality in patients with COVID-19 in Turkey. J Nutr Health Aging. 2021;25(2):189–96. https://doi.org/10.1007/s12603-020-1479-0
- Akbari AR, Khan M, Adeboye W, Hai Lee LH, Chowdhury SI. Ethnicity as a risk factor for vitamin D deficiency and undesirable COVID-19 outcomes. Rev Med Virol. 2021;e2291(4):e2291. https://doi.org/10.1002/rmv.2291
- Ghanbari-Afra L, Azizi-Fini I. Commentary to “Vitamin D and survival in COVID-19 patients: a quasi-experimental study” by C. Annweiler et al, JSBMB, 2021. J Steroid Biochem Mol Biol. 2021;214:105960. https://doi.org/10.1016/j.jsbmb.2021.105960
- Kerget B, Kerget F, Kızıltunç A, Koçak AO, Araz Ö, Yılmazel Uçar E, et al Evaluation of the relationship of serum vitamin D levels in COVID-19 patients with clinical course and prognosis. Tuberk Toraks. 2020;68(3):227–35. https://doi.org/10.5578/tt.70027
- Jayawardena R, Jeyakumar DT, Francis TV, Misra A. Impact of the vitamin D deficiency on COVID-19 infection and mortality in Asian countries. Diabetes Metab Syndr. 2021;15(3):757–64. https://doi.org/10.1016/j.dsx.2021.03.006
- Carpagnano GE, Di Lecce V, Quaranta VN, Zito A, Buonamico E, Capozza E, et al. Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19. J Endocrinol Invest. 2021;44(4):765–71. https://doi.org/10.1007/s40618-020-01370-x
- Alpcan A, Tursun S, Kandur Y. Vitamin D levels in children with COVID-19: a report from Turkey. Epidemiol Infect. 2021;149:e180. https://doi.org/10.1017/S0950268821001825
- Hughes BD. Patient education: vitamin D deficiency (beyond the basics). UpToDate; 2023 [cited 2023 Feb]. Available from: https://www.uptodate.com/contents/vitamin-d-deficiency-beyond-the-basics?source=related_link
- Rahemtoola MS, Suhotoo MJ. Commentary on “Vitamin D deficiency and COVID-19: a case-control study at a tertiary care hospital in India.” Ann Med Surg (Lond). 2021;72:102783. https://doi.org/10.1016/j.amsu.2021.102783
- Ilie PC, Stefanescu S, Smith L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin Exp Res. 2020;32(7):1195–8. https://doi.org/10.1007/s40520-020-01570-8
- Wong RS, Tung KT, So HK, Wong WH, Wong SY, Tsang HW, et al. Impact of COVID-19 pandemic on serum vitamin D Level among infants and toddlers: an interrupted time series analysis and before-and-after comparison. Nutrients. 2021;13(4):1270. https://doi.org/10.3390/nu13041270
- Davoudi A, Najafi N, Aarabi M, Tayebi A, Nikaeen R, Izadyar H, et al. Lack of association between vitamin D insufficiency and clinical outcomes of patients with COVID-19 infection. BMC Infect Dis. 2021;21(1):450. https://doi.org/10.1186/s12879-021-06168-7
- Bayramoğlu E, Akkoç G, Ağbaş A, Akgün Ö, Yurdakul K, Selçuk Duru HN, et al. The association between vitamin D levels and the clinical severity and inflammation markers in pediatric COVID-19 patients: single-center experience from a pandemic hospital. Eur J Pediatr. 2021;180(8):2699–705. https://doi.org/10.1007/s00431-021-04030-1
- Israel A, Cicurel A, Feldhamer I, Dror Y, Giveon SM, Gillis D, et al. The link between vitamin D deficiency and COVID-19 in a large population. MedRxiv. 2020:2020–09. https://doi.org/10.1101/2020.09.04.20188268
- Meoli M, Muggli F, Lava SA, Bianchetti MG, Agostoni C, Kocher C, et al. Vitamin D status in adolescents during COVID-19 pandemic: a cross-sectional comparative study. Nutrients. 2021;13(5):1467. https://doi.org/10.3390/nu13051467
- Darren A, Osman M, Masilamani K, Habib Ali S, Kanthimathinathan HK, Chikermane A, et al. Vitamin D status of children with paediatric inflammatory multisystem syndrome temporally associated with severe acute respiratory syndrome coronavirus 2 (PIMS-TS). Br J Nutr. 2022;127:896–903. https://doi.org/10.1136/archdischild-2021-rcpch.657
- Yılmaz K, Şen V. Is vitamin D deficiency a risk factor for COVID-19 in children? Pediatr Pulmonol. 2020;55(12):3595–601. https://doi.org/10.1002/ppul.25106
- Ahmed S, Jafri L. Prognostic utility of baseline 25-hydroxy vitamin D levels in hospitalised COVID-19 patients: hope or hype? J Coll Physicians Surg Pak. 2020;30(10):183–4. https://doi.org/10.29271/jcpsp.2020.supp2.S183
- Cutolo M, Paolino S, Smith V. Evidences for a protective role of vitamin D in COVID-19. RMD Open. 2020;6(3):e001454. https://doi.org/10.1136/rmdopen-2020-001454
Keywords: Acute respiratory distress syndrome, COVID-19, Deficiency, Infection, Vitamin D.
Publication History
Received: November 18, 2022
Revised: February 13, 2023
Accepted: March 12, 2023
Published: March 26, 2023
Authors
Maria Hassan
Consultant PED, Primary & Secondary Health Department, THQ Hospital Gujar Khan (Government of Punjab), Rawalpindi, Pakistan.
Iffat Batool
Assistant Professor Pediatrics, Foundation University School of Health Sciences, Rawalpindi, Pakistan.
Hasan Mujtaba
Associate Professor of Pathology, Shaheed Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan.
Uzma Abid
Senior Registrar, Department of Pediatrics, Holy Family Hospital, Rawalpindi, Pakistan.
Muhammad Mohsin Javaid
Ph.D. Scholar, Health Services Academy, Islamabad, Pakistan.
