Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 37(2):123-129
CASE REPORT
Preoperative transcatheter arterial chemoembolization and laparoscopic associating liver partition and portal vein ligation for staged hepatectomy to treat unresectable hepatocellular carcinoma - a case report with review of literature
Yilin Hu, Yanbing Shen, Dan Wang, Tingjia Cao*
Received: 12 January 2021 Revised date: 22 April 2021 Accepted: 10 June 2021
Correspondence to: MD. Tingjia Cao
*Department of General Surgery, Wuhan General Hospital Of Chinese People’s Liberation Army, Wuhan, China
Email: caotingjia_1@sina.com
Full list of author information is available at the end of the article.
ABSTRACT
Transcatheter arterial chemoembolization (TACE) is considered as a major method to treat hepatocellular carcinoma (HCC). Associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) has been used to treat patients with advanced HCC. This case report documents the safety, efficacy, and feasibility of TACE and laparoscopic ALPPS to treat the unresectable HCC of the right liver with right intra-hepatic metastasis in a male patient. Percutaneous and trans-femoral artery TACE was performed preoperatively, and the ALPPS stage-I at the 4th week and stage-II after 14 days was carried out. Postoperative outcome was assessed after 180 days of follow-up. It is concluded that preoperative TACE and laparoscopic ALPPS offer a fine treatment alternative to the patients with insufficient residual liver volume and relatively-advanced and extensive HCC.
Keywords:
Transcatheter arterial chemoembolization (TACE), Associated liver partition and portal vein ligation for staged hepatectomy (ALPPS), Hepatocellular carcinoma, Advanced stage.
Introduction
Hepatectomy and transcatheter arterial chemoembolization (TACE) are still two major methods to treat hepatocellular carcinoma (HCC). TACE is a good method to assess the lesion size, control the further development of lesion and even to decrease the size pre-operatively. Hepatectomy, on the other hand, is a key method to treat the HCC. It not only successfully operates the R0 liver but also can ensure some adequate amount of future liver remnant (FLR) which is the premise to get the good curative effect. China has a large prevalence of HCC (up to 80%) complicated with Hepatitis B. Many advance staged patients cannot undergo radical operation because of the limited FLR [1]. Associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) is considered as a good method of choice for relatively advanced HCC patients with limited FLR and compromised tolerance to the massive hepatectomy. Traditional ALPPS adopts the open abdominal surgery which is one of the most innovative and advanced hepatobiliary technologies in the recent years [2]. The short-term therapeutic outcomes of laparoscopic hepatectomy such as intraoperative bleeding, rate of blood transfusion, operating time, and postoperative complications outweigh the open abdominal hepatectomy technique. However, the long-term tumor free survival has no statistical difference [3]. Therefore, laparoscopic ALPPS is considered as a safe and a minimally invasive technique. In the following case report, TACE was performed on one patient with extensive HCC of right liver followed by laparoscopic-ALPPS achieving a better curative effect.
Report of a Case
A male patient, 49 years old, was admitted to the Department of General Surgery, Wuhan General Hospital of Chinese People’s Liberation Army, Wuhan on August 16, 2019, with suspicion of liver carcinoma. There was no jaundice on skin or sclera. Superficial lymph nodes were not palpable. There was no abnormality noted during the cardiopulmonary examination. The patient presented with flat abdomen and abdominal wall was soft without tenderness or rebound tenderness. There was no palpable mass in the abdomen. The liver and spleen were impalpable. Murphy’s sign and shifting dullness was negative. The intestinal bowel sounds were normal. The laboratory tests showed Hepatitis B surface antigen (HBsAg), anti-HBe, and anti-HBc positive. The hepatitis B virus (HBV)-DNA was 9.79 × 103 IU/ml. The blood routine, liver, and kidney function, alpha fetoprotein (AFP), Carcinoembryonic antigen, and CA-199 were normal (Table 1). The magnetic resonance imaging (MRI) studies suggested massive primary carcinoma of the right liver with right intra-hepatic metastasis (Figure 1a,b). The standard liver volume was 1,089 ml (Standard liver volume = 706.2 × BSA + 2.4, BSA = 0.00607H + 0.0127W − 0.0698).
For TACE, puncture and catheterization were done via right femoral artery under local anesthesia. Contrast catheter was introduced into celiac artery and mesenteric artery. Opening of proper hepatic artery was narrowed, mesenteric artery was branched to supply blood for liver. Right hepatic artery was tortuous and thickened. In parenchymal phase, there was one massive tumor-stained lesion in the right liver with nodular tumor-stained lesions in the surrounding areas (Figure 1c). Microtubule was introduced into the targeted vessels. Ultra-liquefied lipiodol (10 ml), lobaplatin (50 mg), embolic microspheres, and gelatin sponge particles were introduced to attain optimal embolism for radiography where the tumor stain disappeared (Figure 1d).
This patient was admitted to the hospital again on September 19 for undergoing the enhanced computerized tomography (CT) examination of liver (Figure 2a,b). Baseline investigations like routine blood count, liver function tests, coagulation function tests, AFP, and Hepatitis B virus DNA (HBV-DNA) (Table 1) were carried out. Liver volume was measured (Table 1).
Under general anesthesia, laparoscopic liver parenchymal segmentation and right portal vein ligation and cholecystectomy were carried out, namely, the ALPPS stage-I. Dorsal elevated position was adopted with five laparoscopic small incisions on the upper abdomen (Figure 2c). Laparoscopy revealed no ascitic fluid in the abdominal cavity and no metastatic nodule in the abdominal and pelvic cavities was observed. No significant abnormality was seen in the gallbladder, extrahepatic bile duct, or gastrointestinal tract. The liver showed nodular cirrhosis, and the liver was adhered to the diaphragm (Figure 2b). There was no mass in the left lobe which had a limited volume, accounting for 25% of the whole liver volume. Ultrasound knife was used to separate the adhesion. After gallbladder was successfully excised, the right branch of the portal vein was anatomized from the Glisson sheath which was close to the first hepatic hilum (Figure 3). Silk thread was used to ligate, as well as ligature clamp was used to block. The ultrasound knife and electrosurgical unit were applied to separate the liver tissue of left and right lobe along the left and right ischemia line (Figure 3b). Hemostasis was ensured. Proline line was used to close the wound and liver vein, abdominal cavity was rinsed, and there was no active bleeding. No biliary fistula in the liver wound surface was seen (Figure 3c). One drainage tube was placed on the wound surface. Amount of intraoperative bleeding was about 100 ml. Drainage tube was taken away at the 6th day (Figure 3d).
At the 12th day after the stage-I associating liver partition and portal vein ligation for staged hepatectomy (ALPSS), the enhanced CT examination was carried out (Figure 4a,b) and the liver volume was measured (Table 1). Results suggested that the right hemi-liver could be excised safely.
At the 14th day, the ALPPS stage-II was performed. Under general anesthesia, the right hemi-hepatectomy was carried out. Horizontal position was adopted, J-type incision on the middle of the abdomen was made with a length of 25 cm. After layered cutting and reaching the abdominal cavity, there was a little ascitic fluid in the abdominal cavity. The left liver lobe was significantly enlarged and thickened with a rosy color. There was no enlargement of lymph nodes in the posterior area of hepatoduodenal ligament and at the level of pancreatic head. No obvious lesion was noted in the stomach, pancreas, spleen, pelvis, and other visceras. The right hemi-liver was cut in accordance with the anterior approach. The right hepatic duct, right hepatic artery, right portal vein, and tube of the right caudate lobe were separated and ligated, respectively. The peritoneum between caudate lobe and inferior vena cava was opened. Right sided short veins were separated and ligated. The avascular area of the inferior vena cava was exposed. The remaining liver parenchyma ahead of the inferior vena cava was separated along this space towards the second hepatic hilum. Common hepatic vein and right hepatic vein were separated and the right hepatic vein was dissected (Figure 4c). Finally, the perihepatic ligament was mobilized and the right hemi-liver was completely excised. The abdominal cavity was rinsed. When no blood and bile leakage were ensured, one drainage tube was placed on the wound surface and the sample was taken (Figure 4d). Amount of intraoperative bleeding was about 150 ml.
Table 1. Laboratory indices before operation.
| Before TACE | Before ALPPS-I stage | Before ALPPS-II stage | |
|---|---|---|---|
| TB (μmol/l) | 12.8 | 8.7 | 13.5 |
| DB (μmol/l) | 3.7 | 2.3 | 5.6 |
| ALT (U/l) | 50 | 43 | 62 |
| AST (U/l) | 56 | 40 | 58 |
| Albumin (g/l) | 36.1 | 34.4 | 37.5 |
| PT (s) | 12.4 | 11.8 | 13.0 |
| APTT (s) | 32.4 | 33.5 | 35.0 |
| HBV-DNA (IU/ml) | 9.79 × 103 | 4.67 × 102 | 2.92 × 102 |
| AFP (μg/l) | 7.9 | 7.1 | 6.8 |
| FLR (ml) | 290 | 290 | 480 |
| FLR/standard liver volume (%) | 26.6 | 26.6 | 44.1 |
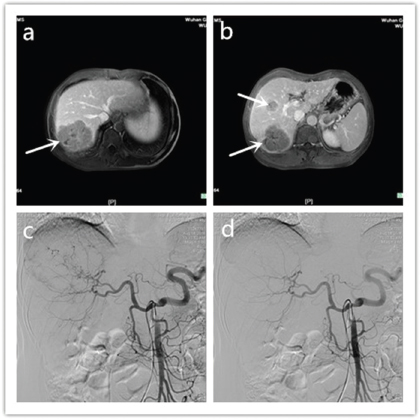
Figure 1. Admission MRI and TACE. (a) Admission MRI-Liver tumor in VI, VII stage, (b) Admission MRI- Liver tumor in VI, VII stage complicated with metastatic lesion in V stage, (c) TACE suggesting tumor stain, (d) TACE embolism completed and tumor stain disappeared.
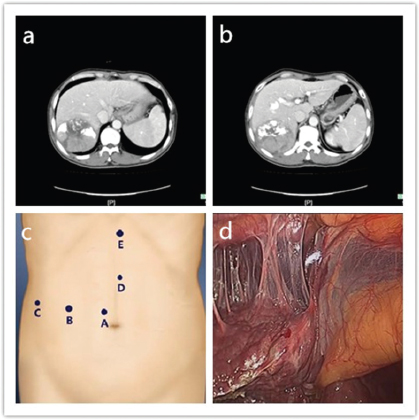
Figure 2. Liver CT and Trocar distribution. (a) Liver CT before laparoscopic-assisted ALPPS I stage: lipiodol deposition after tumor embolism in liver VI, VII stage, (b) Liver CT before laparoscopic-assisted ALPPS I stage: lipiodol deposition after tumor embolism in liver VI, VII stage complicated with metastatic lesion in V stage, (c) Trocar distribution during laparoscopic ALPPS I stage, (d) Nodule cirrhosis and adhesion between liver and diaphragm in laparoscopic ALPPS I stage.
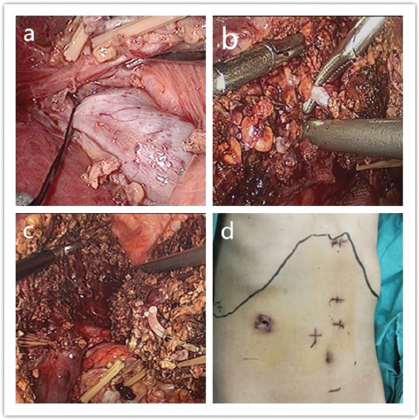
Figure 3. (a) Right portal vein anatomized from Glisson sheath in laparoscopic ALPPS stage-I. (b) Left and right lobe separated in laparoscopic ALPPS stage-I. (c) Laparoscopic ALPPS stage-I operation completed. (d) Drainage tube taken away and abdominal incision of laparoscopic ALPPS stage-I at the 6th day is seen.
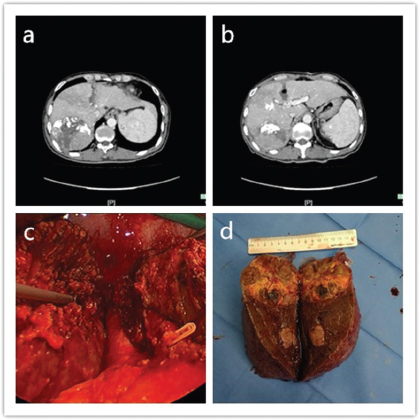
Figure 4. (a) Liver CT before ALPPS stage-II: tumor in liver VI, VII stage; left and right cutting line; obvious hyperplasia on the left liver. (b) Liver CT before ALPPS stage-II: tumor in liver VI, VII complicated with V metastatic lesion; left and right cutting line; obvious hyperplasia on the left liver. (c) During ALPPS stage-II: anterior approach along inferior vena cava to resect right hemi-liver. (d) Post-operative sample.
Patient was followed-up after 180 days. No tumor metastasis or relapse was noted and patient improved satisfactorily (Figure 5a,b).
After TACE, the blood routine, liver function, and coagulation function were normal. After 5 days, the patient was discharged without any discomfort. Entecavir was orally administered 0.5 mg 1/day for 2 weeks. Operating time of the ALPPS stage-I was 150 minutes and amount of intraoperative bleeding was 100 ml. At the 2nd day of the operation, activities and diet of the patient were improved. There was no fever, with body temperature of 36.2°C~37.0°C. Drainage fluid from the liver section at the 1st day was 300 ml, at the 2nd day it was 150 ml, and ranged from 50 to 100 ml later on. The drainage tube was taken away at the 6th day. There was no biliary fistula after operation and no hemorrhage in the abdominal cavity was observed. Postoperative total bilirubin (TB) was 13.8-19.8 μmol/l; peak value of Alanine aminotransferase (ALT) and Aspartate aminotransferase (AST) appeared at the 1st day after operation, and gradually decreased (Table 2). After operation, symptomatic supportive treatment such as routine antibiotics, liver protection and anti-virus were given. At the 12th day after operation, the FLR was 480 ml and the FLR/standard liver volume was 44.1% (Table 1). Liver function came to baseline. No signs of infection were noted in the abdominal cavity. The dietary intake was optimal. All parameters reached the appropriate range to resect the liver safely.
In open abdominal ALPPS stage-II, operating time was approx. 130 minutes and amount of intraoperative bleeding was 150 ml. At the 3rd day after operation, activities and dietary intake were initiated. Body temperature was 36.5°C~37.7°C, heart rate was 70~95/minutes and blood pressure was normal. TB reached the highest level of 39.4 μmol/l at the 5th day after operation, and the highest level of prothrombin time (PT) was 24.1 seconds (Table 3). Daily drainage fluid was 100~300 ml. The tube was taken away at the 5th day. There was no biliary fistula and no abdominal hemorrhage. Postoperative biopsy from the liver revealed poorly differentiated HCC with metastasis in the adjacent nodes.
Discussion
For the extensive and multicentric HCC, TACE is an effective and a minimally-invasive curative method however it still remains debatable in the literature [4]. Some reports point out that the preoperative TACE worsens the prognosis of patient undergoing hepatectomy [5,6]. However, Nishikawa et al. [7] reported in the latest randomized control trail that preoperative TACE is a safe and reliable method with synergistic effects in the postoperative outcome. While another study showed that in patients with portal vein tumor thrombus, TACE can significantly increase the survival benefit [8]. Among the existing literature, only Romic et al. [9] reports one case undergoing preoperative TACE and ALPPS. However, to the author’s knowledge, there is no report about laparoscopic ALPPS. The main reason may be the fear of TACE aggravating the adhesion between liver and surrounding tissue, leading to a difficult and precarious surgery. TACE can lead to tumor necrosis, and at the same time, it may bring in the necrosis of normal liver tissue. According to our experience, adhesion caused by TACE is a treatable entity for an experienced laparoscopic surgeon. Necrosis of normal liver tissue caused by TACE does not influence the increase of FLR. In our case, the increasing rate of FLR was 62.25%. We believe that the TACE augments ALPPS: TACE can also help to scan whether there is a micro-metastatic lesion so as to avoid metastatic lesion on the FLR that subsequently leads to failure to ALPPS. Simultaneously, TACE can control the further growth of the lesion, thus impeding tumor enlargement and/or failure of ALPPS.
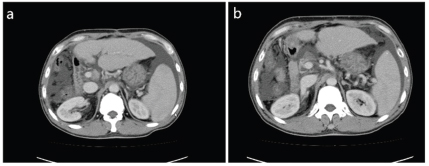
Figure 5. (a,b) Follow-up after 6 months with no relapse of tumor.
Table 2. Laboratory indices after laparoscopic ALPPS stage-I.
| TB (μmol/l) | DB (μmol/l) | ALT (U/l) | AST (U/l) | Albumin (g/l) | PT (s) | APTT (s) | |
|---|---|---|---|---|---|---|---|
| 1st day after operation | 19.6 | 7.8 | 193 | 233 | 27.5 | 14.0 | 36.0 |
| 3rd day after operation | 16.4 | 8.4 | 186 | 89 | 31 | 15.0 | 28.8 |
| 5th day after operation | 19.8 | 9.8 | 64 | 31 | 37.2 | 12.0 | 30.0 |
| 8th day after operation | 13.8 | 5.6 | 62 | 58 | 37.5 | 13.0 | 35.0 |
Table 3. Laboratory indices after laparoscopic ALPPS stage-II.
| TB (μmol/l) | DB (μmol/l) | ALT (U/l) | AST (U/l) | Albumin (g/l) | PT (s) | APTT(s) | |
|---|---|---|---|---|---|---|---|
| 1st day after operation | 19.2 | 10.0 | 41 | 48 | 21.0 | 19.4 | 30.0 |
| 3rd day after operation | 21.4 | 13.2 | 31 | 57 | 26.4 | 24.1 | 34.6 |
| 5th day after operation | 39.4 | 23.6 | 26 | 38 | 33.9 | 22.3 | 38.1 |
Cirrhosis is an adverse factor that restricts the liver regeneration after resection. For the patient with cirrhosis and HCC to undergo the resection, remaining 40% FLR is necessary [10] which prevents choosing hepatectomy for patients with advanced liver carcinoma [11]. In 2012, Schnitzbauer et al. [12] reported staged operation of ALPPS that aroused a widespread concern and was regarded as the revolutionary operative strategy and an innovative breakthrough in the hepatobiliary surgical techniques. Currently, most reports are referring the open abdominal ALPPS with major issue faced by the surgeons being impairment of the patient to undergo two operations in a short-time. During the stage-I, there may occur the inflammatory reaction, biliary leakage and postoperative adhesions that eventually will lead to the difficulty and higher adverse risks for the stage-II operation. Therefore every effort should be made to effectively minimize the complications in stage-I and reach an appropriate FLR. We believe that the full laparoscopy or laparoscopic ALPPS can reduce the biliary leakage, adhesion, infection and liver failure, accelerating the recovery after stage-II, shorten the operative interval and benefit to patients with moderate-and-advanced stage HCC. During the stage-I, we dissected the left and right liver parenchyma via anterior approach, which can separate the tumor for a successful resection thus leaving minimal to mild inflammation and adhesion after stage-I surgery. This is in contrast to the traditional open abdominal surgery where adhesions of portal vein with the liver, between the liver section and abdominal wall, and adhesion among liver section, anterior wall of inferior vena cava and root of hepatic veins are quite common. For the stage-II operation, the anterior approach was again adopted to resect the right hemi-liver to avoid adhesions and extrusion of right liver.
Currently, the ALPPS has become more popular and the surgeons are developing more confidence into the laparoscopic ALPPS. Preoperative TACE and laparoscopic ALPPS may be adopted as a routine procedure to treat patients with advanced stage HCC achieving a good curative effect. After 180 days of post-op follow-up, there was no tumor metastasis that may add a useful information to the existing literature. We believe that preoperative TACE and laparoscopic ALPPS is a safe and effective method but in an experienced surgical hand thus providing a better alternative to the patients with limited FLR and extensive-and-advanced HCC.
Conclusion
Preoperative TACE and laparoscopic ALPPS offer an effective surgical alternative to the patients with insufficient residual liver volume and relatively-advanced HCC.
Limitations of the Case Report
The case report has certain limitations; first, the experience shared is of one patient only. This case report lacks generalizability and does not establish cause-effect relationship. The follow-up period was relatively short. To get a better insight into the safety and efficacy of TACE and ALPPS, more large-scale and prospective randomized studies need to be carried out.
Author’s contributions
YLH: Conception and design of study, acquisition of data, and drafting of manuscript.
YBS, DW, TJC: Acquisition and analysis of data; critical input in the manuscript for important intellectual content.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Acknowledgement
The authors wish to acknowledge the staff of the Department of General Surgery, Wuhan General Hospital of Chinese People's Liberation Army, Wuhan, China for their support during the conduct of study.
Conflict of interest
None to declare.
Grant support & financial disclosure
None to disclose
Ethical approval
All procedures performed in studies involving human participants were approved by the Institutional Ethical Committee of Wuhan General Hospital of Chinese People's Liberation Army, Wuhan, China (Approval number: 201703X /10-2019).
Author details
Yilin Hu1, Yanbing Shen1, Dan Wang1, Tingjia Cao1
- Department of General Surgery, Wuhan General Hospital Of Chinese People’s Liberation Army, Wuhan, China
References
- Guglielmi A, Ruzzenente R, Conci S, Valdegamberi A, Vitali M, Bertuzzo F, et al. Hepatocellular carcinoma: surgical perspectives beyond the barcelona clinic liver cancer recommendations. World J Gastroenterol. 2014;20(24):7525–33. https://doi.org/10.3748/wjg.v20.i24.7525.
- De SE, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg. 2012;255(3):415–7. https://doi.org/10.1097/SLA.0b013e318248577d.
- Dagher I, Di GG, Dubrez J, Lainas P, Smadja C, Franco D. Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg. 2009;198(2):173–7. https://doi.org/10.1016/j.amjsurg.2008.09.015.
- Rahbari NN, Mehrabi A, Mollberg NM, Müller SA, Koch M, Büchler MW, et al. Hepatocellular carcinoma: current management and perspectives for the future. Ann Surg. 2011;253(3):453–69. https://doi.org/10.1097/SLA.0b013e31820d944f.
- Kaibori M, Tanigawa N, Kariya S, Ikeda H, Nakahashi Y, Hirohara J, et al. A prospective randomized controlled trial of preoperative whole-Liver chemolipiodolization for hepatocellular carcinoma. Dig Dis Sci. 2012;57(5):1404. https://doi.org/10.1007/s10620-012-2029-3.
- Toro A, Pulvirenti E, Palermo F, Di CI. Health-related quality of life in patients with hepatocellular carcinoma after hepatic resection, transcatheter arterial chemoembolization, radiofrequency ablation or no treatment. Surg Oncol. 2012;21(1):23–30. https://doi.org/10.1016/j.suronc.2011.10.005.
- Nishikawa H, Arimoto A, Wakasa T, Kita R, Kimura T, Osaki Y. Effect of transcatheter arterial chemoembolization prior to surgical resection for hepatocellular carcinoma. Int J Oncol. 2013;42(1):151–60. https://doi.org/10.3892/ijo.2012.1711.
- Zhang YF, Guo RP, Zou RH, Shen JX, Wei W, Li SH, et al. Efficacy and safety of preoperative chemoembolization for resectable hepatocellular carcinoma with portal vein invasion: a prospective comparative study. Eur Radiol. 2016;26(7):2078–88. https://doi.org/10.1007/s00330-015-4021-8.
- Romic B, Romic I, Mance M, Pavlek G, Skegro M. Successful associating liver partition and portal vein ligation after unsuccessful double TACE procedure complicated with sepsis and pancreatitis. Klin Onkol. 2016;29(1):59; https://doi.org/10.14735/amko201659.
- Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D. Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol. 2006;13(10):1271. https://doi.org/10.1245/s10434-006-9045-5.
- Bruix J, Gores GJ, Mazzaferro V. Hepatocellular carcinoma: clinical frontiers and perspectives. Gut. 2014;63(5):844–55. https://doi.org/10.1136/gutjnl-2013-306627.
- Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255(3):405–14. https://doi.org/10.1097/SLA.0b013e31824856f5.
Keywords: Transcatheter arterial chemoembolization, Associated liver partition and portal vein ligation for staged hepatectomy, Hepatocellular carcinoma.
Publication History
Received: January 12, 2021
Revised: April 22, 2021
Accepted: June 10, 2021
Published: June 30, 2021
Authors
Yilin Hu
Department of General Surgery, Wuhan General Hospital of Chinese People’s Liberation Army, Wuhan - China.
Yanbing Shen
Department of General Surgery, Wuhan General Hospital of Chinese People’s Liberation Army, Wuhan - China.
Dan Wang
Department of General Surgery, Wuhan General Hospital of Chinese People’s Liberation Army, Wuhan - China.
Tingjia Cao
Department of General Surgery, Wuhan General Hospital of Chinese People’s Liberation Army, Wuhan - China.
