Original Article
Volume: 37 | Issue: 3 | Published: Sep 25, 2021 | Pages: 159 - 163 | DOI: 10.51441/BioMedica/5-504
Diagnostic accuracy of TI-RADS classification in differentiating benign and malignant thyroid nodules-a study from Southern Punjab, Pakistan
Authors: Sumera Nighat , Mahwish Zahra , Azhar Mahmood Javed , Shabbir Ahmad , Sadia Anwar , Usama Hussain Kamal
Article Info
Authors
Sumera Nighat
Assistant Professor, Department of Radiology, Bakhtawar Amin Medical & Dental College, Multan - Pakistan.
Mahwish Zahra
Senior Registrar, Department of Radiology, Children Hospital and Institute of Child Health, Multan- Pakistan.
Azhar Mahmood Javed
Associate Professor and Head, Department of Radiology, Children Hospital and Institute of Child Health, Multan-Pakistan.
Shabbir Ahmad
Assistant professor, Department of Surgery, Bakhtarwar Amin Medical and Dental College, Multan- Pakistan.
Sadia Anwar
Professor, Department of Pathology, Gujranwala Medical College, Gujranwala-Pakistan.
Usama Hussain Kamal
First Year Medical Student, Services Institute of Medical Sciences, Lahore - Pakistan.
Publication History
Received: May 02, 2021
Accepted: August 08, 2021
Published: September 25, 2021
Abstract
Background and Objective: Thyroid imaging reporting and data system (TI-RADS) is developed to determine the risk of malignancy in patients with thyroid nodules. The aim of this study was to determine the diagnostic accuracy of TI-RADS classification for diagnosing malignant thyroid nodules taking Fine needle aspiration cytology (FNAC) as a gold standard in the local population.
Methods: In this cross-sectional validation study, 201 patients presenting with thyroid nodules at the Department of Radiology, Bakhtawar Amin Hospital Multan, Pakistan from July 2020 to December 2020 were included. In all patients, thyroid nodules were evaluated on grey scale (B-mode) modality. TI-RADS score was calculated for each patient. Patients with TI-RADS score 4 and 5 were labelled as having malignant nodules. After that FNAC samples were taken and sent for histopathologic evaluation of thyroid nodules. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TI-RADS taking FNAC as a gold standard were determined.
Results: The mean age of the patients was 47.8 ± 4.5 years; there were 129 (67.2%) women and 72 (35.82%) men. There were 42 patients who tested true positive and 36 patients tested false positive and 12 patients were false negative and 111 patients true negative. The TIRADS sensitivity was 77.8%, specificity was 75.5%, PPV was 53.8%, and NPV 90.2%. the diagnostic accuracy was 76.1%.
Conclusion: Differentiating benign thyroid nodules from malignant using the TI-RADS score has a high diagnostic accuracy. Our study results support the TIRADS as a first-line imaging evaluation for diagnosis of thyroid malignancy.
Keywords: Thyroid nodules, Ultrasonography, Fine needle aspiration cytology, TI-RADS.
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 37(3):159-163
ORIGINAL ARTICLE
Diagnostic accuracy of TI-RADS classification in differentiating benign and malignant thyroid nodules-a study from Southern Punjab, Pakistan
Sumera Nighat1*, Mahwish Zahra2, Azhar Mahmood Javed3, Shabbir Ahmad4, Sadia Anwar5, Usama Hussain Kamal6
Received: 02 May 2021 Revised date: 28 July 2021 Accepted: 08 August 2021
Correspondence to: Sumera Nighat
*Department of Radiology, Bakhtawar Amin Medical & Dental College, Multan, Pakistan.
Email: drsumeranighat@msn.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
Thyroid imaging reporting and data system (TI-RADS) is developed to determine the risk of malignancy in patients with thyroid nodules. The aim of this study was to determine the diagnostic accuracy of TI-RADS classification for diagnosing malignant thyroid nodules taking Fine needle aspiration cytology (FNAC) as a gold standard in the local population.
Methods:
In this cross-sectional validation study, 201 patients presenting with thyroid nodules at the Department of Radiology, Bakhtawar Amin Hospital Multan, Pakistan from July 2020 to December 2020 were included. In all patients, thyroid nodules were evaluated on grey scale (B-mode) modality. TI-RADS score was calculated for each patient. Patients with TI-RADS score 4 and 5 were labelled as having malignant nodules. After that FNAC samples were taken and sent for histopathologic evaluation of thyroid nodules. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TI-RADS taking FNAC as a gold standard were determined.
Results:
The mean age of the patients was 47.8 ± 4.5 years; there were 129 (67.2%) women and 72 (35.82%) men. There were 42 patients who tested true positive and 36 patients tested false positive and 12 patients were false negative and 111 patients true negative. The TI-RADS sensitivity was 77.8%, specificity was 75.5%, PPV was 53.8%, and NPV 90.2%. the diagnostic accuracy was 76.1%.
Conclusion:
Differentiating benign thyroid nodules from malignant using the TI-RADS score has a high diagnostic accuracy. Our study results support the TIRADS as a first-line imaging evaluation for diagnosis of thyroid malignancy.
Keywords:
Thyroid nodules, ultrasonography, fine needle aspiration cytology, TI-RADS.
Introduction
Thyroid diseases account for one of the commonest health problems in South Asia, especially in Pakistan due to iodine deficiency in the diet; the prevalence of men being higher than the women.1 Thyroid nodules can be identified using high-frequency ultrasound (US) with a high prevalence rate of 19% to 67% in different populations.2 Based on research reports, up-to 90% of nodules are benign and up-to 10% of these are malignant.3 The early detection and diagnosis between benign and malignant thyroid nodules can be lifesaving. Fine-needle aspiration cytology (FNAC) further augments the conclusive diagnosis. The ultrasonography (USG) is a non-invasive, cost-effective, and safe method. Once any suspicious nodule is reported by the clinician, the US-guided FNAC is planned as the clinical management is based on accurate diagosis.4 FNA is a simple and minimally invasive way of diagnosing thyroid nodules.5 The size, shape, micro-calcifications, and echogenicity are the key features to identify evidence of malignancy in the thyroid nodules.6
Worldwide, many classification systems are available based on the risk of thyroid malignancy. Thyroid imaging reporting and data system (TI-RADS) has a high sensitivity for assessment of thyroid malignancy.7
The present study aims to determine the diagnostic accuracy of TI-RADS classification for diagnosing malignant thyroid nodules taking FNAC as a gold standard in a local population of Southern Punjab.
Methods
In this cross-sectional validation study, 201 patients who were referred for ultrasonic evaluation of thyroid nodules to the Department of Radiology, Bakhtawar Amin Hospital Multan, Pakistan within duration of 06 months (July 2020 to December 2020) were included. Patients with already diagnosed carcinoma of thyroid and/or patients with exclusively cystic nodules were excluded. Informed consent was taken from all the patients and Ethical approval was obtained from Institutional Ethical Committee.
In all patients, USG was done using VERSANA Essential (GE Healthcare) machine. Thyroid nodules were evaluated on grey scale (B-mode) modality using high frequency (12 MHz) probe. All USG were done and analyzed by consultant radiologists and TI-RADS score was calculated. Fine-needle aspiration cytology was done and sent to the histopathology department for the diagnosis of malignancy. TI-RADS score was calculated and divided into four categories as given below in the concert flow diagram (Figure 1). Statistical analysis was done based on the cytology results.
Statistical analysis
Data were analyzed using SPSS v 20. Mean and the standard deviation were used for quantitative variable such as age. Qualitative variables like gender, presence/absence of malignant lesions using TI-RADS and FNAC. 2 × 2 contingency table was used to calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of TI-RADS taking FNAC as a gold standard.
Results
In this study, the age range of 201 patients of both genders, presenting with thyroid nodules, was between 18 and 65 years. The mean age was 47.8 ± 4.5 years; there were 129 (67.2%) females and 72 (35.82%) males. Mean tumors size was 22.5 ± 5.6 mm. Based on TI-RADS score 4 to 5, thyroid malignancy was suspected in 64 (31.84%) patients, while 137 (68.15%) patients were having a score less than 3, hence having the probability of benign lesions (Figure 2). FNAC confirmed malignancy (Figure 3) in 55 (27.36%) patients (Table 1). The TI-RADS sensitivity, specificity, PPV and NPV was 77.8%, 75.5%, 53.8%, and 90.2%. The diagnostic accuracy was 76.1%. (Table 2)
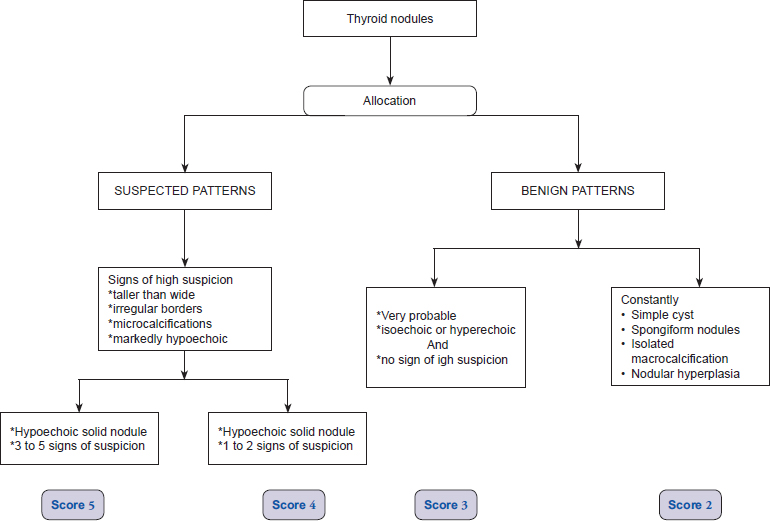
Figure 1. TI-RADS classification of thyroid nodules.
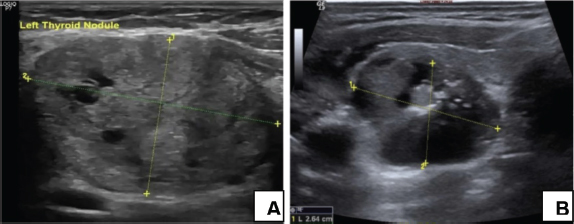
Figure 2. US showing benign (A) and malignant (B) thyroid nodules.
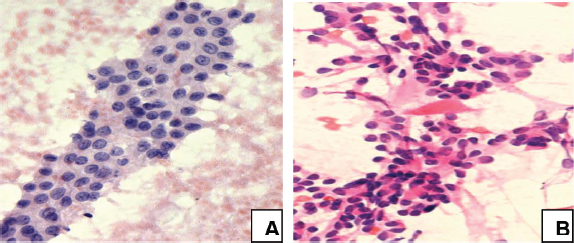
Figure 3. FNAC showing benign (A) and malignant (B) thyroid nodules.
Table 1. Baseline study and diagnostic variables.
| Clinical and diagnostic characteristics | N(%) |
|---|---|
| Age (years) | 47.8 ± 4.5 |
| Gender | |
| Male | 72 (35.82%) |
| Female | 129 (67.2%) |
| Size of tumor (mm) | 22.5 ± 5.6 |
| Diagnosis of malignant lesions. | |
| TI-RADS scoring | |
| 1-3 | 137 (68.15%) |
| 4-5 | 64 (31.84%) |
| FNAC | |
| Yes | 55 (27.36%) |
| No | 146 (72.64%) |
Discussion
Thyroid USG is tremendously important in the estimation of a suspicious thyroid nodule. Identifying such nodules is challenging for the radiologist which leads him to order FNAC for reaching a conclusive diagnosis. There are five characteristics for identifying malignancy in the suspicious thyroid nodules on radiography: 1. Calcification: micro and macro-calcifications8, 2. Hypoechogenicity inside the thyroid nodule, 3. Irregular margins, 4. Consistency- nodules with more solid tissue have higher chance of being malignant while the spongiform or cystic nodules are mostly considered benign9, and 5. Shape - a wider than taller nodule looks more benign than malignant and vice versa.10
Table 2. Comparison of TI-RADS and FNAC for detection of thyroid nodules.
| FNAC | Total | ||||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| TI-RADS | Positive | 42 | 36 | 78 | |
| Negative | 12 | 111 | 123 | ||
| Total | 54 | 147 | 201 | ||
Sensitivity 77.8% Specificity 75.5% PPV 53.8% NPV 90.2% Diagnostic Accuracy 76.1% |
|||||
A study conducted by Alam et al.11 reported the sensitivity (91.7%) and specificity (78.94%) of USG separating the benign from malignant thyroid nodules. Their PPV and NPV was 57.9% and 96.8%. Overall accuracy was 82%. Another multicenter study was conducted by Trimboli et al.12 who reported a higher sensitivity (93%) and NPV (96.8%) but lower specificity (67.9%) and PPV (48.2%) with the diagnostic accuracy of 74%. A study conducted by Macedo et al.13 evaluated the diagnostic accuracy of TI-RADS for differentiating malignant and benign tumors and concluded that TI-RADS is 100% sensitive, 61.1% specific, 100% PPV, and 63% NPV. All these results are in concordance with the present study (Table 2).
Conclusion
Differentiating benign thyroid from malignant thyroid nodules using the TI-RADS score has a high diagnostic accuracy. The study results support the TIRADS as a first-line imaging evaluation for the diagnosis of suspected thyroid malignancy.
Limitations of the study
It was a single center study and clinical variables like duration of disease, size, and age of the patients were not correlated with the suspicion of thyroid malignancy. The study may be supplemented with possible future larger scale studies in order to strengthen the conclusions drawn about study topic under discussion.
Acknowledgement
The authors hereby acknowledge the staff of Radiology and Pathology departments and the administration of Bakhtawar Amin Hospital Multan, Pakistan for providing the opportunity to proceed with the research.
List of Abbreviations
| FNAC | Fine needle aspiration cytology. |
| NPV | Negative predictive value. |
| PPV | Positive predictive value. |
| TI-RADS | Thyroid imaging reporting and data system. |
| USG | Ultrasonography. |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
The study was approved by the Institutional Ethical Review Committee vide Letter No. 0046-21/E.C/BAM&D.
Author’s contribution
SN, MZ: Conception of study, acquisition, analysis of data, drafting the manuscript; AMJ: Intellectual input, critical review of the manuscript; SA: Acquisition and critical revision of data; SA: Conception of study, analysis of data; UHK: Acquisition of data, drafting the manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Author details
Sumera Nighat1, Mahwish Zahra2, Azhar Mahmood Javed3, Shabbir Ahmad4, Sadia Anwar5, Usama Hussain Kamal6
- Assistant Professor, Department of Radiology, Bakhtawar Amin Medical & Dental College, Multan, Pakistan
- Senior Registrar, Department of Radiology, Children Hospital and Institute of Child Health, Multan, Pakistan
- Associate Professor and Head, Department of Radiology, Children Hospital and Institute of Child Health, Multan, Pakistan
- Assistant professor, Department of Surgery, Bakhtarwar Amin Medical and Dental College, Multan, Pakistan
- Professor, Department of Pathology, Gujranwala Medical College, Gujranwala, Pakistan
- First Year Medical Student, Services Institute of Medical Sciences, Lahore, Pakistan
References
- Akhter P, Orfi SD, Ahmad N. Assessment of iodine levels in the Pakistani diet. Nutrition. 2004;20(9):783–7. https://doi.org/10.1016/j.nut.2004.05.019
- Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. https://doi.org/10.1089/thy.2015.0020
- Russ G, Leboulleux S, Leenhardt L, Hegedüs L. Thyroid incidentalomas: epidemiology, risk stratification with ultrasound and workup. Eur Thyroid J. 2014;3(3):154–63. https://doi.org/10.1159/000365289
- Baloch ZW, Cibas ES, Clark DP, Layfield LJ, Ljung BM, Pitman MB, et al. The National Cancer Institute Thyroid fine needle aspiration state of the science conference: a summation. Cyto J. 2008;5:6. https://doi.org/10.1186/1742-6413-5-6
- Bohacek L, Milas M, Mitchell J, Siperstein A, Berber E. Diagnostic accuracy of surgeon-performed ultrasound-guided fine-needle aspiration of thyroid nodules. Ann Surg Oncol. 2012;19(1):45–51. https://doi.org/10.1245/s10434-011-1807-z
- Gregory A, Bayat M, Kumar V, Denis M, Kim BH, Webb J, et al. Differentiation of benign and malignant thyroid nodules by using comb-push ultrasound shear elastography: a preliminary two-plane view study. Acad Radiol. 2018;25(11):1388–97. https://doi.org/10.1016/j.acra.2018.02.025
- Russ G, Royer B, Bigorgne C, Rouxel A, Bienvenu-Perrard M, Leenhardt L. Prospective evaluation of thyroid imaging reporting and data system on 4550 nodules with and without elastography. Eur J Endocrinol. 2013;168(5):649–55. https://doi.org/10.1530/EJE-12-0936
- Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS. The diagnosis and management of thyroid nodules: a review. JAMA. 2018;319(9):914–24. https://doi.org/10.1001/jama.2018.0898
- Stephanie AF. Evaluation of five ultrasound risk-stratification systems for choosing thyroid nodules for fine-needle aspiration. Clin Thyroid. 2019;31(12):520–3. https://doi.org/10.1089/ct.2019;31.520-523
- Zhao W, Han C, Shi X, Xiong C, Sun J, Shan Z, et al. Prevalence of goiter and thyroid nodules before and after implementation of the universal salt iodization program in mainland china from 1985 to 2014: a systematic review and meta-analysis. Plos One. 2014;9(10):e109549. https://doi.org/10.1371/journal.pone.0109549
- Alam T, Khattak YJ, Beg M, Raouf A, Azeemuddin M, Khan AA. Diagnostic accuracy of ultrasonography in differentiating benign and malignant thyroid nodules using fine needle aspiration cytology as the reference standard. Asian Pac J Cancer Prev. 2014;15(22):10039–43. https://doi.org/10.7314/APJCP.2014.15.22.10039
- Trimboli P, Ngu R, Royer B, Giovanella L, Bigorgne C, Simo R, et al. A multicentre validation study for the EU-TIRADS using histological diagnosis as a gold standard. Clin Endocrinol (Oxf). 2019;91(2):340–7. https://doi.org/10.1111/cen.13997
- Macedo BM, Izquierdo RF, Golbert L, Meyer ELS. Reliability of thyroid imaging reporting and data system (TI-RADS), and ultrasonographic classification of the American thyroid association (ATA) in differentiating benign from malignant thyroid nodules. Arch Endocrinol Metab. 2018;62(2):131–8. https://doi.org/10.20945/2359-3997000000018
