Case Report
Volume: 39 | Issue: 4 | Published: Dec 25, 2023 | Pages: 145 - 149 | DOI: 10.24911/BioMedica/5-1144
Fibroadenoma of the Breast Occurring Synchronously in Twin Sisters- A Case Report
Authors: Firdous Iqbal , Gul-e-Rana
Article Info
Authors
Firdous Iqbal
Assistant Professor, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Lahore, Pakistan.
Gul-e-Rana
Postgraduate Trainee, Department of Histopathology, Al-Aleem Medical College/Gulab Devi Hospital, Lahore, Pakistan.
Publication History
Received: November 10, 2023
Accepted: December 15, 2023
Published: December 25, 2023
Abstract
Fibroadenomas (FAs) are the most common benign tumors of the breast in young females. Most of the time, it presents as a well-circumscribed, painless, firm to hard, mobile, and slow-growing unilateral or bilateral breast lump. The median age of its presentation is 25 years with rare occurrence after menopause. The exact etiology of FA is still unclear. Unopposed estrogen in the growing breasts of young females is considered as a main factor in its pathogenesis. Family history and development of FA in identical twins are suggestive of genetic contribution to the pathogenesis of these tumors.
This is a case report of young twin sisters who presented at a tertiary care hospital in Lahore with a complaint of a synchronously developed unilateral breast lump. Fine needle aspiration cytology was planned after taking a detailed history and clinical examination of both patients. Diagnosis of FA was confirmed radiologically and through cytological examination. To the best of the authors’ knowledge, this is the first case of its kind reported from Pakistan.
Keywords: Fibroadenoma, breast lump, cytology, twin sisters
Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 39(4):145-149
CASE REPORT
Fibroadenoma of the breast occurring synchronously in twin sisters- a case report
Firdous Iqbal1*, Gul- e- Rana2
Received: 10 November 2023 Revised date: 03 December 2023 Accepted: 15 December 2023
Correspondence to: Firdous Iqbal
*Assistant Professor, Department of Morbid Anatomy and Histopathology, University of Health Sciences Lahore, Lahore, Pakistan.
Email: dr.firdousiqbal21@gmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Fibroadenomas (FAs) are the most common benign tumors of the breast in young females. Most of the time, it presents as a well-circumscribed, painless, firm to hard, mobile, and slow-growing unilateral or bilateral breast lump. The median age of its presentation is 25 years with rare occurrence after menopause. The exact etiology of FA is still unclear. Unopposed estrogen in the growing breasts of young females is considered as a main factor in its pathogenesis. Family history and development of FA in identical twins are suggestive of genetic contribution to the pathogenesis of these tumors.
This is a case report of young twin sisters who presented at a tertiary care hospital in Lahore with a complaint of a synchronously developed unilateral breast lump. Fine needle aspiration cytology was planned after taking a detailed history and clinical examination of both patients. Diagnosis of FA was confirmed radiologically and through cytological examination. To the best of the authors’ knowledge, this is the first case of its kind reported from Pakistan.
Keywords:
Fibroadenoma, breast lump, cytology, twin sisters.
Introduction
The term fibroadenoma (FA) is a combination of the words fibro means fibrous or stromal tissue and adenoma which means arrangement of epithelial components of a tumor in a benign glandular architecture. It is the most common benign tumor of the breast in adolescent and young females encompassing 91% of all solid breast masses in adolescent girls1. It often presents as a painless, unilateral, solid, mobile, and slow-growing breast lump. with the size of the lesion usually remaining less than 3 cm but it may grow even larger. With increasing age, FAs tend to decrease in size and cellularity.2
Histologically, FA presents as a circumscribed, un-encapsulated, and noninfiltrative breast lump. It is a benign biphasic (fibroepithelial) tumor showing proliferation of both stromal and epithelial components of the terminal duct lobular unit (TDLU) of the breast. Stroma is intralobular, enclosing glandular spaces lined by inner epithelial and outer myoepithelial cell layers.3 Cytological features of FA are fibromyxoid stroma (92.7% of cases), staghorn clusters of epithelial cells (73.6% of cases), and numerous bare nuclei in the background representing myoepithelial cells (73.6% of cases).4
Among different variants of FA, cellular FAs show increased stromal cellularity. Juvenile FAs show increased stromal cellularity along with a higher degree of epithelial hyperplasia, commonly occurring in young girls and adolescents. Complex FAs reveal cysts greater than 3 mm in size, sclerosing adenosis, epithelial calcifications, or papillary apocrine metaplasia.5 All histological variants of FAs, behave in a benign fashion with minimal or no malignant potential. The risk of malignant transformation is extremely low and has been reported to range around 0.01%-0.3%.6 The published literature regarding the occurrence of FAs synchronously in twin young sisters, without any significant family history, is hard to find. To the best of the authors’ knowledge, this is the first case report of its kind from Pakistan.
Case Presentation
We report a case of 21-year-old unmarried twin sisters belonging to a remote rural area of Punjab who presented to a tertiary care hospital in Lahore, Pakistan, with a 2-year history of unilateral breast lump. One patient noticed it in her right breast while the other one spotted it in her left breast. Self-examination revealed a painless lump gradually increasing in size. One noted this lump 2 weeks later than the other. There was no history of breast trauma, associated breast pain, or discharge from the nipple. No history of smoking, previous breast surgery, or other breast disease was there. A family history of breast cancer or FA was negative. No hormonal oral contraceptives were used by both patients. Past medical history was insignificant. The age of menarche was 13 years in both patients and both had regular menstrual cycles of 28 days. On clinical examination, one patient had a single 3.0 × 2.0 cm lump in the right upper outer quadrant and the other patient had a 4.0 × 3.0 cm lump in the left central quadrant of her breast. Both lumps were firm, mobile, and not attached to overlying skin or underlying structures. Breast imaging-reporting and data system (BI-RADS) category two was diagnosed on ultrasound.
After explaining the procedure of FNAC, written informed consent was taken from both girls. FNAC of breast lump was performed in both using a 23-gauge needle under aseptic conditions. A total of 4 smears were prepared from each patient and stained with Hematoxylin and Eosin (H&E) stain.
Cytologically, aspirates from both patients were moderately cellular and revealed characteristic monolayer sheets of benign-looking epithelial cells (designated as “staghorn,” with antler-like configuration on edges) mixed with myoepithelial cells (shown as numerous naked/bipolar nuclei in the background of the aspirate). Cellular cohesiveness was also appreciated. Accompanying the epithelial cells, a small fragment of stromal material was also seen in the aspirate of both patients (Figures 2 and 3).
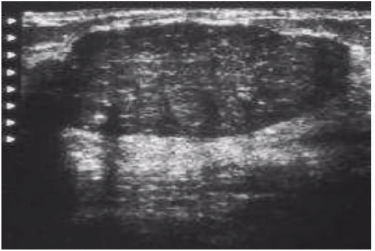
Figure 1. A hypoechoic, single 3.0 × 2.0 cm lump in the right upper outer quadrant of the breast in patient-1 consistent with BI-RADS-2.
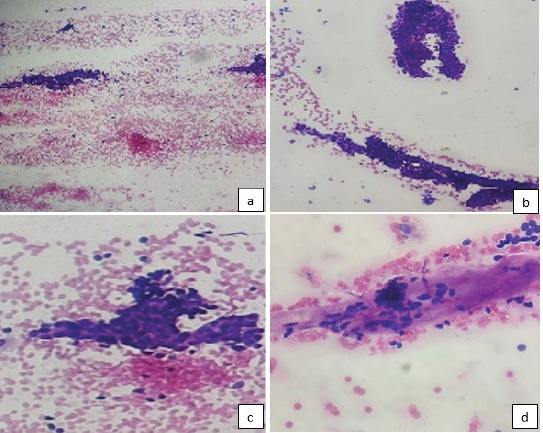
Figure 2. Cytological features of FA from patient-1: Mono-layered sheets of benign epithelial cells with bare nuclei in the background. (a-c) and stromal component(d) (H&E: a = 100X, b = 200X, c,d = 400X).
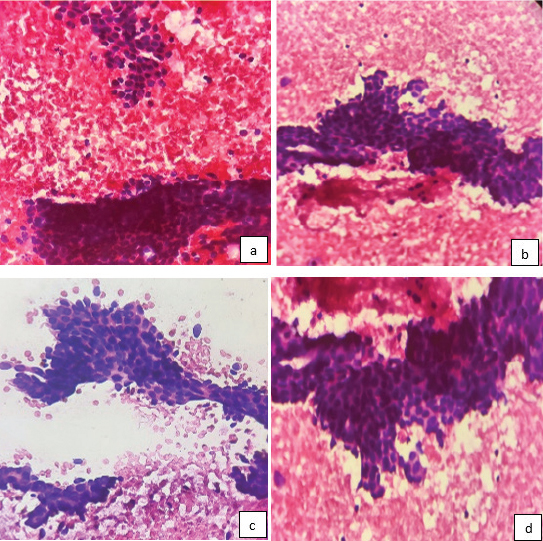
Figure 3. Cytological features of FA from patient-2. Branching sheets of benign epithelial and myoepithelial cells(a-d). (H&E: 400X).
Cytological diagnosis of FA was made in both patients. No follow up regarding the management of the lesion was made in both patients as they were counseled and advised monitoring of the size of the lesion through a yearly mammogram or breast ultrasound.
Discussion
FA occurring synchronously in two twin young sisters is the first case reported of its kind from Pakistan. FAs is a benign breast neoplasm mostly seen in young females between the age of 15-34 years. Usually, it appears as a single, lump however, multifocal and bilateral lesions have also been reported8. This lesion is also called a breast mouse due to its mobile nature. The median age of its presentation is 25 years but can occur at any age. However, it is rare in postmenopausal females. The cellularity of the tumor decreases with age. Regression due to infarction with calcification and hyalinization may occur. Multiple myxoid FAs in both breasts can be seen in patients suffering from Carney complex. Multiple and bilateral involvement is also observed in patients who have a family history of such lesions.7,8
Pathogenesis of FA is still not clear. The reproductive hormone estrogen in the growing breasts of young females is the most important etiological factor in its development9. In previous studies, exposure to hormones (endogenous and exogenous) is well documented in the development of FA.10 Therefore, it is observed that FAs may grow in size during pregnancy and usually involute after menopause. However, the use of combined oral contraceptive pills is reported to decrease the risk of FA by altering the sensitivity of the breast to endogenous hormones and by decreasing the production of hormones from ovaries.11 At present, the genetic abnormalities that underlie these neoplasms remain incompletely understood. MED12 mutations, located in codon 44 of exon 2 are identified in up to 65% of adult FAs.12 The concurrent occurrence of FA in identical twins is also indicative of genetic contribution to the etiology of these tumors; however, this is not fully proven.
According to a similar case presented by Badawi et al.13 identical twin sisters of 19 years, presented with breast lumps of almost the same size in the same breast and size remained constant. On the contrary, in the current case age of presentation was 21 years, both patients presented with breast lumps of different sizes in different breasts, and the lump was gradually increasing in size. In the case reported by Badawi et al.13 patients had a history of 2 weeks, were diagnosed sonographically with no cytological or histological correlation, and were managed conservatively, whereas, in the present study, the patients had a history of 2 years, and were diagnosed cytologically with a conservative management plan by the surgeon. The morphology of both breast lesions was in concordance with the routine cytological features of FAs.
Rarely, atypical ductal hyperplasia, atypical lobular hyperplasia, ductal carcinoma in situ, lobular carcinoma in situ, and invasive carcinomas can evolve from an FA. These patients are treated according to their high-risk, pre-cancer, or cancerous lesions.14 Retrospective studies established the relative risk of breast carcinoma as 2.17 and 3.1 times higher in women with FAs and complex FAs, respectively, as compared with the general population of the same age group .15
History and clinical evaluation can discriminate FAs and other causes of breast lumps. Ultrasound is the favored method of evaluation with cytomorphological confirmation of the lesion. It is mostly categorized as BI-RADS 2 or 3. FNAC can improve the sensitivity of the diagnosis of FA to 86% with a specificity of 76%.16
There is no known medical treatment for FA. Conservative management with follow up is the usual practice to manage these patients. Surgical excision is done in cases where the mass is increasing in size, if the patient is symptomatic and the lesion becomes painful or if there is any confusion in the diagnosis of FA.17
Conclusion
FA is a biphasic benign breast tumor of young females. In the current case report, cytomorphological confirmation of diagnosis was done in two young twin sisters. It was managed conservatively. Though the occurrence of FAs synchronously in twin sisters is indicative of genetic contribution to its etiology, the family history in the present case revealed no significant findings.
Limitations of the Study
This study could not include genetic analysis as FAs in these particular cases were not linked to any strong predisposing genetic factors.
List of Abbreviations
| FA | Fibroadenoma |
| FNAC | Fine needle aspiration cytology |
| H&E | Hematoxylin and Eosin |
Conflict of interest
None to declare.
Ethical approval
The authors were exempted from ethical approval from the Institutional Ethical Review Board of Al-Aleem Medical College Lahore, Pakistan, as this case report is published primarily for educational purposes rather than research, and the data were collected as part of routine care. Permission was granted by the concerned Head of the Department for publication and the Editorial Board verified all the original clinical records including the consent from the patients.
Authors’ contributions
FI: Conception and drafting of the manuscript, critical intellectual input, and revisions.
FI. GR: Acquisition and interpretation of data
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ Details
Firdous Iqbal1, Gul e Rana2
- Assistant Professor, Department of Histopathology, University of Health Sciences, Lahore, Pakistan
- Postgraduate trainee, Department of Histopathology, Al-Aleem Medical College/Gulab Devi Hospital, Lahore, Pakistan
References
- Sanchez R, Ladino-Torres MF, Bernat JA, Joe A, DiPietro MA. Breast fibroadenomas in the pediatric population: common and uncommon sonographic findings. Pediatr Radiol. 2010;40(10):1681–9. https://doi.org/10.1007/s00247-010-1678-7 PMID:20449731
- Greenberg R, Skornick Y, Kaplan O. Management of breast fibroadenomas. J Gen Intern Med. 1998 Sep;13(9):640–5. https://doi.org/10.1046/j.1525-1497 1998.cr188. x.
- Krishnamurthy S, Ashfaq R, Shin HJ, Sneige N. Distinction of phyllodes tumor from fibroadenoma: a reappraisal of an old problem. Cancer. 2000;90(6):342–9. PMID: 11156517.
- Kollur SM, El Hag IA. FNA of breast fibroadenoma: observer variability and review of cytomorphology with cytohistological correlation cytopathology. 2006;17(5):239–44. https://doi.org/10.1111/j.1365-2303.2006.00360.x PMID:16961651
- Krings G, Bean GR, Chen YY. Fibroepithelial lesions; The WHO spectrum. Semin Diagn Pathol. 2017;34(5):438–52. https://doi.org/10.1053/j.semdp.2017.05.006 PMID:28688536
- Jones J, Bell D, Niknejad M Fibroadenoma (breast). Reference article, Radiopaedia.org [Cited 2023 Dec 02]. https://doi.org/10.53347/rID-9021
- Neville G, Neill CO, Murphy R, Corrigan M, Redmond PH, Feeley L, et al. Is excision biopsy of fibroadenomas based solely on size criteria warranted? Breast J. 2018;24(6):981–5. https://doi.org/10.1111/tbj.13069 PMID:29802656
- Williamson ME, Lyons K, Hughes LE. Multiple fibroadenomas of the breast: a problem of uncertain incidence and management. Ann R Coll Surg Engl. 1993;75(3):161–3. PMID:8323208
- Song BS, Kim EK, Seol H, Seo JH, Lee JA, Kim DH, et al. Giant juvenile fibroadenoma of the breast: a case report and brief literature review. Ann Pediatr Endocrinol Metab. 2014;19(1):45–8. https://doi.org/10.6065/apem.2014.19.1.45 PMID:24926464
- Musio F, Mozingo D, Otchy DP. Multiple, giant fibroadenomas. Am Surg. 1991;57(7):438–41. PMID:1647714
- Dent DM, Hacking EA, Wilkie W. Benign breast disease clinical classification and disease distribution. Br J Clin Pract. 1988;42(suppl 56):69–71.
- Lien HC, Huang CS, Yang YW, Jeng YM. Mutational analysis of MED12 exon 2 in a spectrum of fibroepithelial tumours of the breast: implications for pathogenesis and histogenesis. Histopathology. 2016;68(3):433–41. https://doi.org/10.1111/his.12764 PMID:26109290
- Badawi M, Shalaby A. Fibroadenoma of the breast in identical twin: a case report. Clin Case Rep. 2021;11(3):1–3
- Feliciano YZ, Freire R, Net J, Yepes M. Ductal and lobular carcinoma in situ arising within an enlarging biopsy proven fibroadenoma. BMJ Case Rep. 2021;14(1):e237017. https://doi.org/10.1136/bcr-2020-237017 PMID:33468635
- Dupont WD, Page DL, Park FF. Long-term risk for breast cancer in women with fibroadenoma. N Engl J Med. 1994;331:10–15. https://doi.org/10.1056/NEJM199407073310103.
- Dent DM, Cant PJ. Fibroadenoma. World J Surg. 1989;13(6):706–10. https://doi.org/10.1007/BF01658418. PMID: 2696223.
- Javed A, Jenkins SM, Labow B, Boughey JC, Lemaine V, Neal L, et al. Intermediate and long-term outcomes of Fibroadenoma excision in adolescent and young adult patients. Breast J. 2019;25:91–5. https://doi.org/10.1111/tbj.13159
