Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(3):118-122
CASE REPORT
Fungal sinusitis in an immunocompetent patient: a case report
Saima Gulzar1*, Shameen Shoaib2, Maham Akhlaq1, Sumera Nighat3, Sameer Anjum4, Nadia Naseem5
Received: 12 July 2022 Revised date: 26 August 2022 Accepted: 08 September 2022
Correspondence to: Saima Gulzar
*Assistant Professor, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan.
Email: saimadilawar@outlook.com
Full list of author information is available at the end of the article.
ABSTRACT
The frequency of fungal rhinosinusitis is increasing over the last two decades worldwide. It is classified into two main types: the invasive disease with a poor prognosis which is predominantly seen in patients with some form of immunosuppression and chronic fungal rhinosinusitis usually affecting the immunocompetent individuals.
We present a case of fungal sinusitis in an immunocompetent 40-year-old male. The patient had a history of recent onset of progressive nasal blockage, discharge, and cough. Computed tomography scan of paranasal sinuses showed bilateral maxillary, left ethmoidal and sphenoidal sinusitis, and left inferior nasal turbinate hypertrophy. The sample received was necrotic slough from the nose that was processed for histopathology, and special stains including Grocott’s Methenamine Silver and Periodic Acid Schiff were applied based on which the diagnosis of non-invasive fungal infection was made. Due to early diagnosis, the patient responded well to sinus clearance and conservative management in the clinical setting.
Keywords:
Fungus, sinusitis, immunocompetent, microscopy, histopathology, special stains.
Introduction
Fungal rhinosinusitis is an inflammation of the mucosal linings of the paranasal sinuses and nasal passages and usually lasts for 12 weeks or slightly longer. 1,2 The reported prevalence of fungal infections in Pakistan is 40.7% in patients with an intact immune system but having anatomic abnormalities like nasal polyposis and other chronic inflammatory states causing mucosal injuries.3
For therapeutic purposes, the two main types of fungal infection are: invasive disease (with parenchymal and vascular invasion) and non-invasive disease.4
Aspergillus and mucormycosis are the commonest of all fungi. The variable clinical presentation in various patients is due to different host-microbial interactions.4 whereas the fungi may act as an antigen in atopic patients causing allergic fungal rhinosinusitis. Fungus ball is a non-invasive form of the disease resulting in the accumulation of fungal hyphae in the sinuses in immunocompetent individuals without invading the sinus mucosa, bone, or blood vessels.5 But, if host immunity deteriorates due to any cause, the fungus ball can progress to an invasive fulminant disease in which the hyphae could erode the sinus wall resulting in facial swelling and pain or obstructing the sinus ostium thus predisposing to secondary bacterial infections. The pathophysiology of fungal sinusitis has not been fully understood yet; but both the genetic background and immune status of the affected hosts have been proposed to be involved in the underlying etiology, along with anatomical disorders causing obstruction, environmental exposure, and the type of fungus.6
Case Presentation
A 40-years-old male presented in the outpatient department of a tertiary care hospital in Lahore with the complaint of non-progressive left nasal blockage associated with foul-smelling yellowish-black nasal discharge for the last 2 months, preceded by an episode of fever. On examination, the patient was alert, of medium build, and not cachexic. There was no obvious swelling in the facial area and there was no cervical lymphadenopathy noted on clinical examination. On acquiring further history, he denied any symptoms related to complications such as meningitis and/or visual disturbances. He was immunocompetent and non-diabetic on laboratory reports. Nasal endoscopic examination showed yellowish-black debris in the bilateral maxillary sinuses. Computed tomography (CT) scan of the paranasal sinuses showed bilateral maxillary, left ethmoidal and sphenoidal sinusitis, and left inferior nasal turbinate hypertrophy (Figure 1). Nasal secretions were sent for histopathological examination. The eosin and hematoxylin-stained sections showed predominantly necrotic tissue containing numerous fungal spores and hyphae. The hyphae were mostly non-septate and had broad diameters. However, as viable tissue was not identified, the parenchymal and vascular invasion was not commented upon (Figure 2A and B). The findings were confirmed by special stains: including Periodic Acid Schiff (PAS) (Figure 2B) and Grocott’s Methenamine Silver Stain (GMS)(Figure 3A and B).
The culture and sensitivity reports were followed 2 weeks later which showed no growth. He underwent sinus clearance to remove the fungus ball. Superadded, antifungal therapy was not indicated. After 3 months of follow-up, he showed tremendous improvement in clinical symptoms and endoscopic examination findings were also unremarkable.
Discussion
Fungi are pathogens in both immunocompetent as well as immunocompromised hosts. The clinical manifestations include acute invasive fungal rhinosinusitis, allergic fungal rhinosinusitis, fungal balls, and chronic rhinosinusitis. With regards to the immunologic status of the patients, allergic fungal sinusitis appears in patients who are atopic while saprophytic and fungal balls occur in apparently healthy patients. The most commonly involved sinus is the maxillary sinus.4,5
The two peaks in the age distribution of fungal sinusitis reported in the literature are the elderly and pediatric population with comorbidities like nasal polyps, immune-mediated disorders, cystic fibrosis, etc.7,8 However, there must always be a high index of suspicion for diagnosing fungi in all age groups. Risk factors include uncontrolled diabetes, any kind of malignancy, post-transplantation patients, those receiving immunosuppressive therapy, and patients with human immunodeficiency virus.9 Non-invasive fungal infections usually present with mild symptoms like nasal discharge and obstruction6 whereas signs and symptoms in invasive fungal infections range from headache, facial swelling with pain, and proptosis to even involvement of vital organs causing blindness, neural impairment, and systemic fungal infection causing even death.4,10 The gold standard test for diagnosis is histopathology along with GMS stain because these techniques not only detect the fungal infection but parenchymal and vascular invasion and host tissue reactions can also be commented upon. In addition, histopathological diagnosis also helps in correlating the false negative results associated with microbial culture and polymerase chain reaction testing.11-13 The radiographic techniques are only supportive, as they may show only mucous membrane thickening, opacification of the sinus cavity, or extent of disease like erosion of the underlying bone.14 The therapeutic approach for symptomatic fungus ball is sinus surgery for clearance after which antifungal medication may not usually be indicated. Although asymptomatic fungus ball patients do not need surgery, the removal of the fungus ball for pathologic diagnosis is not associated with significant morbidity.6 The invasive fungal infection of the sinonasal cavities is a surgical emergency and must be treated urgently and aggressively by surgical debridement and intravenous antifungal therapy, such as Amphotericin B. The surgical options include a combination of endonasal surgical debridement and open surgery. The former approach is indicated for patients who are diagnosed with a minimal extent of the disease. Open surgery should be reserved for patients who have disease extension involving the palate, orbit, or brain parenchyma.4,9,14 In addition, treating the comorbid disease and immunosuppression also helps in treating the infection. The prognosis is poor if the underlying disease and predisposing immunocompromised state are not corrected. The disease and associated complications can occur if infection recurs, so a long-term follow-up is needed until, the crusting phase is achieved, reepithelization occurs, and bony sequestration resolves.15
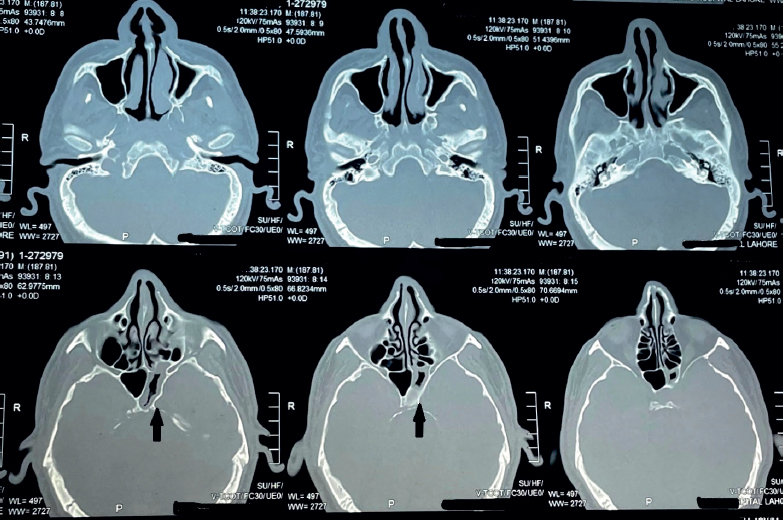
Figure 1. CT Scan image of paranasal sinuses showing wall thickening of the left sphenoid sinus (arrows).
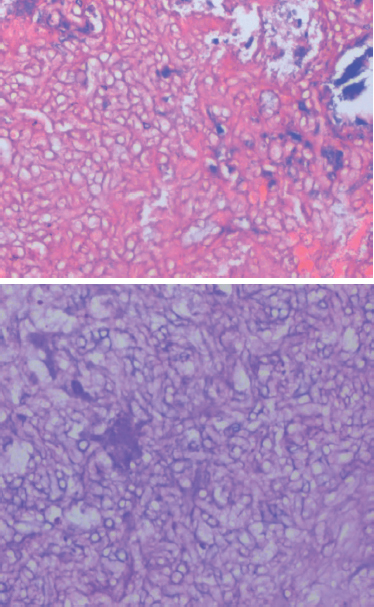
Figure 2. Photomicrographs showing (A) numerous fungal hyphae and spores seen along with eosinophilic mucin with red and blue ripples (H &E stain 400×)(B) numerous non-septate fungal hyphae with broad diameter and spores seen (PAS stain, 400×).
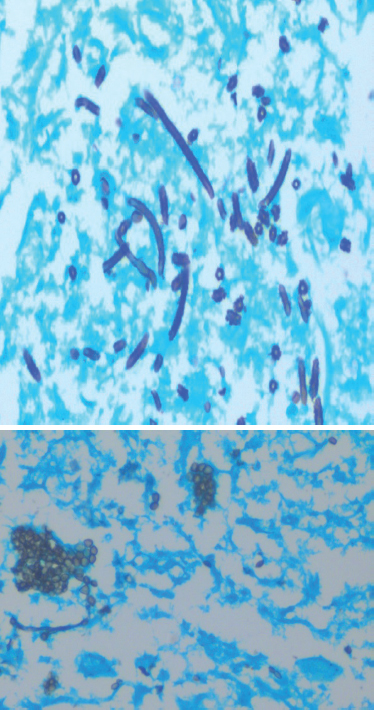
Figure 3. Photomicrographs showing (A) non-septate fungal hyphae seen against necrotic background (B) numerous fungal spores are seen (GMS stain 400×).
Conclusion
We found that fungal ball patients have localized accumulation of hyphae within a single sinus but they are not eradicated without intervention. Hence, there must always be a high index of suspicion for fungi in healthy patients presenting with symptoms of sinusitis to avoid grave complications.
Acknowledgment
The authors would like to acknowledge the residents of the Pathology Department of the University of Health Sciences Lahore, Pakistan for their technical support to the related laboratory work.
List of Abbreviations
| CT | Computed tomography |
| PAS | Periodic acid Schiff |
| GMS | Grocott’s methenamine silver stain |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The case is approved by the Institutional Ethical Review Committee of the University of Health Sciences Lahore, Pakistan.
Authors’ contributions
SG, NN: Conception and drafting of the manuscript, critical intellectual input, and revisions.
SS, MA, SN, SA: Acquisition and interpretation of data.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Saima Gulzar1, Shameen Shoaib2, Maham Akhlaq1, Sumera Nighat3, Sameer Anjum4, Nadia Naseem5
- Assistant Professor, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
- M.Phil student, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
- Assistant Professor, Department of Radiology, Bakhtawar Amin Memorial & Trust Hospital Multan, Pakistan
- Technologist, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
- Professor and Head, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
References
- Salamah MA, Al-Shamani M. Allergic fungal otomastoiditis in a patient without allergic fungal rhinosinusitis: a case report. Am J Med Case Rep. 2019;20:877. https://doi.10.12659/AJCR.915292
- Mossa-Basha M, Ilica AT, Maluf F, Karakoç Ö, İzbudak İ, Aygün N. The many faces of fungal disease of the paranasal sinuses: CT and MRI findings. Diagn Interv Radiol. 2013;19(3):195. https://doi.10.5152/dir.2012.003.
- Sajjad SM, Suhail Z, Ahmed R. Prevalence of fungal infection in nasal polyposis-a cross-sectional study, conducted at a tertiary care hospital in Karachi. J Pak Med Assoc. 2020;2019. https://doi.10.5455/JPMA.300509
- Pham J, Kulla B, Johnson M. Invasive fungal infection caused by Curvularia species in a patient with intranasal drug use: a case report. Med Mycol Case Rep. 2022;37:1–3. https://doi.10.1016/j.mmcr.2022.05.005
- Salman A, Balwant Singh G. Fungal sinusitis in immunocompetent patient: a case report. Available from: https://www.researchgate.net/publication/288226510
- Jiang RS, Huang WC, Liang KL. Characteristics of sinus fungus ball: a unique form of rhinosinusitis. Clin Med Insights Ear Nose Throat. 2018;11:1179550618792254. https://doi.10.1177/1179550618792254
- Knutson JW, Slavin RG. Sinusitis in the aged. Drugs Aging. 1995;7(4):310–6. https://doi.10.2165/00002512-199507040-00006
- Gitomer SA, Poore TS, Anand GS, Cañadas KT. Differing rates of fungi in sinonasal cultures from pediatric sinusitis patients. Int J Pediatr Otorhinolaryngol. 2022;156:111125. https://doi.10.1016/j.ijporl.2022.111125
- Razem B, Dennai Y, Slimani F. Chronical rhino-orbital mucormycosis in an immunocompetent host: a case report. Int J Surg Case Rep. 2021;82:105882. https://doi.10.1016/j.ijscr.2021.105882.
- Althomaly DH, AlMomen AA. Pediatric alternating allergic fungal rhinosinusitis: a case report and literature review. Int J Surg Case Rep. 2019;54:60–2. https://doi.10.1016/j.ijscr.2018.11.015
- Jensen HE. Histopathology in the diagnosis of invasive fungal diseases. Curr Fungal Infect Rep. 2021;15(1):23–31. https://doi.10.1007/s12281-021-00412-y
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24(2):247–80. https://doi.10.1128/CMR.00053-10.
- Kung VL, Chernock RD, Burnham CA. Diagnostic accuracy of fungal identification in histopathology and cytopathology specimens. Eur J Clin Microbiol Infect Dis. 2018;37(1):157–65. https://doi.10.1007/s10096-017-3116-3
- Mohpatra M, Mahapatra A, Srivastava A. Maxillary fungal osteomyelitis: a review of literature and report of a rare case. Ann Maxillofac Surg. 2019;9(1):168. https://doi.10.4103/ams.ams_218_18.
- Ditha BA, Sutikno B. Extraction of sphenochoanal polyp with functional endoscopic sinus surgery approach: a rare case and review article. Int J Surg Case Rep. 2022;97:107429.
Keywords: Fungus, Sinusitis, Immunocompetent, Microscopy, Diagnosis
Publication History
Received: July 12, 2022
Revised: August 26, 2022
Accepted: September 08, 2022
Published: September 25, 2022
Authors
Saima Gulzar
Assistant Professor, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
Shameen Shoaib
M.Phil student, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
Maham Akhlaq
Assistant Professor, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
Sumera Nighat
Assistant Professor, Department of Radiology, Bakhtawar Amin Memorial & Trust Hospital Multan, Pakistan
Sameer Anjum
Technologist, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
Nadia Naseem
Professor and Head, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Pakistan
