Original Article
Volume: 37 | Issue: 3 | Published: Sep 25, 2021 | Pages: 151 - 158 | DOI: 10.51441/BioMedica/5-503
Prednisone combined with antiviral agents for the treatment of early idiopathic brachial plexus neuritis: report of five cases
Authors: Xueyuan Li , Miao Yu , Miaozhong Li , Kyaw Thura , Xiaoling Zhou , Chen Hong
Article Info
Authors
Xueyuan Li
Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang- China.
Miao Yu
Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang- China.
Miaozhong Li
Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang- China.
Kyaw Thura
Mandalay Orthopaedic Hospital, University of Medicine, Mandalay - Myanmar.
Xiaoling Zhou
Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang- China.
Chen Hong
Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang –China.
Publication History
Received: April 19, 2021
Accepted: August 11, 2021
Published: September 25, 2021
Abstract
Background and Objective: The aim of this study was to report the short-term outcomes of early idiopathic brachial plexus neuritis after low-dose corticosteroid combined with antiviral agent.
Methods: Five patients with early brachial plexus neuritis presenting from April to June 2019 were included in this study. According to individual patient conditions, electromyography (EMG), nerve B-ultrasound and/or brachial plexus magnetic resonance imaging (MRI) were performed. After the diagnosis was confirmed, modified conservative treatments were initiated, including low-dose corticosteroid therapy and antiviral therapy for 2 weeks each while neurotrophic therapy for 4 weeks.
Results: Of the five patients, only two patients had symptoms of pain at onset, and three patients had sensory disturbances. Two patients reported a common cold before onset. The lesion involved the upper trunk of the brachial plexus in two patients. MRI showed slightly intense signals, of which one patient also had supraclavicular lymph node augmentation. The other three patients suffered ipsilateral radial nerve (RN) palsy. At 1 month of modified treatment, four patients recovered well with almost complete shoulder and hand movements; however, their muscle strength was still weaker comparing with the contralateral side. One patient restored full range of motion after surgery in 2 months.
Conclusion: Early treatment is the key to good prognosis in patients with brachial plexus neuritis. Antiviral therapy combined with lowdose corticosteroid therapy may be superior to traditional treatment alone. In terms of early diagnosis, the clinical value of imaging examinations such as ultrasound and MRI is more specific as compared to that of EMG.
Keywords: Brachial plexus neuritis, Treatment, Corticosteroid, Neuralgic amyotrophy, Antiviral.
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 37(3):151-158
CASE SERIES
Prednisone combined with antiviral agents for the treatment of early idiopathic brachial plexus neuritis: report of five cases
Xueyuan Li1, Miao Yu1, Miaozhong Li1, Kyaw Thura2, Xiaoling Zhou1, Chen Hong1*
Received: 19 April 2021 Revised date: 14 July 2021 Accepted: 11 August 2021
Correspondence to: Chen Hong
*Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang, China.
Email: chenhong_6612@163.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
The aim of this study was to report the short-term outcomes of early idiopathic brachial plexus neuritis after low-dose corticosteroid combined with antiviral agent.
Methods:
Five patients with early brachial plexus neuritis presenting from April to June 2019 were included in this study. According to individual patient conditions, electromyography (EMG), nerve B-ultrasound and/or brachial plexus magnetic resonance imaging (MRI) were performed. After the diagnosis was confirmed, modified conservative treatments were initiated, including low-dose corticosteroid therapy and antiviral therapy for 2 weeks each while neurotrophic therapy for 4 weeks.
Results:
Of the five patients, only two patients had symptoms of pain at onset, and three patients had sensory disturbances. Two patients reported a common cold before onset. The lesion involved the upper trunk of the brachial plexus in two patients. MRI showed slightly intense signals, of which one patient also had supraclavicular lymph node augmentation. The other three patients suffered ipsilateral radial nerve (RN) palsy. At 1 month of modified treatment, four patients recovered well with almost complete shoulder and hand movements; however, their muscle strength was still weaker comparing with the contralateral side. One patient restored full range of motion after surgery in 2 months.
Conclusion:
Early treatment is the key to good prognosis in patients with brachial plexus neuritis. Antiviral therapy combined with low-dose corticosteroid therapy may be superior to traditional treatment alone. In terms of early diagnosis, the clinical value of imaging examinations such as ultrasound and MRI is more specific as compared to that of EMG.
Keywords:
Brachial plexus neuritis, treatment, corticosteroid, neuralgic amyotrophy, antiviral.
Introduction
Idiopathic brachial plexus neuritis, also known as Parsonage-Turner syndrome (PTS),1 manifests as unexplained pain in the early stage with acute muscle weakness in the upper limbs. Muscle atrophy may occur in a short period of time. The etiology of the disease has not yet been elucidated; however, mainstream opinions are primarily focused on virus infection and immuno-mediated theory.2,3 Classic treatment strategies include the use of anti-inflammatory and analgesic agents, electrical nerve stimulation, physiotherapy, and pulse corticosteroid therapy. However, the overall outcome for PTS patients is far from satisfactory and the sequelae involving a certain degree of dysfunction cannot be avoided.4 There have been no reports in the literature of the use of antivirals for the treatment of idiopathic brachial plexus neuritis. Antiviral therapy is limited to patients with clear evidence of viral infection, for instance, herpes zoster infection.5 In view of the fact that the classic treatment strategy cannot meet the clinical needs of patients, we adjusted early treatment in five consecutive patients with brachial plexus neuritis with an onset of less than 1 month from April to June 2019 in an outpatient clinic. In addition to traditional treatments, antiviral therapy was administered. The predisposing factors and outcomes of 5 patients were analyzed and the progress in treatment for brachial plexus neuritis was ascertained.
Methods
From April to June 2019, our medical team consecutively treated five patients with clinical symptoms consistent with early idiopathic brachial plexus neuritis in the outpatient clinic of Ningbo Sixth Hospital, Zhejiang, China (Table 1). There were four males and one female. The shortest disease onset was within 1 day, and the longest was 1 month. The nerve lesion involvement was seen (Table 1). In the patient with disease onset of 1 month, the upper trunk was affected accompanied by an obvious atrophy of the infraspinatus and deltoid muscle. Disease onset for the other patients was within 2 weeks, and no muscle atrophy was noted. Of the five patients, three had accompanying sensory disorders while only two had obvious symptoms. Only two of the five patients had a history of pain. Reduced muscle strength was seen in all patients in the short time since onset manifesting as the inability in extension of wrist and finger or shoulder abduction. In terms of predisposing factors, two patients had a clear history of cold before onset, only one had a history of fever. Two patients had a long history of alcohol addiction, and one patient worked as a heavy manual labor. One patient had a history of diabetes.
We collected a detailed medical history of all five patients which included possible predisposing factors at the time of the clinic visit. The extent and time period of pain were assessed and skin sensation and movement of the affected upper limb were examined. Muscle strength of the upper limb was carefully examined and recorded. Routine blood work, blood glucose and blood biochemical panels were completed and abnormal results were recorded. Auxiliary examinations such as neurosonography, were used to examine specific nerves of upper extremity. The three patients with radial and posterior interosseous nerve (PIN) involvement received ultrasound examination. The morphological changes in the affected nerves and potential entrapment structures by comparing bilateral nerve images was observed. Magnetic resonance imaging (MRI) of the brachial plexus was performed in two patients with upper trunk involvement. Electromyography (EMG) was not recommended within 3 weeks of injury. Therefore, only two patients beyond 3 weeks of onset underwent EMG. Cervical MRI was also used to rule out other diseases, such as cervical spondylosis.
In terms of treatment, the first and second patients were treated with antiviral drug. On April 22, the first male patient presented with an inability to extend fingers 1-5 for 2 weeks. Prednisone (5 mg) was given orally twice daily for five consecutive days according to traditional treatment, but no effects were observed. The patient’s medical history revealed that he had a history of common cold without fever. Therefore, oseltamivir (75 mg) was added orally twice a day on the basis of corticosteroid therapy. The patient recovered obviously in the next week. We documented the course of continuous recovery during follow-up (Figure 1).
On April 26, the second patient presented with severe neck and shoulder pain with an inability to abduct the left shoulder for 10 days. MRI showed the brachial plexus nerve root edema with supraclavian and mediastinal enlarged lymph nodes noted on the affected side. Considering the possibility of acute viral infection, prednisone (5 mg) was administered orally twice a day for five consecutive days, and oral oseltamivir was administered concurrently, 75 mg twice daily for 10 days. Two weeks later, the treatment was changed to oral neurotrophic agents such as Mecobalamin. The patient was able to complete shoulder abduction movements 10 days after treatment with a muscle strength (M3) (Figure 2).
The other three patients had no evidence of viral infection. Prednisone was given 5 mg orally twice a day for five consecutive days for the first 2 weeks and oseltamivir 75 mg orally twice a day for a week. The treatment in the second week was the same as that in the first week. Simple neurotrophic therapy and oral neurotrophic agents, such as Mecobalamin, were given in the following 2 weeks. Patients were examined weekly for 1 month, and the recovery process was recorded (Figures 3-5). The fourth patient underwent RN neurolysis after 1.5 month of conservative treatment because of unsatisfactory recovery.
Table 1. Clinical features of five enrolled patients.
| Case | Date of consultation | Gender | Age (year) | Inducement | Clinical onset | Involved nerves (according to severity) | Pain (VAS) | Sensory change |
|---|---|---|---|---|---|---|---|---|
| 1 | 2019/4/22 | Male | 64 | Cold history | 14 days | PIN + RN + MN | 0 | No |
| 2 | 2019/4/26 | Female | 31 | Strengthen work | 10 days | Suprascapular + axillary + muscular cutaneous | 7 | No |
| 3 | 2019/5/6 | Male | 52 | Cold and fever history | 30 days | Suprascapular + axillary + muscular cutaneous | 0 | Numbness over lateral arm |
| 4 | 2019/5/27 | Male | 55 | Chronic alcohol ingestion | 1 day | PIN + RN + MN | 3-4 | No |
| 5 | 2019/5/24 | Male | 54 | Chronic alcohol ingestion | 14 days | RN + MN + UN | 0 | Numbness over dorsal thumb |
PIN, posterior interosseous nerve; RN, radial nerve; MN, median nerve; UN, ulnar nerve.
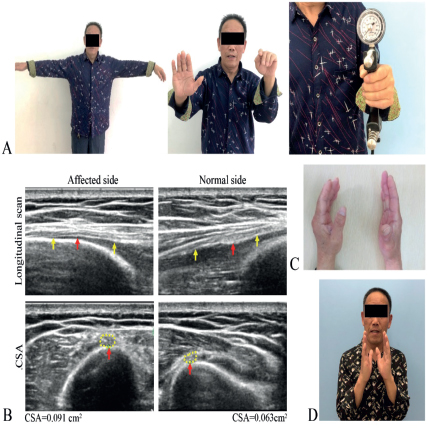
Figure 1. A 64-year-old male present with left wrist and finger extension failure 14 days. A. Wrist extension and 1-5 finger extension failure with decreased grip strength. B. B-Ultrasound (BUS) indicated left RN augmentation over middle of radial groove. C. After 2 weeks of conservative treatment 1-5 finger extension strength improved to M2. D. After 3 weeks, left wrist and finger extension strength restored to M3.
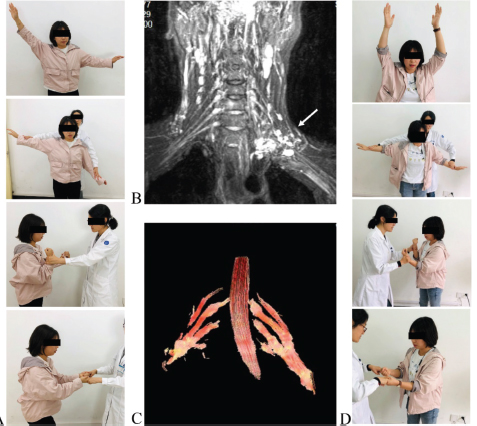
Figure 2. A 31-year-old female complained left shoulder abduction failure for 10 days. A. Clinical presentation: Left shoulder abduction (M2 ,Elbow flexion (M3), Grip strength (M4) B. MRI for brachial plexus, white arrow indicate limb notes C. DTI (diffusion tensor imaging) of brachial plexus nerve bundle showed that the left brachial plexus nerve was swollen and thickened compared with the right side. D. 10 days later: shoulder joint elevation recovered, shoulder abductor strength recovered to level 4, elbow flexion and grip strength increased.
Results
The lesions of two patients involved the upper trunk of the brachial plexus. In three patients, the lesion mainly involved the radial nerve (RN) and PINs, one of which was accompanied by mild involvement of the median and ulnar nerves (UN). Of the five patients, only two patients had symptoms of pain at disease onset, three patients had sensory disturbances, and two had a history of common cold. The shortest disease onset was within a day, and the longest was a month. Raised blood glucose levels were reported in one patient. In terms of auxiliary examinations, MRI of the brachial plexus showed slightly enhanced signals of the affected side in two patients with upper trunk involvement, accompanied by an enlarged supraclavicular lymph node of the affected side in one patient. B-ultrasound of the RNs in the other three patients showed extensive nerve swelling but no obvious narrowing and hourglass changes. Two patients had a disease onset longer than 2 weeks and underwent EMG, which showed severe RN injury in one patient and upper trunk (superior scapular nerve, axillary nerve) injury in the other patient. After 1 month of conservative treatment, four patients recovered satisfactorily, with full range of motion except muscle strength reduced. Only one patient with diabetes had RN damage and median UN involvement. After 1 month of conservative treatment, the median nerve (MN) symptoms were well-recovered, while RN improvement was not obvious, although the EMG re-examination showed signs of nerve regeneration. Patient was consulted for surgical exploration. During the operation, the RN was seen edematous with poor elasticity, suspicious vascular bundle and the arcade of Frohse were released. These findings were consistent with the results of the ultrasound. After a 1.5-month follow-up, wrist and finger extension were recovered (Figure 4). All patients had no obvious toxic effects or side effects from the medication. In the fourth patient, a transient abnormal increase in blood glucose levels occurred when taking prednisone and was controlled by insulin therapy. The functional analyses of all patients before and after treatment are shown in Figures 1-5. All patients were followed up over telephone for 6 months to 1 year, and no recurrence was reported.
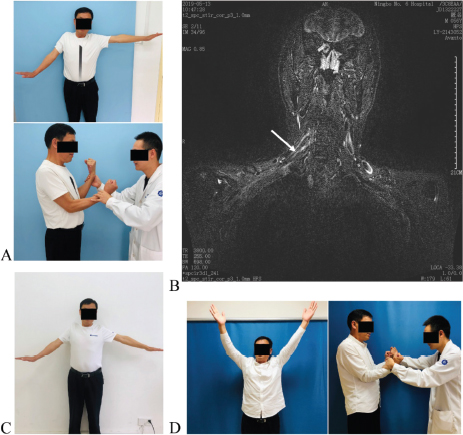
Figure 3. A. Clinical presentation on May 6: Muscle strength of right shoulder abduction and elbow flexion was very weak. B. Right brachial plexus MRI, Arrow indicated C5, C6 nerve roots T2 signal enhancement. C. Conservative treatment 1 week, right shoulder abduction improved. D. 1 month later, patient restored full Range of motion (ROM) of shoulder abduction and improved elbow flexion.
Discussion
Since Parsonage and Turner reported this disease in 1943,1 idiopathic brachial plexus neuritis has been known as PTS, as well as neuralgic amyotrophy. The incidence was previously thought to be relatively rare, with 2-3 cases per 100,000 people.2,3 However, van Alfen6, found that the annual incidence was 1/1,000. Seror7 and van Eijk et al.8 expressed similar opinions in their review. However, a century has passed, and our knowledge about the etiology and treatment of brachial plexus neuritis has not progressed substantially.7 The existing research on early treatment is limited. The course of brachial plexus neuritis in most of patients is 6 months to 3 years, during which the pain and muscle weakness can considerably impact patients’ work and routine life.6,7 A case-control study of pulse corticosteroid treatment by van Eijk et al.9 showed that the short-term recovery rate after treatment reached 18% which was statistically significant compared with the non-corticosteroid treatment group. As a result, early pulse corticosteroid therapy has become part of the classic treatment.8 Other acute treatment options include expensive immunotherapy but have only been reported in individual cases.10,11 Short-term recovery after conservative treatment of PTS is disappointing. Antiviral therapy is rarely reported in the literature, unless there is clear evidence of viral infection. In this study, four consecutive patients recovered satisfactorily within 1 month after antiviral treatment, and one patient recovered satisfactorily after 2 months of treatment with surgery.
Past studies suggest that brachial plexus neuritis is a benign self-limiting disease that can be cured even without treatment or with simple conservative treatment.2,3,12 However, more studies in recent years indicate that the prognosis of patients with brachial plexus neuritis is not ideal. van Alfen et al.6 reported a large sample-sized study, and approximately 2/3 of patients after conservative treatment had long-term dysfunction. Seror7 reported that 80% of patients treated conservatively did not recover until 6 months or even 3 years and that 20% of patients did not recover. Park et al.13 reported 11 patients with anterior interosseous nerve (AIN) spontaneous paralysis who did not respond to 7-month conservative treatment and then underwent surgery. Although the outcomes of surgical neurolysis are satisfactory, the recovery process is long. Sigamoney et al.14 reviewed data of patients with spontaneous PIN palsy and proposed that in patients with no early signs of recovery within the first month of onset, only 21% will recover within 1 year. Therefore, the authors advocate for early surgical exploration for patients who show no signs of recovery for 6 weeks. We chose a more aggressive surgical treatment for the fourth patient, who did not achieve satisfactory outcome at 1 month following conservative treatment. Fortunately, the patient recovered within 1.5 months after surgery. Three months later, the muscle strength was further restored to M4 (Figure 4).
Early symptoms of brachial plexus neuritis include typical pain, followed by weakness and muscle atrophy in the upper limbs in a short time period. Most literature reports that the incidence of pain in patients with brachial plexus neuritis exceeds 90%.2,15 However, Milner et al.16 reported 38 patients with PTS, of whom 1/3rd did not have pain symptoms. Akane et al.17 reported 51 cases of neuropathic muscular atrophy with a pain incidence of 52.9%. In the absence of acute pain, acute onset and muscle weakness, numbness, and muscle atrophy in a short time period may be more reliable diagnostic evidence. Of the five patients reported in this study, only two had pain symptoms. Studies reported by a group of hand surgeons elaborate that involvement of the posterior and AIN is more common than other nerves. In fact, brachial plexus neuritis can involve any nerve in the brachial plexus; therefore, the clinical manifestations are diverse.16,17 Two of the five patients presented with involvement of the upper trunk, two patients had predominant involvement of the RN and one had the involvement of PIN. All patients showed multiple nerve involvement at an early stage, but to varying degrees.
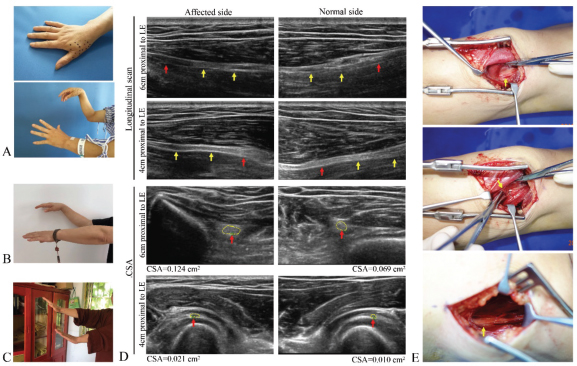
Figure 4. Case 4. A. Clinical presentation on May 27: Numbness over right first web space, right wrist and finger extension failed. B. 5 weeks later, Right (R) wrist and finger extension improved to M3. C. 3 months after the operation, the muscle power restored to M4. D. BUS right RN showed augmentation at the 6 cm proximal to the LE and 4 cm distal to LE, the Cross sectional area (CSA) was larger than the left side. The arrows and dotted lines show the deep branches of the RN and the red arrows show the swollen area. E. RN neurolysis at 6 cm above LE, A vascular nerve bundle across PIN was released at 4 cm distal to LE. The following picture shows the Froche arch release.
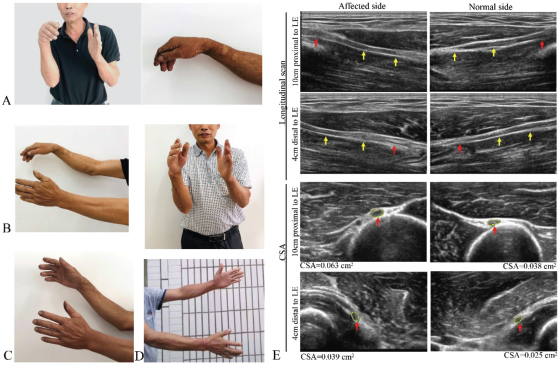
Figure 5. A. Clinical presentation on May 27: Right wrist and 1-5 fingers extension failure; B. 1 week after treatment, the muscle strength of right extensor wrist and fingers was restored to level 2; C. 17 days later, right wrist and finger extension movement significantly improved. D. After 4 weeks of conservative treatment, the extensor muscle strength restored to M3. E. Ultrasound showed right RN augmentation 10 cm proximal to lateral supracondlye, PIN augmentation 4 cm distal to lateral supracondyle. Arrows and dotted lines indicate the RN and the PIN; red arrow indicates nerve augmentation LE.
The uncertainty of the etiology makes the clinical diagnosis of brachial plexus neuritis quite challenging. It needs to be differentiated from many related diseases, such as frozen shoulder, rotator cuff injury, thoracic outlet syndrome, nerve root cervical spondylosis, and peripheral nerve entrapment such as superior scapular nerve compression, RN compression and AIN compression. A detailed clinical history and physical examination can reveal multiple nerve involvement with early brachial plexus neuritis. However, mild nerve involvement is often ignored. In the two patients with upper trunk involvement, the main complaint was shoulder abduction limitations, but careful examination revealed significantly impacted muscle strength during elbow flexion (Figures 2 and 3). The physical examination revealed numbness in the MN ulnar innervation area and decreased grip strength in three patients with RN involvement and a slight impact on grip strength in the other two patients. Auxiliary examinations, such as nerve B-ultrasound, MRI, and EMG, are essential for diagnosis. Fukushima18 concluded that MRI can show T2-weighted high intense signals in the proximal nerve of early-stage PTS patients. In addition, both MRI and B-ultrasound can help to find swelling, distortion, narrowing, and hour-glass changes19,20 in a single nerve beyond the brachial plexus and can provide references for clinicians to choose the appropriate treatment plan. B-ultrasound is a more cost-friendly and convenient method. While EMG cannot indicate early stage of nerve injury. In our group, two patients whose symptoms occurred within less than 2 weeks did not receive EMG until 3 weeks after onset, the results were consistent with clinical manifestations of early axonal damage. Three patients who had RN injury, B-ultrasound showed varying degrees of edema in the affected nerve. Two patients with brachial plexus neuritis of the upper trunk underwent MRI of the brachial plexus which showed edema of the corresponding affected nerve root and enlarged cervical lymph nodes in a female patient. Nerve B-ultrasound is especially helpful to guide nerve surgery. In the fourth patient in this study, we found significant edema of the RN bundle at the level of the arcade of Frohse above and below the lateral epicondyle (LE) of the humerus which was completely consistent with the ultrasound findings.
The reasons for hourglass-like changes in nerves are still unclear in the literature. Pan et al.21 and Nakagawa and Hirata22 found that neural hourglass-like changes occurred in patients with brachial plexus neuritis that had been diagnosed. Wang et al.23 reviewed data of 22 patients with spontaneous hourglass-like changes in the nerves of the upper extremities. No evidence of compression was found during surgery. MRI and ultrasound showed no hourglass changes or signs of compression on the nerve in this study.
Ortiz Torres and Mesfin4 demonstrated in a review that idiopathic brachial plexus neuritis is often associated with recent viral infections. The causes of infection include Haemophilus influenzae, Coxsackie virus, Parvovirus B19, Cytomegalovirus, Herpes zoster, Human immunodeficiency virus, Salmonella typhi etc. Many studies support this statement.8,24-26 In addition, reports regarding hepatitis E virus leading to brachial plexus neuritis have increased significantly.27,28 In the recommendations for early treatment, no researcher has directly recommended antiviral treatment unless there is a clear evidence of viral infection. Neurophysiologists have reported that herpes zoster virus can cause typical brachial plexus neuritis.29 The onset of herpes zoster virus infection is characterized by secondary brachial plexus damage including typical muscle atrophy. Idiopathic brachial plexus neuritis does not cause a rash, but pain and nerve damage are indeed very similar. None of the five patients reported in this study had a rash specific to herpes virus.
Conclusion
Prednisone combined with antiviral therapy achieves 80% cure rate in 1 month and 100% cure rate in 3 months in patients with early idiopathic brachial plexus neuritis which is quite a higher recovery rate than prednisone alone. Although there is no conclusive evidence of viral infection in all five patients reported in the study, atypical viral infections cannot be ruled out. Therefore, we strongly speculate that the success of antiviral treatment may not be a simple coincidence.
Limitations of the study
The limitations of this study include small sample size and single-center design, as well as short follow-up period.
Acknowledgement
The authors would like to thank our patients and their families for their contribution. Special thanks to Dr. Guoqing Shao for assistance in nerve B-ultrasound examination, to Dr. Xin Wang, Dr. Haoliang Hu, Dr. Mintao Tian, Dr. Linhai Liu and Dr. Hui Zhang for data collection and analysis on this project.
List of Abbreviations
| AIN | Anterior interosseous nerve |
| EMG | Electromyography |
| LE | Lateral epicondyle |
| MN | Median nerve |
| MRI | Magnetic resonance imaging |
| PIN | Posterior interosseous nerve |
| PTS | Parsonage-Turner syndrome |
| RN | Radial nerve |
| UN | Ulnar nerve |
Conflict of interest
None to declare.
Grant support and financial disclosure
This study was approved and funded by Ningbo Science and Technology Planning Project, China (Ref No. 2019C50047).
Ethical approval
This study was approved by the Ethics Committee of Ningbo Sixth Hospital, Zhejiang, China (Ref: L2020004).
Author’s contribution
XL, MY and ML, HC: Conception and design of study, acquisition and analysis of data, drafting the manuscript.
KT, and XZ: Critical revision of the manuscript with important intellectual content.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Author details
Xueyuan Li1, Miao Yu1, Miaozhong Li1, Kyaw Thura2, Xiaoling Zhou1, Chen Hong1
- Department of Hand Surgery, Ningbo Sixth Hospital, Zhejiang, China
- Department of Surgery, Mandalay Orthopaedic Hospital, University of Medicine, Mandalay, Myanmar
References
- Davidson C, Gordon N. Shoulder-girdle syndrome. Lancet. 1948;252(6524):433. https://doi.org/10.1016/S0140-6736(48)91006-X
- Tjoumakaris FP, Anakwenze OA, Kancherla V, Pulos N. Neuralgic amyotrophy (Parsonage-Turner syndrome). J Am Acad Orthop Surg. 2012;20(7):443–9. https://doi.org/10.5435/JAAOS-20-07-443
- Hosey RG, Rodenberg RE. Brachial neuritis: an uncommon cause of shoulder pain. Orthopedics. 2004;27(8):833–6. https://doi.org/10.3928/0147-7447-20040801-17
- Ortiz Torres M, Mesfin FB. Brachial plexitis (Parsonage Turner syndrome, brachial neuropathy, brachial radiculitis). Treasure Island, FL: StatPearls Publishing; 2020.
- Melikoglu M, Melikoglu MA. An unusual cause of shoulder pain; herpes zoster induced brachial plexopathy, a case report and review of the literature. J Back Musculoskelet Rehabil. 2013;26(3):243–5. https://doi.org/10.3233/BMR-130377
- van Alfen N, van Eijk JJ, Ennik T, Flynn SO, Nobacht IE, Groothuis JT, et al. Incidence of neuralgic amyotrophy (Parsonage Turner syndrome) in a primary care setting--a prospective cohort study. PLoS One. 2015;10(5):e0128361. https://doi.org/10.1371/journal.pone.0128361
- Seror P. Neuralgic amyotrophy. An update. Joint Bone Spine. 2017;84(2):153–8. https://doi.org/10.1016/j.jbspin.2016.03.005
- van Eijk JJ, Groothuis JT, van Alfen N. Neuralgic amyotrophy: an update on diagnosis, pathophysiology, and treatment. Muscle Nerve. 2016;53(3):337–50. https://doi.org/10.1002/mus.25008
- van Eijk JJ, van Alfen N, Berrevoets M, van der Wilt GJ, Pillen S, van Engelen BG. Evaluation of prednisolone treatment in the acute phase of neuralgic amyotrophy: an observational study. J Neurol Neurosurg Psychiatry. 2009;80(10):1120–4. https://doi.org/10.1136/jnnp.2008.163386
- Johnson NE, Petraglia AL, Huang JH, Logigian EL. Rapid resolution of severe neuralgic amyotrophy after treatment with corticosteroids and intravenous immunoglobulin. Muscle Nerve. 2011;44(2):304–5. https://doi.org/10.1002/mus.22100
- Nakajima M, Fujioka S, Ohno H, Iwamoto K. Partial but rapid recovery from paralysis after immunomodulation during early stage of neuralgic amyotrophy. Eur Neurol. 2006;55(4):227–9. https://doi.org/10.1159/000093875
- Smith CC, Bevelaqua AC. Challenging pain syndromes: Parsonage-Turner syndrome. Phys Med Rehabil Clin N Am. 2014;25(2):265–77. https://doi.org/10.1016/j.pmr.2014.01.001
- Park IJ, Roh YT, Jeong C, Kim HM. Spontaneous anterior interosseous nerve syndrome: clinical analysis of eleven surgical cases. J Plast Surg Hand Surg. 2013;47(6):519–23. https://doi.org/10.3109/2000656X.2013.791624
- Sigamoney KV, Rashid A, Ng CY. Management of atraumatic posterior interosseous nerve palsy. J Hand Surg Am. 2017;42(10):826–30. https://doi.org/10.1016/j.jhsa.2017.07.026
- van Alfen N, van Engelen BG. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006;129(Pt 2):438–50. https://doi.org/10.1093/brain/awh722
- Milner CS, Kannan K, Iyer VG, Thirkannad SM. Parsonage-Turner syndrome: clinical and epidemiological features from a hand surgeon’s perspective. Hand (N Y). 2016;11(2):227–31. https://doi.org/10.1177/1558944715627246
- Akane M, Iwatsuki K, Tatebe M, Nishizuka T, Kurimoto S, Yamamoto M, et al. Anterior interosseous nerve and posterior interosseous nerve involvement in neuralgic amyotrophy. Clin Neurol Neurosurg. 2016;151:108–12. https://doi.org/10.1016/j.clineuro.2016.11.001
- Fukushima K. [Clinical features and MRI characteristics in neuralgic amyotrophy]. Rinsho Shinkeigaku. 2014;54(12):1053–5. https://doi.org/10.5692/clinicalneurol.54.1053
- Aranyi Z, Csillik A, Devay K, Rosero M, Barsi P, Bohm J, et al. Ultrasonographic identification of nerve pathology in neuralgic amyotrophy: enlargement, constriction, fascicular entwinement, and torsion. Muscle Nerve. 2015;52(4):503–11. https://doi.org/10.1002/mus.24615
- Lieba-Samal D, Jengojan S, Kasprian G, Wober C, Bodner G. Neuroimaging of classic neuralgic amyotrophy. Muscle nerve. 2016;54(6):1079–85. https://doi.org/10.1002/mus.25147
- Pan YW, Wang S, Tian G, Li C, Tian W, Tian M. Typical brachial neuritis (Parsonage-Turner syndrome) with hourglass-like constrictions in the affected nerves. J Hand Surg Am. 2011;36(7):1197–203. https://doi.org/10.1016/j.jhsa.2011.03.041
- Nakagawa Y, Hirata H. Hourglass-like constriction of the brachial plexus in the posterior cord: a case report. Neurosurgery. 2018;82(1):E1–5. https://doi.org/10.1093/neuros/nyx171
- Wang Y, Liu T, Song L, Zhang Z, Zhang Y, Ni J, et al. Spontaneous peripheral nerve palsy with hourglass-like fascicular constriction in the upper extremity. J Neurosurg. 2019;131(6):1876–86. https://doi.org/10.3171/2018.8.JNS18419
- Shaikh MF, Baqai TJ, Tahir H. Acute brachial neuritis following influenza vaccination. BMJ Case Rep. 2012;2012:243–5. https://doi.org/10.1136/bcr-2012-007673
- Vanpee D, Laloux P, Gillet JB, Esselinckx W. Viral brachial neuritis in emergency medicine. J Emerg Med. 2000;18(2):177–9. https://doi.org/10.1016/S0736-4679(99)00189-4
- Jeevarethinam A, Ihuoma A, Ahmad N. Herpes zoster brachial plexopathy with predominant radial nerve palsy. Clin Med (Lond). 2009;9(5):500–1. https://doi.org/10.7861/clinmedicine.9-5-500
- Njabom CN, Gilbert A, Brasseur E, Zandona R, Ghuysen A, D’Orio V. Parsonage-Turner syndrome as a rare extrahepatic complication of hepatitis e infection. Eur J Case Rep Intern Med. 2019;6(8):001208. https://doi.org/10.12890/2019_001208
- Aranyi Z, Szpisjak L, Szoke K. Multiphasic presentation of neuralgic amyotrophy associated with hepatitis E virus infection. Muscle Nerve. 2020;61(1):108–10. https://doi.org/10.1002/mus.26722
- Ismail A, Rao DG, Sharrack B. Pure motor herpes zoster induced brachial plexopathy. J Neurol. 2009;256(8):1343–5. https://doi.org/10.1007/s00415-009-5149-8
