Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(1):18-22
ORIGINAL ARTICLE
Root resorption in ameloblastoma: a radiographic analysis of 35 cases
Ruqqia Jehan1, Hasan Mujtaba2*, Nouman Noor3, Muhammad Shoaib4, Asif Noor5, Javeria Afzal6, Mustafa Sajid7, Muhammad Mohsin Javaid8
Received: 11 December 2021 Revised date: 22 February 2022 Accepted: 05 March 2022
Correspondence to: Hasan Mujtaba
*Associate Professor, Department of Oral Pathology, School of Dentistry (SOD), Shahid Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan.
Email: h_mujtaba@outlook.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Odontogenic tumors are heterogenous lesions with diverse clinical manifestations and histopathological features. Ameloblastoma is a slow growing, sizeable benign tumor with an increased recurrence potential. Radiographically, ameloblastoma mimics other odontogenic tumors occurring in the same region but can be differentiated based on certain features. The objective of the study was to evaluate the radiographic features and presence of root resorption in ameloblastoma as a diagnostic feature in the local population.
Methods:
This retrospective hospital-based study was conducted at the Oral and Maxillofacial Surgery Department of Multan Medical and Dental College Multan, Pakistan from 1st Oct 2019 to 31st March 2020. Radiographs of 35 histopathologically confirmed cases of ameloblastoma were included in the study. These radiographs were assessed for site, locularity, and root resorption. Data were processed and analyzed by using SPSS version 23.0
Results:
Mean age of the patients was 35.35+18.2 years with male predominance (66% vs. 34%). A total of 55% cases presented below 35 years age group thus showing increased prevalence in young adults. Multilocular appearance was seen in 24 (68.5%) cases while uni-locular pattern was seen in 12 (31.5%) cases. Root resorption was detected in 19 (54.3%) cases. Statistically, root resorption was not significantly associated with the gender or age of the patients (p > 0.05).
Conclusion:
Multi-locular appearance and root resorption are the key radiographical features of ameloblastoma presenting in our population.
Keywords:
Ameloblastoma, multilocular, root resorption, unilocular, radiograph, odontogenic.
Introduction
Ectomesenchymal cells or odontogenic epithelium is involved in the tooth development.1 Any disturbance or mutation occurring in the tooth development process can lead to odontogenic tumor of diverse types which are classified according to their radiographic and histopathological features.1 Robinson2 described it as a benign tumor that is “usually unicentric, nonfunctional, intermittent in growth, anatomically benign and clinically persistent”. World Health Organization (WHO) considers ameloblastoma as the prototype of odontogenic tumors of epithelial origin with three clinico-pathological subtypes; conventional, unicystic and peripheral ameloblastoma.3 Ameloblastoma is a benign slow growing tumor which has an increased recurrence potential and ability to attain large size.4 Among all odontogenic tumors, it accounts for 13%–58% including its various types.5
Ameloblastoma presents most commonly in the posterior region of mandible with male predominance. The tumor may be found accidently in routine radiograph because of its asymptomatic nature. Swelling and jaw expansion are the most common signs.6 Patients usually present with swelling, mobile tooth, and dull or severe pain7. It is more common in mandible than in maxilla8. Radiographically, this tumor appears either as multilocular or unilocular radiolucency. Multilocular appearance is frequent and may be associated with root resorption.9
Radiographically, blunt or knife-edge root resorptions are pathognomonic for ameloblastomas that differentiate them from other similar lesions in this area including nasopalatine duct cysts, odontogenic keratocysts, and simple bone cysts. Root resorption may be associated with distinct histological features of ameloblastomas, such as benign epithelial tumors without fibrous capsule, epithelial cords and epithelial islands mimicking dental lamina, invasion into the neighboring tissues and release of tooth and bone resorption mediators (epidermal growth factors and interleukins).10
Orthopantomogram (OPG) (Figure 1) and excisional biopsy are mandatory for the diagnosis of the tumor. Computed tomography (CT) scan or cone beam computed tomography are very useful to demarcate the extension of ameloblastoma. CT scan also helps in providing clear anatomic landmarks and define the buccal and lingual curvature of the lesion which are not recorded in two-dimensional radiographs.11
This study was conducted to evaluate the radiographic features and root resorption associated with ameloblastoma. It will contribute to the previous literature as to our knowledge no such study from Pakistan has been reported. Also, the findings will help the surgeons to educate the patients regarding prognosis and follow-up because of increased tendency for recurrence.
Methods
This retrospective, hospital-based study comprised of 35 cases of ameloblastomas. Complete radiographic and clinical data of n = 35 histopathologically diagnosed cases was retrieved from the Oral and Maxillofacial Surgery (OMFS) Department of Multan Medical and Dental College Multan, Pakistan from 1st Oct 2019 to 31st March 2020. Institutional Ethical approval was taken before the acquisition of data.
Inclusion criteria were ameloblastomas, either uni-cystic or multicystic, presenting in adult age group (18-55 years) of both genders. Cases with presence of factors causing root resorption other than the tumor such as periapical lesion due to caries and/or adjacent impacted tooth were excluded. Complete radiographic details were retrieved to determine the features like site, locularity, and root resorption etc. Histopathological features were also recorded.
Statistical analysis
The data were analyzed by using SPSS-version 23.0. Frequency and percentages were calculated for categorical variables like gender, radiological features, and root resorption. Pearson chi-Square test was used to find the association between radiological, clinical and histopathological variables taking 5% level of significance.
Results
Among 35 patients, there were 23 (66%) males and 12 (34%) females. The mean age of the patients was 35.35+18.2 years. Patients were stratified into four age groups with age range from 18 to 55 years. Majority of the patients belonged to 26-35 years age group indicating more prevalence in young adults (Table 1).
Radiologically, most of the cases 25 (86.2%) were seen in posterior region of mandible while only one case was found in the anterior region of maxilla (Table 2).
Regarding locularity, approximately 24 (68.5%) cases presented as multi-locular while uni-locular appearance was observed in only 11 (31.5%) lesions as shown in Figure 2.
Root resorption was seen in 19 (54.3%) cases; 80% of these presented with scalloped margins. Root resorption was seen in 56.3% and 73.7% of unilocular and multilocular lesions respectively. Statistically, no significant association of root resorption with gender and age was observed (Tables 3 and 4).
Discussion:
Ameloblastoma, an odontogenic benign tumor of epithelial origin, shows the tendency of local aggressive behavior with an excessive potential for recurrence.12 There is no gender predominance as ameloblastoma affects both males and females equally. 6,13 The present study observed males predominance over females which is synchronous with the study done by Alves et al.14, while studies conducted in Brazil and Chile reported preponderance in females.15,16 In the current study, 26-35 years age group was most commonly seen which depicts local prevalence in younger population A study conducted by Ranchod17 reported a mean age of
32 ± 11.6 years, whereas a study by Arotiba et al.18, reported patients mostly from an even younger age group, i.e., 18 to 19 years. Another study reported higher age group prevalence between third and fourth decade of age.12 Ameloblastoma rarely occurs in children with almost less than 10% of pediatric cases are seen in children below 10 years of age. The unicystic variant has been found more commonly in the younger age group.19
Table 1. Distribution of ameloblastoma in different age groups.
| Age groups (years) | Frequency (n) | Percentage (%) |
|---|---|---|
| 1825 | 3 | 8.6 |
| 26-35 | 16 | 46 |
| 36-45 | 12 | 34 |
| 46-55 | 04 | 11.4 |
| Total | 35 | 100 |
Table 2. Distribution of ameloblastoma in mandible and maxilla.
| Site | Mandible n (%) | Maxilla n (%) | Total n (%) |
|---|---|---|---|
| Anterior | 4 (13.8%) | 1 (16.7%) | 5 (14.2%) |
| Posterior | 25 (86.2%) | 5 (83.3%) | 30 (85.8%) |
| Total | 29 (83%) | 6 (17%) | 35 (100%) |
The treatment of amelobastoma includes surgical resection with clear margins. Radical surgery is recommended mostly in cases of multicystic / solid and advanced unicystic patterns with long term follow-up.20,21 The present study showed predominant multilocular radiographic appearance than the unilocular pattern; however, no statistical significance with gender or age was observed (p > 0.05). Mostly the literature supports the findings that ameloblastoma is presented with multi-locular radiolucency. 22,23 A study of Kim and Jang24 contradicts these findings as they found a total of 59.2% uni-locular lesions with a fine demarcated boundary. The study, however, included 28.5% population in paediatric and adolescent age group which may be the reason of predominant unilocular pattern.
In this study, root resorption was seen in 19 (54.3%) patients which is much lesser in frequency than the reported study of Bi et al. (87.9%),22 but comparable to those of Au (51.9%)25, and Kitisubkanchana et al. (66.7%)26. Resorption may be regular or uniform, parallel to interface with the islands of neoplastic epithelial cells closer to the roots, and a set of clasts generates this regular surface, which presents as a knife-edge root resorption on the imaging studies.10 Root resorption is more common amongst ameloblastomas than odontogenic keratocysts, simple bone cysts and nasopalatine duct cysts; therefore, this particular feature serves as an important landmark when considering the radiographic signs of ameloblastoma.14 This radiographic finding can be a differentiating feature among other similar lesions of the jaws. 26 Several inflammatory mediators and cytokines are involved in mediating odontoclastic activity in ameloblastomas that play a significant role in the resorption of the root.27
Therefore, the radiolucent lesions of the mandible and maxilla showing root resorption can support the diagnosis of ameloblastoma in differentiation from the other odontogenic cysts and tumors presenting with similar radiographic findings. Recurrence potential in these patients remains high for which a closer follow-up and patient’s education is pivotal.22,25
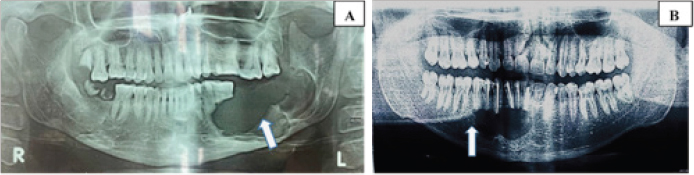
Figure 1. OPG showing (arrows) multilocular (A) radiolucency on the left side of mandible and unilocular radiolucency (B) in the anterior region of mandible.
Table 3. Association between root resorption in ameloblastoma and gender.
| Gender | Root resorption | Total n (%) | p-value* | |
|---|---|---|---|---|
| Absent n (%) | Present n (%) | |||
| Female | 6 (37.5%) | 6 (31.6%) | 12 (34.3%) | 0.604 |
| Male | 10 (62.5%) | 13 (68.4%) | 23 (65.7%) | |
| Total | 16 (45.7%) | 19 (54.3%) | 35 (100%) | |
*Chi square test
Table 4. Association between root resorption in ameloblastoma and age groups.
| Age groups (years) | Root resorption | Total n (%) | p-value* | |
|---|---|---|---|---|
| Absent n (%) | Present n (%) | |||
| 16-25 | 2 (11.76%) | 1 (5.55%) | 3 (8.57%) | 0.292 |
| 26-35 | 6 (35.3%) | 10 (55.55%) | 16 (45.7%) | |
| 36-45 | 7 (41.18%) | 5 (27.8%) | 12 (34.3%) | |
| 46-55 | 2 (11.76%) | 2 (11.11%) | 4 (11.43%) | |
| Total | 17 (48.58%) | 18 (51.42%) | 35 (100%) | |
*Chi square test.
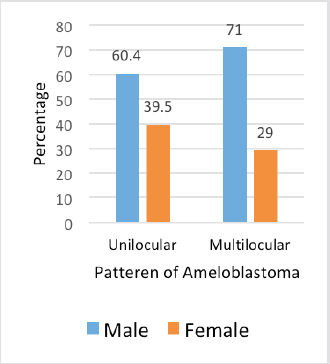
Figure 2. Gender-based distribution of locularity of ameloblastoma (n =35).
Conclusion:
Multilocular appearance and root resorption are the key radiographical features of ameloblastoma presenting in our population. The presence of root resorption may be taken as a differential diagnostic feature for ameloblastoma in contrast to other benign odontogenic tumors of the jaw.
Limitations of the study
One of the limitations of this study was a small sample size and because of the retrospective nature of the study, data of the CT scan of most of the patients could not be retrieved and authors had to rely on the OPG findings of the record files mostly. Prospective studies with large sample size and generating statistical associations between the multicytic pattern, root resorption, and recurrence may be carried out using advanced radiological techniques to validate the findings of the present study.
Acknowledgment
The authors would like to acknowledge the staff of OMFS Department of Multan Medical and Dental College Multan, Pakistan for their logistic and technical support in acquisition of data related to this study. We would also like to acknowledge all those patients whose data has helped us to add this scientific context in the literature.
List of Abbreviations
| OPG | Orthopantomogram |
| WHO | World Health Organization |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
This study was approved by the Ethics Committee of Multan Dental College Multan, Pakistan vide ethical letter MDC#0475 dated 24-02-2020.
Author s’ contribution
RJ, HM, NN: Conception of study, drafting of manuscript, critical revision with important intellectual content.
MS, AN & JA: Drafting of manuscript.
MS, MJ: Acquisition of data.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Ruqqia Jehan1, Hasan Mujtaba2, Noman Noor3, Muhammad Shoaib4, Asif Noor5, Javeria Afzal6, Mustafa Sajid7, Muhammad Mohsin Javaid8
- Senior Registrar, Department of Oral & Maxillofacial Surgery, CMH Multan Institute of Medical Sciences, Multan, Pakistan
- Associate Professor, Department of Oral Pathology, School of Dentistry (SOD), Shahid Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan
- Associate Professor, Department of Operative Dentistry, School of Dentistry (SOD), Shahid Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan
- Assistant Professor, Department of Maxillofacial Surgery, Multan Medical and Dental College Multan, Pakistan
- Associate Professor, Department of Community Dentistry, Multan Medical and Dental College Multan, Pakistan
- Assistant Professor, Department of Community Dentistry, Multan Medical and Dental College Multan, Pakistan
- Associate Professor, Department of Operative Dentistry, Multan Medical and Dental College Multan, Pakistan
- Demonstrator, Community & Preventive Dentistry Department, School of Dentistry (SOD), Shaheed Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan
References
- Soluk-Tekkeşin M, Wright JM. The world health organization classification of odontogenic lesions: a summary of the changes of the 2017 (4th) edition. Turk PatolojiDerg. 2018;34(1):1–5. https://doi.org/10.5146/tjpath.2017.01410
- Robinson L, Martinez MG. Unicystic ameloblastoma: a prognostically distinct entity. Cancer. 1977;40(5):2278–85. https://doi.org/10.1002/1097-0142(197711)40:5<2278
- El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ. WHO classification of head and neck tumours. Lyon, France: IARC; 2017. pp 215–8.
- Wright JM, Soluk Tekkesin M. Odontogenic tumors: where are we in 2017 ? J Istanb Univ Fac Dent. 2017;51(3 Suppl 1):S10–30. https://doi.org/10.17096/jiufd
- Effiom OA, Ogundana OM, Akinshipo AO, Akintoye SO. Ameloblastoma: current etiopathological concepts and management. Oral Dis. 2018;24(3):307–16. https://doi.org/10.1111/odi.12646
- Petrovic ID, Migliacci J, Ganly I, Patel S, Xu B, Ghossein R et al. Ameloblastomas of the mandible and maxilla. Ear Nose Throat J. 2018; 97(7): E26–32. https://doi.org/10.1177/014556131809700704
- Adeline VL, Dimba EA, Wakoli KA, Njiru AK, Awange DO, Onyango JF, et al. Clinicopathologic features of ameloblastoma in Kenya: a 10-year audit. J Craniofac Surg. 2008; 19(6):1589–93. https://doi.org/10.1097/SCS.0b013e31818c0504
- Liu L, Zhang X, Hu Y, Zhang C, Zhang Z. Clinical and pathological analysis of jaw ameloblastomas in 890 patients. Shanghai Kou Qiang Yi Xue. 2015; 24(3):338–40. PMID: 26166525
- Ogunsalu C, Daisley H, Henry K, Bedayse S, White K, Jagdeo B, et al. A new radiological classification for ameloblastoma based on analysis of 19 cases. West Indian Med J. 2006; 55(6):434–9. https://doi.org/10.1590/s0043-31442006000600013
- Martins GG, Oliveira IA, Consolaro A. The mechanism: how dental resorptions occur in ameloblastoma. Dental Press J Orthod. 2019; 24(4):21–32. https://doi.org/10.1590/2177-6709.24.4.021-032.oin
- Hendra FN, Van Cann EM, Helder MN, Ruslin M, de Visscher JG, Forouzanfar T, et al. Global incidence and profile of ameloblastoma: a systematic review and meta-analysis. Oral Dis. 2020;26(1):12–21. https://doi.org/10.1111/odi.13031
- Cadavid AM, Araujo JP, Coutinho-Camillo CM, Bologna S, Junior CA, Lourenço SV. Ameloblastomas: current aspects of the new WHO classification in an analysis of 136 cases. Surg Exp Pathol. 2019; 2(1):1–6. https://doi.org/10.1186/s42047-019-0041-z
- “WHO classification of tumours. In: Barnes L, Eveson J, Reichart P, Sidransky D, editors. Pathology and genetics of head and neck tumous. Lyon, France: IARC Press; 2005. pp 296–300.
- Alves DBM, Tuji FM, Alves FA, Rocha AC, Santos-Silva ARD, Vargas PA, et al. Evaluation of mandibular odontogenic keratocyst and ameloblastoma by panoramic radiograph and computed tomography. Dentomaxillofac Radiol. 2018;47(7):1–7. https://doi.org/10.1259/dmfr.20170288
- Santos JN, Pereira Pinto L, FigueredoCrlvd, Souza Lbd. Odontogenic tumors: analysis of 127 cases. Pesqui Odontol Bras. 2001; 15(4):308–13. https://doi:org/10.1590/S1517-74912001000400007
- Ochsenius G, Ortega A, Godoy L, Peñafiel C, Escobar E. Odontogenic tumors in Chile: a study of 362 cases. J Oral Pathol Med. 2002; 31(7):415–20. https://doi.org/10.1034/j.1600-0714.2002.00073.x
- Ranchod S, Titinchi F, Behardien N, Morkel J. Ameloblastoma of the mandible: analysis of radiographic and histopathological features. J Oral Med Oral Surg. 2021;27(1):6–7. https://doi.org/10.1051/mbcb/2020051
- Arotiba GT, Ladeinde AL, Arotiba JT, Ajike SO, Ugboko VI, Ajayi O. Ameloblastoma in Nigerian children and adolescents: a review of 79 cases. J Oral Maxillofac Surg. 2005; 63(6):747–51. https://doi.org/10.1016/j.joms.2004.04.037
- Castro-Silva II, Israel MS, Lima GS, de Queiroz Chaves Lourenço S. Difficulties in the diagnosis of plexiform ameloblastoma. Oral Maxillofac Surg. 2012;16(1):115–8. https://doi.org/10.1007/s10006-011-0265-x
- Neagu D, Escuder-de la Torre O, Vázquez-Mahía I, Carral-Roura N, Rubín-Roger G, Penedo-Vázquez Á,et al. Surgical management of ameloblastoma: review of literature.J Clin Exp Dent. 2019;11(1):e70. https://doi.org/10.4317/jced.55452
- Effiom OA, Ogundana OM, Akinshipo AO, Akintoye SO. Ameloblastoma: current etiopathological concepts and management. Oral Dis. 2018;24(3):307–16. https://doi.org/10.1111/odi.12646.
- Bi L, Wei D, Hong D, Wang J, Qian K, Wang H et al. A retrospective study of 158 cases on the risk factors for recurrence in ameloblastoma. Int J Med Sci. 2021; 18(14):3326–32. https://doi.org/10.7150/ijms.61500
- Chawla R, Ramalingam K, Sarkar A, Muddiah S. Ninety-one cases of ameloblastoma in an Indian population: A comprehensive review. J Nat Sci Biol Med. 2013; 4(2):310–15. https://doi.org/10.4103/0976-9668.116984
- Kim SG, Jang HS. Ameloblastoma: a clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(6):649–53. https://doi.org/10.1067/moe.2001.114160
- Au SW, Li KY, Choi WS, Su YX. Risk factors for recurrence of ameloblastoma: a long-term follow-up retrospective study. Int J Oral Maxillofac Surg. 2019;48(10):1300–6. https://doi.org/10.1016/j.ijom.2019.04.008
- Kitisubkanchana J, Reduwan NH, Poomsawat S.Pornprasertsuk-Damrongsri S, Wongchuensoontorn C. Odontogenic keratocyst and ameloblastoma: radiographic evaluation.Oral Radiol. 2021; 37(1):55–65. https://doi.org/10.1007/s11282-020-00425-2
- Teo KW, Shi AH, Teh LY, Lee AM. External root resorption in common odontogenic cysts and ameloblastomas of the jaw: A retrospective radiographic study in an Asian population. Oral Surgery. 2021; 14(4):335–41. https://doi.org/10.1111/ors.12628
Keywords: Ameloblastoma, multilocular, unilocular, root resorption, radiograph, odontogenic.
Publication History
Received: December 11, 2021
Revised: February 22, 2022
Accepted: March 05, 2022
Published: March 30, 2022
Authors
Ruqqia Jehan
Department of Oral & Maxillofacial Surgery, CMH Multan Institute of Medical Sciences, Multan, Pakistan.
Hasan Mujtaba
Department of Oral Pathology, School of Dentistry (SOD), Shahid Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan.
Noman Noor
Department of Operative Dentistry, School of Dentistry, Shahid Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan.
Muhammad Shoaib
Department of Maxillofacial Surgery, Multan Medical and Dental College Multan, Pakistan.
Asif Noor
Department of Community Dentistry, Multan Medical and Dental College Multan, Pakistan.
Javeria Afzal
Department of Community Dentistry, Multan Medical and Dental College Multan, Pakistan.
Mustafa Sajid
Department of Operative Dentistry, Multan Medical and Dental College Multan, Pakistan.
Muhammad Mohsin Javaid
School of Dentistry, Shaheed Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan.
