Original Article
Volume: 40 | Issue: 1 | Published: Mar 25, 2024 | Pages: 55 - 60 | DOI: 10.24911/BioMedica/5-1138
Comparison of Functional Outcome Between Locking Plate Technique Versus Hybrid Ilizarov Technique in Patients with Complex Tibial Plateau Fractures
Authors: Baqir Jafree , Adeel Hamid , Shuja Uddin , Sher Afghan , Shoaib Saleem , Muhammad Khalid Syed
Article Info
Authors
Baqir Jafree
Assistant Professor, Department of Orthopedic Surgery, Jinnah Hospital, Lahore, Pakistan.
Adeel Hamid
Assistant Professor, Department of Orthopedic Surgery, Lahore General Hospital, Lahore, Pakistan.
Shuja Uddin
Consultant Orthopedic Surgeon, Lahore General Hospital, Lahore, Pakistan.
Sher Afghan
Assistant Professor, Department of Orthopedic Surgery, Services Institute of Medical Sciences, Lahore, Pakistan.
Shoaib Saleem
Consultant Orthopedic Surgeon, Continental Medical College, Lahore, Pakistan.
Muhammad Khalid Syed
Professor of Orthopedic Surgery, Lahore General Hospital, Lahore, Pakistan.
Publication History
Received: January 20, 2024
Accepted: March 15, 2024
Published: March 25, 2024
Abstract
Background and Objective: Schatzker type V or VI tibial plateau fractures pose complicated surgical problems, with potential complications including neurovascular injury, compartment syndrome, and soft-tissue and ligament damage. Successful treatment requires regenerating articular cartilage, maintaining biological integrity, realigning the mechanical axis, stabilizing the joint, and preserving mobility. This study compares the functional outcomes of two approaches, the locking plate technique and the hybrid Ilizarov technique, in managing complicated tibial plateau fractures.
Methods: This cross-sectional study was conducted on 78 patients presenting with proximal tibial complex fracture at the Orthopedic Surgery Department of Jinnah Hospital, Lahore. Patients were divided into two groups, Group A received the Hybrid Ilizarov Technique while Group B received the locking plate technique as a treatment modality for their fracture. Data were analyzed using statistical software with a p-value <0.05 as significant.
Results: In Group A (Hybrid Ilizarov Technique), 84.6% of males and 15.4% of females participated, while Group B (locking plate technique) had 82.1% of males and 17.9% of females. Type VI fractures were the most common in both groups. Postoperative Rasmussen’s clinical functional knee score was higher in Group B (24.90 ± 4.266) as compared to Group A (22.23 ± 5.783). Functional outcome was reported as excellent in 46.2% of patients of Group A as compared to 30.8% of patients of Group B suggesting the supremacy of the locking plate technique in treating complex tibial plateau fractures.
Conclusion: The locking plate technique is a more reliable method for treating complex proximal tibial fractures than the hybrid Illizarov technique.
Keywords: Tibia, fracture, external fixation,
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 40(1):55-60
ORIGINAL ARTICLE
Comparison of functional outcome between locking plate technique versus hybrid Ilizarov technique in patients with complex tibial plateau fractures
Baqir Jafree1, Adeel Hamid2, Shuja Uddin3*, Sher Afghan4, Shoaib Saleem5, Muhammad Khalid Syed6
Received: 20 January 2024 Revised date: 18 February 2024 Accepted: 15 March 2024
Correspondence to: Shuja Uddin
*Consultant Orthopedic Surgeon, Lahore General Hospital, Lahore, Pakistan.
Email: Drshujauddin111@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Schatzker type V or VI tibial plateau fractures pose complicated surgical problems, with potential complications including neurovascular injury, compartment syndrome, and soft-tissue and ligament damage. Successful treatment requires regenerating articular cartilage, maintaining biological integrity, realigning the mechanical axis, stabilizing the joint, and preserving mobility. This study compares the functional outcomes of two approaches, the locking plate technique and the hybrid Ilizarov technique, in managing complicated tibial plateau fractures.
Methods:
This cross-sectional study was conducted on 78 patients presenting with proximal tibial complex fracture at the Orthopedic Surgery Department of Jinnah Hospital, Lahore. Patients were divided into two groups, Group A received the Hybrid Ilizarov Technique while Group B received the locking plate technique as a treatment modality for their fracture. Data were analyzed using statistical software with a p-value <0.05 as significant.
Results:
In Group A (Hybrid Ilizarov Technique), 84.6% of males and 15.4% of females participated, while Group B (locking plate technique) had 82.1% of males and 17.9% of females. Type VI fractures were the most common in both groups. Postoperative Rasmussen’s clinical-functional knee score was higher in Group B (24.90 ± 4.266) as compared to Group A (22.23 ± 5.783). Functional outcome was reported as excellent in 46.2% of patients of Group A as compared to 30.8% of patients of Group B suggesting the supremacy of the locking plate technique in treating complex tibial plateau fractures.
Conclusion:
The locking plate technique is a more reliable method for treating complex proximal tibial fractures than the hybrid Illizarov technique.
Keywords:
Tibial plateau fracture, Schatzker type V and VI, hybrid Ilizarov, locking plate, Rasmussen’s knee clinical-functional score.
Introduction
Schatzker type V or VI for tibial plateau fractures presents complex surgical challenges, marked by potential complications such as neurovascular injury, compartment syndrome, and soft-tissue and ligament damage.1,2 Critical variables impacting long-term prognosis include the absence of articular congruity restoration and ligamentous instability.3 Success in treatment necessitates restoring articular cartilage, maintaining biological integrity, realigning the mechanical axis, stabilizing the joint, and preserving mobility.4
While standard open reduction and internal fixation (ORIF) with a lateral locking plate can successfully restore osseous alignment, it is associated with high surgical morbidity, particularly severe infection and wound necrosis. The Ilizarov technique offers a viable alternative, allowing closed reduction and fixation without extensive soft tissue complications.5,6
In cases of high-energy fractures with intra-articular comminution (AO/OTA class C3) and substantial soft-tissue compromise, the Ilizarov circular ring fixator may offer benefits. Stability is achieved even in situations where internal fixation mechanisms provide only a tenuous hold. Ilizarov spanning of the knee achieves indirect reduction through ligamentotaxis, and percutaneous fixation can restore the articular surface when proper leg alignment has been established.7
Tibial fractures can result from high or low-energy trauma, with complex and open fractures more common in high-energy incidents.8 Open fractures carry a higher risk of complications and long-term disability.9
Tibial plateau fractures present treatment challenges, and management options include both non-operative and surgical approaches. Non-operative therapy, such as the Sarmiento program, is suitable for stable, non-displaced fractures, sub-meniscal fractures, and certain patient populations like the elderly.10,11 Surgical therapy becomes necessary for displaced fractures, fractures with vascular or compartment syndrome involvement, and certain fracture types. Surgical methods encompass internal fixation techniques such as biologic fixation, arthroscopic fixation, and standard double-plating, as well as external fixation methods using devices like the Ilizarov instrument or hybrid fixators. Balloon tibioplasty, while promising, lacks established long-term efficacy.12 Studies evaluating Rasmussen’s knee functional outcome demonstrate varying results with the hybrid Ilizarov technique and locking plate approach.13,14
This research aims to contribute to the existing knowledge by comparing the functional outcomes of patients undergoing the locking plate approach versus the hybrid Ilizarov technique for complicated tibial plateau fractures. Given the scarcity of local studies on this issue, the findings of this research are anticipated to enhance the understanding and treatment of such fractures in the future.
Methods
After receiving approval from the hospital’s ethical committee, 78 patients from the Department of Orthopedics meeting the inclusion criteria were enrolled, i.e., patients presenting with proximal tibial complex fracture (Schatzker type V and VI), both genders and ages between 20 and 65 years. Written informed consent and complete medical histories were obtained. Patients were divided using the lottery approach into two treatment groups; Group A received the Hybrid Ilizarov Technique, and Group B received the Locking Plate Technique. After pre-operative measures and assessment for fitness, the patient, in a supine position on a traction table, underwent knee flexion to 90 degrees after spinal anesthesia. A tourniquet was used for blood flow restriction during the locking compression plate fixation. C-arm imaging verified fracture healing. Lateral or medial plating was employed via the respective incision. A hybrid Ilizarov circular ring fixator was applied, with traction through k-wires and Schanze screws connected to a C-ring. Patients were discharged on the second post-operative day.
Active ROM was started at the end of the first week. Patients practiced non-weight bearing (crutch-walking) for 2 months. Regular check-ups radiological evaluations and functional outcomes were determined by Rasmussen clinical-functional assessment score. Scores were graded as Excellent (27-30), Good (20-26), Fair (10-19), and Poor (<10).13 Any incidence of infection was reported and compared. Time for union in both groups was compared, and non-union incidence was reported.
Statistical analysis
Data were entered and processed using Statistical Package for Social Sciences version 25.0. Descriptive statistics were used for age and Rasmussen’s knee functional score. Gender, fracture type, and functional result were defined in frequencies and percentages. The functional outcome at 6 months was compared between the two groups using the chi-square test. Significance was set at p-value <0.05.
Results
Gender distribution showed 33 males and 6 females in Group A, while 32 males and 7 females in Group B (Figure 1). The mean age was 37.08 ± 8.090 years in Group A while 36.77 ± 7.869 years in Group B. The mean body mass index (BMI) was 27.2 ± 3.5 kg/m2 in Group A and 28.4 ± 3.9 kg/m2 in Group B. Fracture type distribution was type-V: 48.7% and VI: 51.3% in Group A, while type-V: 46.2% and VI: 53.8% in Group-B. Rasmussen’s knee clinical-functional score was 22.23 ± 5.783 in Group A and 24.90 ± 4.266 in Group B. Functional outcomes were Excellent (30.8% vs. 46.2%) and Good (38.5% vs. 41.0%) in Group-A and B, respectively. The infection rate was 15.4% and 12.8% in Groups and B, respectively. 0 No significant association was seen between gender, age, BMI, and type of fracture (p > 0.05) (Tables 1-3).
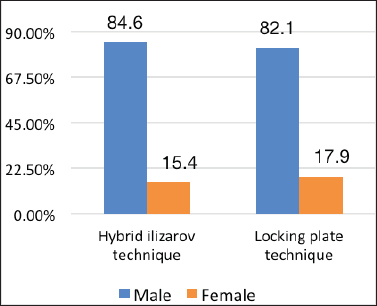
Figure 1. Comparison of gender distribution between groups.
Discussion
Fracture reduction refers to the process through which the initial displacement of a fracture is reversed. Reconstitution of the original anatomical position of fracture pieces is one definition of fracture reduction. In intra-articular fractures, the damaged cancellous bone and articular fragments must be removed. 12
The gold standard for treating fractures of the tibial plateau is surgical intervention. It is difficult to make an accurate comparison between the clinical outcomes of different reduction techniques because of the differences in injury, co-morbid conditions of the patient, and outcome measures.15-17
Expanding on this accomplishment, a number of investigations have shown that a laterally placed locked plate in the proximal tibia has mechanical stability and overall stiffness comparable to the conventional control offered by dual plating.18,19
The Ilizarov procedure has several benefits, such as the ability to reduce and fixate fracture fragments with little soft tissue exposure and blood loss if performed according to the original instructions. Early weight bearing is possible because of fixation’s stability.20,21
One typical consequence is a pin tract infection, which may be treated with adequate dressing changes on a regular basis. Less research has been done to compare Ilizarov and related treatments. A randomized multicenter study conducted in Canada over 82 patients, comparing plate fixation with circular external fixation comparable to Ilizarov found that, although both techniques resulted in sufficient Western Ontario and McMaster Universities Arthritis Index scores at 2 years after the injury were not significantly different between the groups with regard to the pain (p = 0.923), stiffness (p = 0.604), or function (p = 0.827) categories.21 In yet another piece of research, Dendrinos et al.22 came to the conclusion by conducting their study on 24 patients that the Ilizarov technique is an effective method for the management of complex fractures of the proximal tibia as fractures united, with an average time to healing of 14.4 weeks without any septic arthritis and postoperative skin infections. This was the case when extensive dissection and internal fixation were ruled out as treatment options because of comminuted fractures and compromised soft tissue.22
Table 1. Functional outcome stratification within groups with respect to type of fracture.
| Type of fracture | Functional outcome* | Groups | Total | p-value** | |
|---|---|---|---|---|---|
| Hybrid ilizarov technique | Locking plate technique | ||||
| Type-V | Excellent | 7 | 9 | 16 | 0.677 |
| 36.8% | 50.0% | 43.2% | |||
| Good | 10 | 8 | 18 | ||
| 52.6% | 44.4% | 48.6% | |||
| Fair | 2 | 1 | 3 | ||
| 10.5% | 5.6% | 8.1% | |||
| Total | 19 | 18 | 37 | ||
| 100.0% | 100.0% | 100.0% | |||
| Type-VI | Excellent | 5 | 9 | 14 | 0.220 |
| 25.0% | 42.9% | 34.1% | |||
| Good | 5 | 8 | 13 | ||
| 25.0% | 38.1% | 31.7% | |||
| Fair | 8 | 3 | 11 | ||
| 40.0% | 14.3% | 26.8% | |||
| Poor | 2 | 1 | 3 | ||
| 10.0% | 4.8% | 7.3% | |||
| Total | 20 | 21 | 41 | ||
| 100.0% | 100.0% | 100.0% | |||
*Rasmussen clinical-functional outcome.
**Chi-square test.
Table 2. Functional outcome stratification within groups with respect to gender.
| Gender | Functional outcome* | Groups | Total | p-value** | |
|---|---|---|---|---|---|
| Hybrid ilizarov technique | Locking plate technique | ||||
| Male | Excellent | 10 | 13 | 23 | 0.504 |
| 30.3% | 40.6% | 35.4% | |||
| Good | 14 | 15 | 29 | ||
| 42.4% | 46.9% | 44.6% | |||
| Fair | 7 | 3 | 10 | ||
| 21.2% | 9.4% | 15.4% | |||
| Poor | 2 | 1 | 3 | ||
| 6.1% | 3.1% | 4.6% | |||
| Total | 33 | 32 | 65 | ||
| 100.0% | 100.0% | 100.0% | |||
| Female | Excellent | 2 | 5 | 7 | 0.329 |
| 33.3% | 71.4% | 53.8% | |||
| Good | 1 | 1 | 2 | ||
| 16.7% | 14.3% | 15.4% | |||
| Fair | 3 | 1 | 4 | ||
| 50.0% | 14.3% | 30.8% | |||
| Total | 6 | 7 | 13 | ||
| 100.0% | 100.0% | 100.0% | |||
*Rasmussen clinical-functional outcome.
**Chi-square test.
Table 3. Functional outcome stratification within groups with respect to age.
| Age groups | Functional outcome* | Groups | Total | p-value** | |
|---|---|---|---|---|---|
| Hybrid ilizarov technique | Locking plate technique | ||||
| 25-40 years | Excellent | 7 | 10 | 17 | 0.459 |
| 33.3% | 43.5% | 38.6% | |||
| Good | 7 | 10 | 17 | ||
| 33.3% | 43.5% | 38.6% | |||
| Fair | 5 | 2 | 7 | ||
| 23.8% | 8.7% | 15.9% | |||
| Poor | 2 | 1 | 3 | ||
| 9.5% | 4.3% | 6.8% | |||
| Total | 21 | 23 | 44 | ||
| 100.0% | 100.0% | 100.0% | |||
| 41-50 years | Excellent | 5 | 8 | 13 | 0.341 |
| 27.8% | 50.0% | 38.2% | |||
| Good | 8 | 6 | 14 | ||
| 44.4% | 37.5% | 41.2% | |||
| Fair | 5 | 2 | 7 | ||
| 27.8% | 12.5% | 20.6% | |||
| Total | 18 | 16 | 34 | ||
| 100.0% | 100.0% | 100.0% | |||
*Rasmussen clinical-functional outcome.
**Chi-square test.
Bone loss is a common complication of complex fractures. Maurizio et al.23 discovered that the Ilizarov approach was efficient in managing these fractures because it made it possible to address deformity, infection, non-union, and bone loss all at the same time. Foster et al.24 conducted a study involving 40 individuals (21 closed fractures and 19 open fractures). Injuries were treated in a range of 0-35 days (average = 8 days), and the average duration to union was 187 days (87-370 days). Non-union was present in four cases.24 Union time for the 24 patients evaluated by Dendrinos et al.22 (11 open, 13 closed fractures) was an average of 14.4 weeks.
In spite of this, Bacon et al.25 conducted a study on the treatment of tibial plafond fractures and came to the conclusion that “definitive external fixation and staged ORIF” have comparable rates of union, time to union, and complication rates. To assess the findings’ validity and long-term functional effects, they recommended carrying out bigger randomized prospective trials.25
In this study, the Mean Rasmussen’s knee clinical-functional score in Group A patients was 22.23 ± 5.783 and 24.90 ± 4.266 in Group B patients. According to functional outcome, in the Hybrid Ilizarov technique group, 12(30.8%) had excellent outcomes, while 15(38.5%), 10 (25.6%), and 2 (5.1%) had good, fair, and poor outcomes, respectively, while in locking plate technique group, 18 (46.2%) had excellent outcome, while 16 (41.0%), 4 (10.3%), and 1 (2.6%) had good, fair, and poor outcomes, respectively.
According to research conducted by Raza et al.7 25% of participants in the hybrid Ilizarov procedure were judged as excellent, 60% as good, 10% as fair, and 5% as poor in terms of their knee’s functional outcome. In another study done by Vélez et al.18 the hybrid Ilizarov procedure was used to score the knee functional outcome. Of these, 40% were labeled as excellent, 40% good, 15% fair, and 5% poor.
Rasmussen’s knee functional outcome was used in the study, and the locking plate technique was scored as outstanding by 50% of participants, good by 35%, fair by 15%, and poor by 0%. In a study by Karunakaran et al.26 the locking plate technique was judged as outstanding by 35% of participants, good by 42%, fair by 15%, and poor by 8% based on Rasmussen’s knee functional result. This comprehensive overview highlights the intricate considerations in tibial plateau fracture management, emphasizing tailored approaches based on fracture characteristics, patient factors, and soft tissue conditions. There is a lack of data for such a comparison-based study in our local population hence the findings of this study may open avenues for further research in our clinical settings.
Conclusion
The locking plate technique is a more dependable and outcome-based approach for treating complex proximal tibial fractures than the hybrid Illizarov technique.
Limitations of the study
The study has a small sample size and the radiological assessment through standard scoring systems could not be made a part of this study as only clinical-functional outcomes were evaluated.
Acknowledgement
The authors would like to acknowledge the staff of the Department of Orthopedic Surgery, Jinnah Hospital Lahore, Pakistan, for their technical support during surgical treatment and follow-up of the patients.
List of Abbreviations
| ORIF | Open reduction and internal fixation |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The study was approved by the institutional Ethical Committee of Allama Iqbal Medical college, Lahore, Pakistan, vide Letter no. 73-ERB/2022 dated 3rd July 2022.
Authors’ contributions
BJ, AH, SU: Conception and design of study, acquisition, and analysis of data.
SA, SS, MKS: Drafting of the manuscript, revision of manuscript with critical intellectual input.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Baqir Jafree1, Adeel Hamid2, Shuja Uddin3, Sher Afghan4, Shoaib Saleem5, Muhammad Khalid Syed6
- Assistant Professor, Department of Orthopedic Surgery, Jinnah Hospital, Lahore, Pakistan
- Assistant Professor, Department of Orthopedic Surgery, Lahore General Hospital, Lahore, Pakistan
- Consultant Orthopedic Surgeon, Lahore General Hospital, Lahore, Pakistan
- Assistant Professor, Department of Orthopedic Surgery, Services Institute of Medical Sciences, Lahore, Pakistan
- Consultant Orthopedic Surgeon, Continental Medical College, Lahore, Pakistan
- Professor of Orthopedic Surgery, Lahore General Hospital, Lahore, Pakistan
References
- Aziz MA, Fawzy S. Treatment of complex tibial plateau fractures using Ilizarov external fixator with or without minimal internal fixation. Egypt Orthop J. 2016;51(1):60–4. https://doi.org/10.4103/1110-48.194436
- Tomić S, Baljozović A, Jeremić D. High-energy tibial plateau fractures treated with Ilizarov fixator. Srp Arh Celok Lek. 2019;147:427–31. https://doi.org/10.2298/SARH180413038T
- Manjunatha H, Mahesh U. Surgical management of tibial condylar fractures. Intern J Orthop Sci. 2019;5(1):83–6. https://doi.org/10.22271/ortho.2019.v5.i1b.19
- Ahmed ASA. Management of open complex tibial plateau fractures by Ilizarov fixator: average follow-up of 8.5 years. Egypt Orthop J. 2019;54:72–8. http://doi.org/10.4103/eoj.eoj_5_19
- Boutefnouchet T, Lakdawala AS, Makrides P. Outcomes following the treatment of bicondylar tibial plateau fractures with fine wire circular frame external fixation compared to open reduction and internal fixation: a systematic review. J Orthop. 2016;13:193–9. https://doi.org/10.1016%2Fj.jor.2015.02.002
- Yao Y, Lv H, Zan J, Li J, Zhu N, Jing J. Functional outcomes of bicondylar tibial plateau fractures treated with dual buttress plates and risk factors: a case series. Injury. 2014;45(12):1980–4. https://doi.org/10.1016/j.injury.2014.10.004
- Raza A, Kumar S, Kumar D, Qadir A, Muzzammil M, Lakho MT. Complex tibial plateau fractures: primary fixation using the Ilizarov external fixator. A two-year study at Civil Hospital Karachi, Pakistan. Cureus. 2019;11(8):5375–82. https://doi.org/10.7759/cureus.5375
- Albuquerque PR, Hara R, Prado J, Schiavo L, Giordano V, Amaral NPD. Epidemiological study on tibial plateau fractures at a level I trauma center. Acta Ortop Bras. 2013;21(2):109–15. https://doi.org/10.1590/S1413-78522013000200008
- Kohlprath R, Assal M, Uçkay I, Holzer N, Hoffmeyer P, Suva D. Open fractures of the tibia in the adult: surgical treatment and complications. Rev Med Suisse. 2011;7(322):2484–8.
- Born CT, Gil JA, Johnson JP. Periprosthetic tibial fractures. J Am Acad Orthop Surg. 2018;26(8):167–72. https://doi.org/10.5435/jaaos-d-16-00387
- Laible C, Earl-Royal E, Davidovitch R, Walsh M, Egol KA. Infection after spanning external fixation for high-energy tibial plateau fractures: is pin site-plate overlap a problem? J Orthop Trauma. 2012;26(2):92–7. https://doi.org/10.1097/bot.0b013e31821cfb7a
- Craiovan BS, Keshmiri A, Springorum R, Grifka J, Renkawitz T. Minimally invasive treatment of depression fractures of the tibial plateau using balloon repositioning and tibioplasty: video article. Orthopade. 2014;43:930–3. https://doi.org/10.1007/s00132-014-3019-2
- Bormann M, Bitschi D, Neidlein C, Berthold DP, Jörgens M, Pätzold R, et al. Mismatch between clinical-functional and radiological outcome in tibial plateau fractures: a retrospective study. J Clin Med. 2023;12(17):5583–94. https://doi.org/10.3390/jcm12175583
- Yang Y, Zhou X, Ji H, Zhou X, Ye L, Zhang M. A novel arthroscopically assisted reduction technique for three patterns of posterolateral tibial plateau fractures. J Orthop Surg Res. 2020;15:376–83. https://doi.org/10.1186/s13018-020-01901-5
- Júnior MK, Fogagnolo F, Bitar RC, Freitas RL, Salim R, Paccola CAJ. Tibial plateau fractures. Rev Bras Ortop. 2015;44(6):468–74. https://doi.org/10.1016/s2255-4971(15)30142-7
- Gálvez-Sirvent E, Ibarzábal-Gil A, Rodríguez-Merchán EC. Complications of the surgical treatment of fractures of the tibial plateau: prevalence, causes, and management. EFORT Open Rev. 2022;7(8):554–68. https://doi.org/10.1530/eor-22-0004
- Prabhakar S, Mohan G, Kathir Azhagan S, Karthikeyan M. A prospective study of hybrid external fixation for proximal tibial fractures. Int J Orthop Sci. 2018;4(3):91–4. https://doi.org/10.22271/ortho.2018.v4.i3b.19
- Vélez DA, Headford M, Suresh KV, Liberatos PM, Bledsoe G, Revak T. Biomechanical analysis of dual versus lateral locked plating in elderly bicondylar tibial plateau fractures: Does medial comminution matter? Injury. 2022;53(10):3109–14. https://doi.org/10.1016/j.injury.2022.08.039
- Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop Relat Res. 2003;412:189–95. https://doi.org/10.1097/01.blo.0000071754.41516.e9
- Spiegelberg B, Parratt T, Dheerendra S, Khan W, Jennings R, Marsh D. Ilizarov principles of deformity correction. Ann R Coll Surg Engl. 2010;92(2):101–5. https://doi.org/10.1308/003588410X12518836439326
- Hall JA, Beuerlein MJ, Mckee MD. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Surgical technique. J Bone Joint Surg Am. 2009;91:74–88. https://doi.org/10.2106/jbjs.g.01165
- Dendrinos GK, Kontos S, Katsenis D, Dalas A. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996;78(5):710–7.
- Maurizio A, Giulia O, Massimiliano M. Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation. J Trauma. 2007;63(5):1043–53. https://doi.org/10.1097/ta.0b013e3181238d88
- Foster P, Barton S, Jones S, Morrison R, Britten S. The treatment of complex tibial shaft fractures by the Ilizarov method. J Bone Joint Surg Br. 2012;94(12):1678–83. https://doi.org/10.1302/0301-620x.94b12.29266
- Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, et al. A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: open reduction and internal fixation versus external Ilizarov fixation. Injury. 2008;39(2):196–202. https://doi.org/10.1016/j.injury.2007.09.003
- Karunakaran A, Rajamani SG. A prospective study of locking plate fixation in tibial plateau fractures. Int J Orthop Sci. 2018;4(1):1133–41. https://doi.org/10.22271/ortho.2018.v4.i1p.159
