Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 38(2):53-56
CURRENT UPDATE
The truth of monkeypox outbreak: a guide for the diagnostic laboratories, health care workers and community in Pakistan
Mulazim Hussain Bukhari
Received: 25 May 2022 Revised date: 07 June 2022 Accepted: 10 June 2022
Correspondence to: Mulazim Hussain Bukhari
*Professor of Pathology & Principal, Azad Jammu Kashmir Medical College, Muzaffarabad, Pakistan.
Email: mulazim.hussain@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Surviving the lethal coronavirus pandemic just recently, the world is now facing another challenge to prevent getting infected with the monkeypox virus. Antiviral vaccines and treatments are being explored for possible protection and treatment. The health workers and paramedics are the front-line fighters who are facing high risk of acquisition. Safe human practices, like COVID-19 pandemic, are at the core of preparedness and response to curb the spread of this distressing disease.
Keywords:
Monkeypox, Orthopoxvirus, Pakistan, smallpox, vaccine.
No case of Monkeypox (MP) has been reported in Pakistan yet, but the World Health Organization (WHO) and the Federal government of Pakistan have issued special instructions to all national and provincial health authorities to remain on high alert for any suspected case of MP.1,2 Pakistan is a developing country with a population of more than 220 million people, with low hygienic facilities and insufficient awareness about the current outbreak of MP disease. The first case of this disease was reported on May 6, 2022, in UK in a male who came from Nigeria and till May 28, there were 33 cases and interestingly all were males and homosexual. According to WHO till May 28, 2022, the MP virus was transmitted to more than 21 countries with about 300 confirmed cases and over 100 suspected cases in no endemic nations; where it is typically not found.3
What is MP and the pathogen of MP
MP is a rare disease, caused by the MP, an enveloped double-stranded DNA virus which belongs to the Orthopoxvirus genus of the Poxviridae family. It includes the variola (smallpox) virus as well as the vaccinia virus, which is used in the smallpox vaccine. This disease was reported in Monkeys in 1958 in Danish Laboratory and first time in humans in 1970 in Congo, Democratic Republic of Africa.1
There are two distinct genetic clades of the MP virus:
- The Central African (Congo Basin) clade.
- The West African clade.
The West African Congo Basin clade has historically caused more severe disease with >10% mortality and was thought to be more transmissible; Cameroon is the only African country where both clades of the virus have been found.
It is a zoonotic disease but still, the primary source of the MP remained mysterious and uncertainty remains on the natural history of the MP virus. The various animal species have been identified as susceptible to MP virus like squirrels, rats, monkeys, etc. How MP virus circulation is maintained in nature, it is still an uncovered mystery.1,4
MP virus transmission from animals
The transmission can be from direct contact with the skin, mucosal surface, blood, bodily fluids, of infected animals. The disease can be transmitted by eating inadequately cooked meat and other animal products of infected animals. It has been observed that the population living in or near the forested areas may have indirect or low-level exposure to infected animals.1,4
MP virus transmission from humans to humans
This may be due to direct physical contact with an infected person, sexual interaction (homosexual), etc. While close physical contact is a well-known risk factor for transmission of MP virus, like coronavirus, it can spread through droplet infection, sharing of saliva, and nasal or respiratory secretions (Figure 1). The virus particles can remain viable on surfaces, clothing, and bedding for up to 1 week, therefore using or sharing of the patient’s clothing or other stuff can cause MP virus transmission. However, the longest documented chain of transmission in a community has risen in recent years from 6 to 9 successive person-to-person infections. They remained contagious until their last MP scab fell off. The MP virus can spread through the air in enclosed settings, such as a building (airborne route). Transmission can also occur via the placenta from mother to fetus (which can lead to congenital MP) or during close contact during and after birth. But transmission through milk has not been reported yet.1-4
Signs and symptoms
The incubation period of the MP virus is usually from 5 to 21 days but the danger is considered for 4 weeks. The infection can be divided into two phases: the invasion phase (lasts between 1 and 5 days) characterized by fever, intense headache, lymphadenopathy (swelling of the lymph nodes), back pain, myalgia (muscle aches), and intense asthenia (lack of energy). Enlargement of the neck lymph nodes is a distinctive feature of MP compared to other diseases that may initially appear similar (chickenpox, measles, and smallpox). During the second phase, skin eruptions usually begin within 1-3 days of the appearance of fever. The rash tends to be more concentrated on the face and extremities rather than on the trunk.2-3
The rash evolves sequentially from macules (lesions with a flat base) to papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts that dry up and fall off. The number of lesions varies from a few to several thousand. In severe cases, lesions can coalesce until large sections of skin slough off.1,3
Complications of the MP virus
It is a self-limited disease with the symptoms lasting from 2 to 4 weeks, but the severe cases occur more commonly among children and are related to the extent of virus exposure, patient health status and nature of complications. Underlying immune deficiencies may lead to worse outcomes. Complications of MP can include secondary infections, bronchopneumonia, sepsis, encephalitis, and infection of the cornea with ensuing loss of vision. Although vaccination against smallpox was protective in the past, today persons younger than 40 to 50 years of age (depending on the country) may be more susceptible to MP due to cessation of smallpox vaccination campaigns globally after eradication of the disease. 2-3
How to diagnose the MP disease?
The diagnosis is bases on clinical presentation of the patient and if the MP is suspected, health workers should collect an appropriate sample and have it transported safely to a laboratory with appropriate capability for testing.2
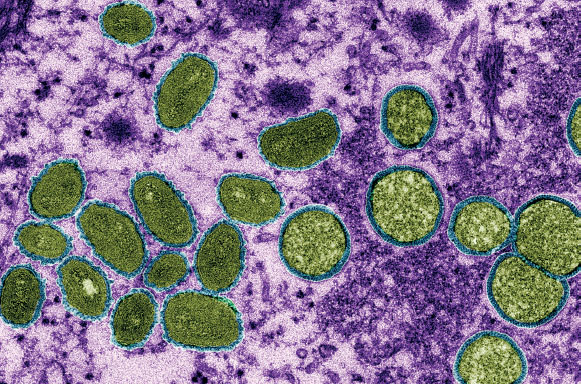
Figure 1. The MP virus shown here in a colored electron micrograph typically spreads by skin-to-skin contact or respiratory droplets. Sexual transmission (homosexual) may play a role in the new outbreak. Adopted from CDC/CYNTHIA S. GOLDSMITH/SCIENCE SOURCE.5
- Confirmation of MP depends on the type of specimen, quality of specimen, and laboratory test performed.
- The specimens should be packed and shipped in accordance with national and international chain of custody requirements.
- Samples taken from people and animals with suspected MP virus infection should be handled by trained staff working in suitably equipped laboratories.
- Polymerase chain reaction (PCR) is the preferred laboratory test given its accuracy and sensitivity; both qualitative and quantitative.
- How to collect the sample: for this, optimal diagnostic samples for MP are from skin lesions, the roof or fluid from vesicles and pustules, and dry crusts.
- Where feasible, biopsy is an option. The biopsy samples must be stored in a dry, sterile tube (no viral transport media or formalin is used for fixation) and kept cold.
- Do not perform PCR on blood, fluids, saliva, semen tests because these are usually inconclusive due to short duration of viremia relative to the timing of specimen collection after symptoms begin and should not be routinely collected from patients.
- Patient specimens must be safely prepared for transport with triple packaging in accordance with WHO guidance for transport of infectious substances.
- As orthopoxviruses are serologically cross-reactive, antigen and antibody detection methods do not provide MP-specific confirmation.
- Serology and antigen detection methods are therefore not recommended for diagnosis or case investigation where resources are limited.
- False positive test: recent or remote vaccination with a vaccinia-based vaccine (e.g., anyone vaccinated before smallpox eradication, or more recently vaccinated due to higher risk such as Orthopoxvirus laboratory personnel) might lead to false positive results.
- It is critical that patient information be provided with the specimens including: date of onset of fever, date of onset of rash, date of specimen collection, current status of the individual (stage of rash) etc.
Prevention of the MP virus
The prevention can be made through use of its vaccination, general public awareness, and safe practices through regulations. One vaccine, JYNNEOSTM (also known as Imvamune or Imvanex) contains a live attenuated vaccinia virus1,3,4. The smallpox was demonstrated through several observational studies to be about 85% effective in preventing MP. Thus, prior smallpox vaccination may result in milder illness. Evidence of prior vaccination against smallpox can usually be found as a scar on the upper arm. It can be used for children up to 18 years old and at high risk of the disease. Reportedly, this vaccine is 85% effective in preventing MP. There are two doses with 4-week duration; immunity after completion of schedule. It can be administered prophylactically and to the exposed persons. Experts also believe that vaccination after a MP exposure may help prevent the disease or make it less severe.
Raising public awareness
1. The media (electronic and social media), as a first line modality, should highlight the risk factors for this disease by eeducating people about the measures they can take to reduce exposure to the virus.
2. Use of mask, washing of the hands, and keeping the social distance are the main tools for protecting the transmission and breaking the chain of any infectious disease and MP virus. During this outbreaks, close contact with infected persons is the most significant risk factor for MP virus infection.
3. Health care authorities’ policies to train laboratory staff regarding the collection and safety of the sampling techniques, offering the vaccine to persons who may be at risk such as laboratory personnel, rapid response teams and health task force may be established in countries where cases are rising speedily. Health workers and their household members are at a greater risk of infection. Health workers caring for patients with suspected or confirmed MP virus infection, or handling specimens from them, should implement standard infection control precautions. If possible, persons previously vaccinated against smallpox should be selected to care for the patient.
4. The development of accurate surveillance system and rapid identification of new cases is critical for outbreak containment. The Government of Pakistan should keep the eyes by making an authority like The National Command and Operation Center, Pakistan during COVID-19. Some countries have put in place regulations restricting import of rodents and non-human primates especially from high risk countries.
5. Captive animals that are potentially infected with MP should be isolated from other animals and placed into immediate quarantine for 30 days. Unprotected contact with wild animals, especially those that are sick or dead, including their meat, blood, and other parts must be avoided. Additionally, all foods containing animal meat or parts must be thoroughly cooked before eating.
Treatment of the MP viral disease
- Clinical care for MP disease should be fully optimized to alleviate symptoms, manage complications and prevent long-term sequelae1,4.
- Patients should be offered liberal fluids and food to maintain adequate nutritional status.
- Secondary bacterial infections should be prevented and treated as indicated.
- An antiviral agent known as tecovirimat that was developed for smallpox was licensed by the European Medical Association for MP in 2022 based on the data in animal and human studies. If used for patient care, tecovirimat should ideally be monitored in a clinical research context with prospective data collection.
- The Cidofovir and Brincidofovir (CMX001) have proven activity against poxviruses in in vitro and animal studies but in humans the data is still not available.Brincidofovir may have an improved safety profile over Cidofovir. Data are not available on the effectiveness about vaccinia immune globulin (VIG). VIG can be considered for prophylactic use in an exposed person with severe immunodeficiency in T-cell function for which smallpox vaccination following exposure to MP is contraindicated.
List of Abbreviations
| MP | Monkey pox |
| PCR | Polymerase chain reaction |
| VIG | Vaccinia immune globulin |
| WHO | World Health Organization |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethical approval
Not required.
Author’s contribution:
Conception of the idea, acquisition of data, drafting of manuscript and approval of the final version of the manuscript to be published.
Authors’ Details
Mulazim Hussain Bukhari
- Professor of Pathology & Principal, Azad Jammu Kashmir Medical College, Muzaffarabad, Pakistan
References
- Ligon BL. Monkeypox: a review of the history and emergence in the Western hemisphere. Semin Pediatr Infect Dis. 2004;15(4):280–7. https://doi.org/10.1053/j.spid.2004.09.001
- Dawn: Govt declares high alert against monkeypox; 2022 [cited 2022 Jun 6]. Available from: https://www.dawn.com/news/1692258
- World Health Organization. Monkeypox: key facts. Geneva, Switzerland: World Health Organization [cited 2022 Jun 6]. Available from: https://www.who.int/news-room/fact-sheets/detail/monkeypox
- Centre for Disease Control and Prevention. Monkeypox. Centre for Disease Control and Prevention [cited 2022 Jun 5]. Available from: https://www.cdc.gov/poxvirus/monkeypox/index.html
- ScienceInsider. Monkeypox outbreak questions intensify as cases soar. ScienceInsider [cited 2022 Jun 5]. Available from: https://www.science.org/content/article/monkeypox-
outbreak-questions-intensify-cases-soar
Keywords: Monkeypox, Orthopoxvirus, Pakistan, Small Pox, Vaccine
Publication History
Received: May 25, 2022
Revised: June 07, 2022
Accepted: June 10, 2022
Published: June 20, 2022
Authors
Mulazim Hussain Bukhari
Professor of Pathology, Principal, Azad Jammu Kashmir Medical College, Muzaffarabad, Pakistan.
