Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 40(2):84-89
ORIGINAL ARTICLE
Determining the knowledge of medical students regarding spread and prevention of monkeypox virus - a single institution-based study from Lahore
Syed Tahir Hussain1*, Hina Ahmed2, Rehan Hassan Butt1, Shazil Iman1, Muhammad Ali Hussain1, Muhammad Awais1
Received: 27 March 2024 Revised date: 20 May 2024 Accepted: 25 May 2024
Correspondence to: Syed Tahir Hussain
*Final Year MBBS Student, Central Park Medical College, Lahore, Pakistan.
Email: syedtahirhussainshahthe@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
The world has already seen a massive pandemic of COVID-19. Medical professionals are the first line of defense in this pandemic. In this regard knowing about the spread of Monkeypox and then its preventive measure could save us from another pandemic. This study was therefore designed to determine the knowledge and awareness of medical students regarding the spread and prevention of monkeypox viral disease.
Methods:
It was a cross-sectional study comprising of 406 medical students from first to final year MBBS of a private medical college in Lahore were enrolled through convenient sampling. The data were collected through a structured and validated questionnaire designed through Google Forms and administered by the researchers through WhatsApp groups. The data regarding the mode of spread and prevention was analyzed statistically with a p-value < 0.05 as significant.
Results:
A total of 406 responses were collected. The mean age of the participants was 22 ± 2 SD years. Regarding modes of spread of monkeypox, the medical students had significant knowledge about different routes; 359 (88.4%) respondents were aware of human-to-human transmission through respiratory secretions and vertical transmission (p < 0.001), while 298 (73.4%) respondents also regarded fomites as one of the modes (p < 0.001).
Regarding the prevention of spread, 359 (88.4%) respondents picked each of the options of wearing masks, smallpox vaccination, and prior infection with chickenpox or smallpox while 329 (81%) and 309 (76.1%) respondents regarded the use of antivirals and isolation of affected person respectively as protective against Monkeypox (p < 0.001).
Conclusion:
The knowledge of medical students regarding the spread and prevention of monkeypox seems satisfactory. This can be attributed to the inclusion of the disease in their curriculum and its status as an emerging global outbreak, with extensive information readily available through social media platforms.
Keywords:
Monkeypox virus, spread, prevention, medical students, knowledge, awareness.
Introduction
Human monkeypox virus (MPXV) is a double-stranded DNA virus that belongs to Orthopoxvirus genus.1 It has a presentation similar to smallpox. Clinical differentiation of the disease from smallpox and varicella is difficult.1 The virus is the foremost Orthopoxvirus affecting the human population since smallpox eradication, confirmed by the World Health Organization (WHO) in 1980. It potentially spreads from zoonotic reservoir.2
First ever human cases of MPXV were detected in 1970 in the Democratic Republic of the Congo (DRC).3 In 1970, 11 African states documented human cases of MPXV.1 Unfortunately, Nigeria has been experiencing a major epidemic since 20174, with over 500 suspected cases and over 200 confirmed cases.1 In 2003, the first case of MPXV was reported in the United States of America. Thirty seven new cases of monkeypox have been identified till 19 May, 2022.5 Although no case of monkeypox has been reported yet in Pakistan6, NIH (National Institute of Health) has placed Pakistan on high alert against the virus in light of cases being reported in non-endemic countries.7
The transmission of monkeypox virus mostly occurs through respiratory aerosols. However, indirect or direct contact with live or dead animals is assumed to be the driver of human monkeypox infections in humans.8 Direct contact with the rash of the affected person can also cause the spread of monkeypox virus to other. Intimate contact with the infected person can also cause the spread of infection. The risk of spread of monkeypox virus from inanimate objects is not yet determined. Monkey pox virus can also spread to fetus from the affected mother by vertical transmission.
It has an incubation period of 7-14 days and a prodromal period of 1-4 days.9 The disease is characterized by a short febrile illness with lymphadenopathy followed by a rash first appearing on face then following to the body, hands, legs, and feet.10 The rash undergoes several stages of evolution from macules, papules, vesicles (fluid-filled blisters), and pustules3, followed by resolution over time with crusts and scabs, which drop off on recovery. Recovery occurs in most patients within 2-4 weeks.9
Complications are more likely in children, pregnant women, and the immunocompromised. Specific diagnosis is by detection of viral DNA by Polymerase chain reaction. The most common differential diagnosis is chickenpox.1
The rationale of conducting of this study is to gather information regarding knowledge that student has regarding the modes of spread and preventive strategies related to this emerging disease.
Methods
It was a cross sectional study conducted at the Central Park Medical College (CPMC), Lahore, Pakistan, a private sector medical college recognized by Pakistan Medical and Dental Council. The total duration of the study was 6 months from August to September 2023. A sample size of 384 was calculated by the WHO sample size calculator. Students from first to final year MBBS were included in this research after taking their written informed consent Students who were not willing to participate, those who did not respond within the stipulated time and the ones who were on leave because of any reason including freezing or discontinuation during data collection, were excluded. The study was approved by the Institutional Ethical Review Committee of CPMC. The identities of the students were not revealed hence confidentiality was maintained. Data were collected from a self-designed, customized, and structured questionnaire which was validated after piloting and reviewing by the experts.
The questionnaire comprised of two big parts. The first part is to gather information regarding spread of Monkeypox virus and questions asked in this part are regarding the reservoir of Monkeypox, human-to-human transmission, and vertical transmission, spread through respiratory system and fomites. In the second part questions regarding prevention is asked such as use of antiviral, smallpox vaccine, wearing mask, washing of hand and quarantine. The questionnaire disseminated to the students through WhatsApp groups using online Google Forms. The principal investigator sent reminder messages to all WhatsApp groups of different MBBS classes twice a week. The checking of information given in the Google Form questionnaire is done by principal investigator (PI). Class representatives from each class were appointed as focal person. Queries regarding questionnaire is answered by PI. The data were collected by maintaining the anonymity and confidentiality.
Statistical Analysis
Once the data were collected, the compiled Excel sheet from online Google Forms was transferred to Statistical Package for the Social Sciences software version 26.0 for further analysis. Means and standard deviations were calculated for quantitative variables like age while frequencies of each variable were calculated. Chi square test was applied to determine the relationship between the categorical variables. Data were presented in the form of frequency tables, histograms, bars, and pie charts. The level of significance was set at 95% (p < 0.05) and the power of the study at 80%.
Results
A Google Form questionnaire was distributed to 500 enrolled students in different years of MBBS out of which 406 responses were received. The response rate was 81.2%. The maximum respondents 94 (23%) were from second-year and third-year MBBS each while the least responses 52 (13%) were received from Final year MBBS students. (Figure 1). The mean age of the enrolled students was 22 ± 2 SD years.
A total of 359 (88.4%) medical students agreed that the spread of monkeypox virus occurs through human-to-human transmission, respiratory secretions, and vertical transmission (p < 0.001). However, 298 (73.4%) students agreed that fomites could transmit monkeypox virus to others (p < 0.001).
Furthermore, regarding the prevention of monkeypox, 359 (88.4%) respondents opined wearing masks, vaccination against smallpox, and having a previous infection of chickenpox or smallpox as the effective preventive measures (p < 0.001) while 329 (81%) and 309 (76.1%) respondents regarded use of antivirals and isolation of effected person respectively as one of the modes of prevention (p < 0.001), (Table 1).
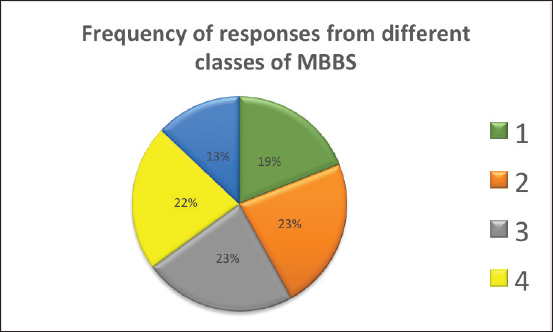
Figure 1. Pie chart showing the reponses from each year of MBBS students.
Table 1. Cross tabulation between knowledge of monkeypox virus and methods of prevention.
| Prevention of monkeypox virus | Category | Knowledge of monkeypox virus | Total n (%) | p-value* | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Antivirals | Yes | 329 (81%) | 0 | 329 (81%) | <0.001 |
| No | 71 (17.5%) | 6 (1.5%) | 77 (19%) | ||
| Small pox vaccine | Yes | 359 (88.4%) | 0 | 359 (88.4%) | <0.001 |
| No | 41 (10%) | 6 (1.6%) | 47 (11.6%) | ||
| Isolation of affected person | Yes | 309 (76.1%) | 0 | 309 (76.1%) | <0.001 |
| No | 91 (22.4%) | 6 (1.6%) | 97 (23.9%) | ||
| Wearing Mask | Yes | 359 (88.4%) | 0 | 359 (88.4%) | <0.001 |
| No | 41 (10%) | 6 (1.6%) | 47 (11.6%) | ||
| Previous infection of chickenpox or smallpox | Yes | 359 (88.4%) | 0 | 359 (88.4%) | <0.001 |
| No | 41 (10%) | 6 (1.6%) | 47 (11.6%) | ||
| Hand washing | Yes | 309 (76.1%) | 0 | 309 (76.1%) | <0.001 |
| No | 91 (22.4%) | 6 (1.6%) | 97 (23.9%) | ||
| Quarantine | Yes | 309 (76.1%) | 0 | 309 (76.1%) | <0.001 |
| No | 91 (22.4%) | 6 (1.6%) | 97 (23.9%) | ||
*Chi square test.
Discussion
The results of the present study depict that 83.7% of participants are well informed about the grave consequences of the human MPXV infection. The respondents were MBBS students from different years of study with maximum representation from second and third-year students. The least number of responses gathered from final year MBBS students could be because of high academic pressure and intense ward rotations of Final year MBBS students due to which they are unable to fill the response form.
The results regarding awareness in the present study are comparable to a cross-sectional survey conducted in Saudi Arabia where physician’s knowledge and attitudes regarding monkeypox infection on multiple-item scales were conducted.11 The results indicated that 55% of the survey respondents had “good knowledge” about human MPXV. On the other hand, a study conducted in Ohio12, United States of America, revealed that medical professionals have limited knowledge. Participant’s perspectives on the eventual containment of MPXV and the threat posed by the virus were mixed. Despite the fact that approximately one quarter of respondents reported prior knowledge of MPXV. Similarly, another study conducted in Indonesia on 432 general practitioners revealed that only 10% had a good understanding regarding the predictors of monkeypox spread and prevention.13 It is because of that the emerging health problems like MPXV is the part of the curriculum of medical students. The improvement of one’s understanding of MPXV can be aided by informative lectures and workshops. Seminars and public awareness campaigns may aid in the education of healthcare professionals. Improving the capacity of general practitioners to respond to human MPXV cases and report them to disease surveillance systems requires a greater understanding of monkeypox. About 82% of respondents in a multinational study felt the need to obtain additional information.14 The results demonstrated that people were more concerned about COVID-19 infection than monkeypox, particularly those who had never been infected with COVID-19. This could be the reason why people are less eager to learn about other diseases. One of the main features of the present study was to highlight the awareness and knowledge among medical students regarding the spread and prevention of MPXV as it will help them to handle it correctly as front line healthcare workers if there is another epidemic or pandemic like COVID-19.
Nevertheless, according to a survey conducted in Bangladesh, the majority of the general population (66.6%) were aware of the MPX disease.15 The factors influencing the level of knowledge about MPXV were educational standing and occupation. Another interesting study conducted in Lebonan16 the overall level of knowledge regarding MPXV was poor among the Lebanese healthcare workers; only 33.04% demonstrated a good level of knowledge.
According to our study, 88.4% of participants were convinced that it spreads through human-to-human transmission, respiratory secretions, and vertical transmission. About 73.4% of participants responded that it spreads through fomites. A study conducted in the United Kingdom found evidence of sustained human-to-human transmission of MPXV through close contact, including sexual networks.17 It denotes the need for sex education to be provided to everyone and public health should be enhanced so that the message can reach everyone. MPXV may spread via respiratory aerosols and contact lesions on the skin.17 This indicates the importance of wearing a mask when the disease is endemic or when a patient infected with MPXV is nearby. MPXV can be transmitted through direct contact with an infected person’s bodily fluids, mucous membranes, broken skin, open sores, or virus-infected material.18 In addition, the virus can be transmitted by droplet transmission through direct and prolonged face-to-face contact between people. The present study also shows improved behavior among the participants regarding the spread of monkeypox virus.
A total of 88.4% participants of in the present study responded that monkeypox can be transmitted through vertical transmission; the literature however reveals that MPXV transmission through the placenta is not quite frequent.19
Our study results showed that 88.4% of students were aware that monkey pox can be prevented by smallpox vaccine and 76.1% of students responded that isolation of the patient is helpful in limiting the spread of monkey pox. A questionnaire-based cross-sectional study was conducted among the community of pharmacists in Saudi Arabia.20 The overall awareness was almost 75% which is comparable to the present study. While another study conducted in Pakistan3 revealed that the majority of study participants lacked adequate knowledge regarding MPXV disease and the efficacy of the smallpox vaccine. The results of our study in terms of the knowledge regarding prevention against monkeypox virus are very promising and shows better awareness in medical students as compared to the study conducted in Saudi Arab20 and Pakistan.3 To prevent the emergence and spread of MPXV in Pakistan, it is necessary to establish and implement a comprehensive strategic framework for public health education. A study conducted in Italy21 demonstrated that the smallpox vaccine is 80.7% effective in preventing human monkey pox and that immunity conferred by a prior smallpox vaccination is durable. Vaccination against smallpox also reduces the risk of human MPXV. Two Congo-based cross-sectional studies involving approximately 1,800 human MPXV cases revealed that the risk of acquiring infection was 2.73 times greater among unvaccinated participants than among vaccinated individuals.24
The present study shows a good knowledge of respondents towards the use of smallpox vaccine for prevention against the monkeypox virus. But framework is required to build the same level of awareness in the general public as well.
Facemasks and facemasks plus hand hygiene may prevent infection in community settings, subject to early use and compliance. Two trials in healthcare workers favored respirators for clinical respiratory illness.22 It shows that respondents of our research have a good knowledge regarding use of face mask for MPXV. It can also be attributed to the safety measures taken during the COVID-19 pandemic.
Role of inactivated antibody-based therapies, including hyper immune globulin, monoclonal antibodies, and convalescent plasma, have been utilized against a variety of infectious diseases.23 Therapies based on inactivated antibodies may play a role in the treatment of MPXV, either as a bridge between vaccines and antivirals or as a supplement to direct acting antivirals. Their effectiveness is contingent upon early administration and the presence of high-titer antibodies against the target pathogen. In addition to vaccination, safer sexual practices can help prevent the spread of MPXV. The Centers for Disease Control and Prevention recommends avoiding sexual contact with a person exhibiting symptoms of MPXV and refraining from activities that increase exposure to MPXV for 2 weeks following the second vaccination dose. Similarly, the medical students in the present study were aware of these facts as about 81% of them were convinced that it could be prevented by the use of different antiviral therapies.
Conclusion
The knowledge and awareness of medical students concerning the transmission and mitigation of monkeypox is deemed satisfactory. This may be due to the fact that monkeypox is included in their curriculum and being an emerging global disease, social media platforms must have also led to this optimal level of knowledge and awareness among these students.
Limitations of the study
The study participants enrolled were from a single private medical college only due to feasibility issues. It is highly recommended to plan a future study with a larger sample size and other institutions for better comparison.
Acknowledgement
The authors would like to acknowledge the support of Community Medicine Department of Central Park Medical College, Lahore, Pakistan for execution of this research project.
List of Abbreviations
| MPXV | Human monkeypox virus |
| PI | Principal investigator |
| PXV | Human monkeypox virus |
| WHO | World Health Organization |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethics approval number and date
The study was approved by the Institutional Review Board of Central Park Medical College Lahore Pakistan vide Letter No CPMC/IRB-No/1417 dated October 17, 2023.
Authors’ contributions
TH, HA: Conception and design of study, acquisition of data, critical intellectual input, drafting of manuscript
RB, MA, SI, MA: Acquisition of data, drafting of manuscript.
ALL AUTHORS: Approval of the final version of the manuscript to be published
Authors’ details
Syed Tahir Hussain1, Hina Ahmed2, Rehan Hassan Butt1, Shazil Iman1, Muhammad Ali Hussain1, Muhammad Awais1
- Final year MBBS student, Central Park Medical College, Lahore, Pakistan
- Associate Professor, Department of Community Medicine, Central Park Medical College, Lahore, Pakistan
References
- Singhal T, Kabra SK, Lodha R. Monkeypox: a review. Indian J. Pediatr. 2022;89(10):955–60. https://doi.org/10.1007/s12098-022-04348-0
- Mitjà O, Ogoina D, Titanji BK, Galvan C, Muyembe JJ, Marks M, et al. Monkeypox. Lancet. 2023;7:401(10370):60–74. https://doi.org/10.1016/s0140-6736(22)02075-x
- Martín-Delgado MC, Sánchez FJ, Martínez-Sellés M, García JM, Guillén SM, Rodríguez-Artalejo F, et al. Monkeypox in humans: a new outbreak. Revista de la SEQ. 2022;35(6):509–15. https://doi.org/10.37201/req/059.2022
- Beer EM, Rao VB. A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLoS Negl Trop Dis. 2019;13(10):e0007791. https://doi.org/10.1371/journal.pntd.0007791
- Kumar N, Acharya A, Gendelman HE, Byrareddy SN. The 2022 outbreak and the pathobiology of the monkeypox virus. J Autoimmun. 2022;131:102855. https://doi.org/10.1016/j.jaut.2022.102855
- No monkeypox case detected in Pakistan yet, clarifies NIH - Pakistan - DAWN. 2022 May 24. [cited 2024 Jan 11]. Available from: https://www.dawn.com/news/1691293
- Najeeb H, Huda Z. Monkeypox virus: a spreading threat for Pakistan?. Ann Med Surg. 2022;79:103977–79. https://doi.org/10.1016/j.amsu.2022.103977
- Lum FM, Torres-Ruesta A, Tay MZ, Lin RT, Lye DC, Rénia L, et al. Monkeypox: disease epidemiology, host immunity and clinical interventions. Nat Rev Immunol. 2022;22(10):597–613. https://doi.org/10.1038/s41577-022-00775-4
- Huang Y, Mu L, Wang W. Monkeypox: epidemiology, pathogenesis, treatment and prevention. Signal Transduct Target Ther. 2022;7(1):373–94. https://doi.org/10.1038/s41392-022-01215-4
- Kmiec D, Kirchhoff F. Monkeypox: a new threat?. Int J Mol Sci. 2022;23(14):7866–79. https://doi.org/10.3390/ijms23147866
- Alshahrani NZ, Algethami MR, Alarifi AM, Alzahrani F, Alshehri EA, Alshehri AM, et al. Knowledge and attitude regarding monkeypox virus among physicians in Saudi Arabia: a cross-sectional study. Vaccines. 2022;10(12):2099–111. https://doi.org/10.3390/vaccines10122099
- Bates BR, Grijalva MJ. Knowledge, attitudes, and practices towards monkeypox during the 2022 outbreak: an online cross-sectional survey among clinicians in Ohio, USA. J Infect Public Health. 2022;15(12):1459–65. https://doi.org/10.1016/j.jiph.2022.11.004
- Harapan H, Setiawan AM, Yufika A, Anwar S, Wahyuni S, Asrizal FW, et al. Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog Glob Health. 2020;114(2):68–75. https://doi.org/10.1080/20477724.2020.1743037
- Swed S, Alibrahim H, Bohsas H, Jawish N, Rais MA, Nasif MN, et al. A multinational cross-sectional study on the awareness and concerns of healthcare providers toward monkeypox and the promotion of the monkeypox vaccination. Public Health Front. 2023;11:1153136. https://doi.org/10.3389/fpubh.2023.1153136
- Nath SD, Islam AK, Majumder K, Rimti FH, Das J, Tabassum MN, et al. Assessment of knowledge on human monkeypox virus among general population in Bangladesh: a nationwide cross-sectional study. MedRxiv. 2022:2022-08. https://doi.org/10.1101/2022.08.31.22279445
- Malaeb D, Sallam M, Salim NA, Dabbous M, Younes S, Nasrallah Y, et al. Knowledge, attitude and conspiracy beliefs of healthcare workers in Lebanon towards monkeypox. Trop Med Infect. 2023 23;8(2):81–8. https://doi.org/10.3390/tropicalmed8020081
- Vivancos R, Anderson C, Blomquist P, Balasegaram S, Bell A, Bishop L, et al. Community transmission of monkeypox in the United Kingdom, April to May 2022. Eurosurveillance. 2022;27(22):2200422. https://doi.org/10.2807/1560-7917.ES.2022.27.22.2200422
- Ugwu SE, Abolade SA, Ofeh AS, Awoyinka TB, Okolo BO, Ayeni ET, et al. Knowledge, attitude, and perception of monkeypox among medical/health students across media space in Nigeria. Int J Community Med Public Health. 2022;9(12):4391. https://doi.org/10.18203/2394-6040.ijcmph20223197
- Lai CC, Hsu CK, Yen MY, Lee PI, Ko WC, Hsueh PR. Monkeypox: an emerging global threat during the COVID-19 pandemic. J Microbiol Immunol Infect. 2022;55(5):787–94. https://doi.org/10.1016/j.jmii.2022.07.004
- Alrasheedy AA, Aldawsari AH, Alqasir MI, Alsawyan OA, Alalwan OA, Alwaker SA, et al. Knowledge of community pharmacists in saudi arabia regarding human monkeypox, its management, prevention, and vaccination: findings and implications. Vaccines. 2023;11(4):878–88. https://doi.org/10.3390/vaccines11040878
- Scarinci S, Padovan M, Cosci B, Petillo A, Gattini V, Cosentino F, et al. Evaluation of smallpox vaccination coverage and attitude towards monkeypox vaccination among healthcare workers in an Italian University Hospital. Vaccines. 2023;11(12):1741–50. https://doi.org/10.3390/vaccines11121741
- Maclntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h964–71. https://doi.org/10.1136/bmj.h694
- Bloch EM, Sullivan DJ, Shoham S, Tobian AA, Casadevall A, Gebo KA. The potential role of passive antibody-based therapies as treatments for monkeypox. Public Health. 2022;13(6):e02862–22. https://doi.org/10.1128/mbio.02862-22
- Akter F, Hasan TB, Alam F, Das A, Afrin S, Maisha S, et al. Effect of prior immunization with smallpox vaccine for protection against human Mpox: a systematic review. Rev Med Virol. 2023;33(4):e2444. https://doi.org/10.1002/rmv.2444
Keywords: Monkeypox virus, spread, prevention, medical students, knowledge, awareness.
Publication History
Received: March 27, 2024
Revised: May 20, 2024
Accepted: May 25, 2024
Published: June 25, 2024
Authors
Rehan Hassan Butt
Central Park Medical College
Shazil Iman
Central Park Medical College
Muhammad Ali Hussain
Central Park Medical College
Muhammad Awais
Central Park Medical College
