Biomedica - Official Journal of University of Health Sciences, Lahore, Pakistan
Volume 40(2):95-99
ORIGINAL ARTICLE
Diagnostic accuracy of intraoperative touch imprint cytology and frozen sections for the evaluation of margin status and diagnosis of oro-pharyngeal squamous cell carcinomas
Hamna Salahuddin1,2*, Sadia Sharif3, Shizra Kaleemi4, Kanwal Babar5, Abeer Zaheer6, Sadia Anwar7
Received: 01 April 2024 Revised date: 07 June 2024 Accepted: 20 June 2024
Correspondence to: Hamna Salahuddin
*Former Assistant Professor, Department of Pathology, University College of Medicine and Dentistry, University of Lahore, Lahore, Pakistan.
Email: Dr_device_hamna@hotmail.com
Full list of author information is available at the end of the article.
ABSTRACT
Background and Objective:
In surgical procedures, accurate intraoperative diagnosis is essential for guiding surgical management. Two common techniques employed for rapid intraoperative diagnosis are touch imprint cytology (TIC) and frozen section (FS). However, their diagnostic accuracy as compared to histopathology remains under debate. This study therefore aims to evaluate the diagnostic precision of FSs and TIC taking histopathology as a gold standard in oropharyngeal squamous cell carcinoma (OPSCC) biopsies.
Methods:
A total of 122 biopsies of OPSCC were received for FS analysis at the Histopathology Department of the University College of Medicine and Dentistry Lahore, Pakistan. Touch imprints were taken from the surgical margins of the same biopsies and FSs were cut and stained with rapid Hematoxylin and Eosin stain following standard protocols. Paraffin-embedded histopathology sections were later made from the same tissues for comparison and diagnostic accuracy studies.
Results:
Comparison of FS with histopathology showed a sensitivity of 60%, specificity of 100%, positive predictive value (PPV) of 100%, negative predictive value (NPV) of 95%, and overall diagnostic accuracy of 95%. On comparison of TIC with histopathology, sensitivity was 86.6%, specificity was 100%, PPV was 100%, NPV was 98.2%, and accuracy was 98.3%.
Conclusion:
In comparison to histopathology, TIC and FS examination have promising utility as well as certain limitations for the evaluation of the margin status of OPSCC specimens. Thus, with careful consideration, these techniques may provide valuable insights for clinical practice in local settings with both time and cost-effective approaches.
Keywords:
Frozen section, histopathology, touch imprint, diagnostic accuracy, specimens, surgical margins, oropharyngeal squamous cell carcinoma.
Introduction
Surgeons require intraoperative consultation from pathologists for prompt decision-making and performing gilt-edge surgical procedures. Both Frozen Section (FS) and touch impression cytology (TIC) serve this purpose well.1,2 The rapid FS method is a means of intraoperative pathological diagnosis, first introduced by Welchin in 1891 and developed as a diagnostic tool by Wilson in 1905.3
FS is helpful in the evaluation of margin status, diagnosis of metastatic carcinoma in sentinel lymph nodes (SLNs).4 SLN biopsy is performed in surgical oncology in daily practice. It can be performed by cytological examination (scrape, smear, or touch), histologic FS, immunohistochemical stains, and/or molecular biology. Of these, the most important and widely utilized methods are FS, TIC, and a combination of both.5
The limitations of FS include cutting artifacts, poor quality of sections, suboptimal histology, poor quality staining, pressure of immediate diagnosis, and lack of ancillary studies at the time of intraoperative consultation. The FS method can provide information about the depth of infiltration but is limited by its cost and the need for qualified technical staff. Therefore, FSs should not be considered as replacement of the permanent sections.6
TIC is prepared from fresh surgical specimens and provides valuable information when FS interpretation is equivocal.5 Lack of alteration of tissue morphology in TIC helps in making the evaluation of tissue on subsequent permanent section better. However, there is still some reluctance on part of some pathologists most likely due to their inadequate experience to render a definite diagnosis on TIC alone.7,8
The current study will evaluate the diagnostic accuracy of intraoperative TIC and FS analyses in comparison with histopathology for oropharyngeal squamous cell carcinoma (OPSCC) biopsies. The data from the current study will help us assess the practical utility of FS and TIC in a tertiary care setting for these tissues where resources are limited.
Methods
This comparative, cross sectional study comprised of a total of 122 specimens of FSs from oropharyngeal squamous cell carcinoma patients received during a period of 6 months (1st December 2021 till 1st June 2022) at the Histopathology department of University College of Medicine and Dentistry, Lahore, Pakistan. Those cases in which samples were sent in formalin or were improperly labelled were excluded from the study. The specimens were grossed according to the standard protocols for margin resection. Touch imprints covering both the surfaces of the surgical margin were taken and FSs were cut from the same using standard method. Both these slides were stained by rapid Hematoxylin and Eosin (H&E) stain. Later, the same margins were sent to histopathology section of the Department of Pathology for obtaining permanent histopathology sections. At least three to four pathologists reviewed each case and decisions were made with a consensus of the majority. External opinions were also taken in case of disagreements.
Statistical Analysis
For statistical analysis, FS, TIC and Histopathology methods were analyzed, interpreted, and recorded in tabular manner along with suitable graphical representations. The FS and TIC results were compared to final histopathological diagnoses and categorized into two groups: concordant and discordant. The examinations were considered concordant when the permanent and FS diagnosis was the same and discordant if there was mismatch between FS and permanent section diagnosis. Finally, discordant cases were analyzed and causes of disagreement were recorded.
Diagnostic accuracy was assessed by calculating sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Sensitivity was defined as the proportion of true positive cases correctly identified by the diagnostic test, while specificity was the proportion of true negative cases accurately detected. PPV was calculated as the percentage of positive test results that were true positives, and NPV as the percentage of negative test results that were true negatives. The analysis was performed using a 2 × 2 contingency table, and 95% confidence intervals were calculated for each metric to assess the precision of the estimates. Statistical significance was set at a p-value < 0.05. All computations were conducted using Stata version 18.
Results
Total 122 FS biopsies were received from maxillofacial Department for margin status analysis of oropharyngeal squamous cell carcinoma (OPSSC). Out of 122 OPSCC, the number of FS received from mandible, tongue and buccal mucosa were 45 (37%), 52 (43%) and 25 (20%) respectively. All of the cases were referred for permanent sections for histopathology.
The results of FS were concordant with histopathology in 116 (95%) cases and discordant in 6 (5%) cases in case of OPSCC. Among the concordant cases, 9 (7.37) cases /margins were true positive for malignancy and 107 (87.7%) cases/margins were true negative for malignancy (Table 1).
Figure 1 shows positive margin on FS while Figure 2 shows negative margin on FSs. Among the discordant cases, the surgical margins were reported negative on FS while these were reported positive on subsequent permanent sections (false negative).
The diagnosis of TIC was concordant with permanent section diagnosis of negative margin in 107 (98.3%) cases and positive margin in 13 (10.6%) cases. It was discordant in 2 (1.7%) cases. (Table.1) Among the discordant cases, only 2 (4%) surgical margins were reported negative on TIC while these turned out to be positive on permanent sections.
Table 1. Status of concordance among FS and TICwith respect to the site of the tumor.
| Site | Total | FS | TIC | |||
|---|---|---|---|---|---|---|
| Concordant | Discordant | Concordant | Discordant | |||
| Mandible | 45 | 43 (96%) | 2 (4%) | 45 (100%) | 0 | |
| Tongue | 52 | 49 (94.2%) | 3 (5.7%) | 50 (96%) | 2 (4%) | |
| Buccal mucosa | 25 | 24 (96%) | 1 (4%) | 25 (100%) | 0 | |
| Total | 122 | 116 (95%) | 6 (5%) | 120 (96%) | 2 (4%) | |
On comparison of FS with histopathology the, the sensitivity, specificity, PPV, NPV and accuracy of FS is 60%,100%,100%, 95% and 95% respectively. (Figure 3)
On comparison of TIC with histopathology the sensitivity, specificity, PPV, NPV and accuracy of TIC is 86.6%, 100%, 100%, 98.2% and 98.3% respectively (Figure 3).
Discussion
In the therapeutic management of diverse malignant disorders, FS analysis stands as a precise intraoperative diagnostic modality. It serves as a pivotal tool in determining the requisite extent of surgical intervention, thereby guiding subsequent therapeutic strategies. The decision regarding the nature of surgical intervention or ensuing treatment modalities hinges upon various factors, notably the discernment of neoplastic presence or absence. Furthermore, the determination of margin status in malignant lesions holds paramount significance, as the attainment of adequate margins is pivotal in preventing tumor recurrence. This axiom particularly resonates in the realm of head and neck malignancies, where the meticulous assessment of resected specimen margins assumes heightened importance, given the anatomical constraints and the imperative for maximal tumor excision within limited spatial confines 9,10 A positive margin of 5 mm is associated with a higher probability of local recurrence in most of the tumors including OPSS.10,11 To reduce the recurrence rate, adequate margin clearance is essential in head and neck tumors, and intraoperative FS is widely used by surgeons to achieve clear margins.12-14
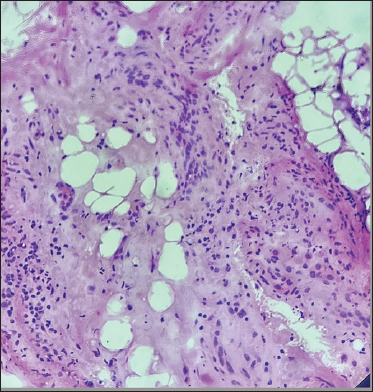
Figure 1. The H&E stained sections show nests of large polygonal cells (arrow head) infiltrating the soft adipose tissue margin.
In this study we attempted to assess the differences in the diagnosis made on TIC, FS, and subsequent histopathological sections. The reason for discordance may be attributed to the lack of proper cutting of FS block and presence of tumor in subsequent deeper levels of permanent sections.
The high specificity (100%) and PPV of FS (100%) indicates its reliability in confirming the presence of malignancy. This is particularly evident in the cases where FS accurately identified positive margins for malignancy. However, the sensitivity of FS (60%) raises concerns regarding its ability to detect malignancy, especially in cases where false negatives occurred due to inadequate cutting of FS blocks or deeper tumor involvement missed during initial assessment.
However, it is important to note that in the broader body of literature, the sensitivity of FS analysis typically falls within the ranges of 87%–97%.15,16 which is concordant with our results. In our investigation, the sensitivity of FS analysis was determined to be 60%, a figure notably lower when compared to the study by Bharadwaj et al. 5 where a sensitivity of 92.5% was reported.
Notably, renowned institutions such as the Mayo Clinic in Rochester, USA, have reported a remarkable overall accuracy of 97.8% after reviewing a significant volume of frozen cases.17 Click or tap here to enter text. Consistently, within the literature, diagnostic accuracy rates for FSs have been documented to range from 87% to 97% 18 In our investigation, we observed a diagnostic accuracy rate of 95%, aligning favorably with the aforementioned studies.
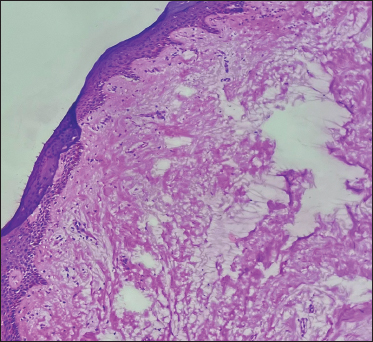
Figure 2. The H&E stained section shows squamous mucosa uninvolved by tumor on FS.
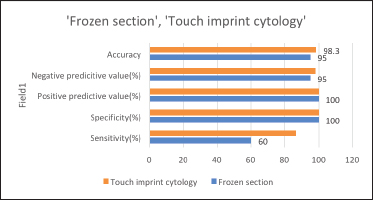
Figure 3. The values of diagnostic accuracy studies for FS and TIC as compared to histopathology (gold standard).
The discordant cases in our studies were 6 (5%) and the most common causes of discordant diagnosis in the present study are sampling error. Similar results were seen in study conducted by Tangde et al and Novis et al.19,20
The occurrence of false negatives in both FS and TIC underscores the challenges associated with intraoperative diagnosis, including sampling errors and difficulties in interpreting tissue specimens rapidly. Moreover, the limited sensitivity of FS raises concerns regarding its reliability in detecting malignancy, necessitating caution in its interpretation and reliance on subsequent histopathological evaluation for definitive diagnosis.
Conclusion
In conclusion, the data presented underscores the significance of FS and TIC as valuable adjuncts to histopathology in intraoperative diagnosis of oropharyngeal squamous cell carcinoma. While both techniques offer rapid assessment and aid in guiding surgical management, careful consideration of their limitations and diagnostic accuracy is essential for ensuring optimal patient care and treatment outcomes.
Limitations of the Study
This study has several limitations that must be acknowledged. Firstly, the sample size is relatively small, consisting of only a limited number of squamous cell carcinoma (SCC) cases. This small sample size reduces the generalizability of our findings. Secondly, the data was collected from a single institution, which may introduce institutional biases and limit the applicability of the results to other settings or populations. Moreover, this study did not account for various pathological variables or clinical details that could significantly influence the outcomes. Future research should aim to include larger, multi-center cohorts and incorporate comprehensive pathological and clinical data to validate and extend the findings of this study.
Acknowledgement
The authors would like to acknowledge the patients who participated in this study, as well as the Maxillofacial and Pathology Departments of UCMD Lahore, Pakistan involved in sample collection, processing, and analysis.
List of Abbreviations
| FS | Frozen section |
| H&E | Hematoxylin and eosin. |
| PPV | Positive predictive value |
| SLN | Sentinel lymph node |
| TIC | Touch imprint cytology |
Conflict of interest
None to declare.
Grant support and financial disclosure
None to disclose.
Ethics approval
The study was approved by the Institutional Ethical Review Committee of UCMD Lahore, Pakistan vide Letter No: ERC/96/22/02 dated 7/02/2022.
Authors’ contributions
HS, KB: Principal investigator, concept and design of study, critical intellectual input
HS, SS, SK: Drafting of the manuscript, acquisition of data.
AZ: Analysis of data and interpretation.
ALL AUTHORS: Approval of the final version of the manuscript to be published.
Authors’ details
Hamna Salahuddin1,2, Sadia Sharif3, Shizra Kaleemi4, Kanwal Babar5, Abeer Zaheer6, Sadia Anwar7
- Former Assistant Professor, Department of Pathology, University College of Medicine and Dentistry, University of Lahore, Lahore, Pakistan
- Assistant Professor, Ameeruddin Medical College, Lahore, Pakistan
- Associate Professor, Department of Pathology, University College of Medicine and Dentistry, University of Lahore, Lahore, Pakistan
- Assistant Professor, Department of Pathology, Al Aleem Medical College/Gulab Devi Hospital, Lahore, Pakistan
- Consultant Pathologist, Chughtai Lab, Lahore, Pakistan
- Assistant Professor, Department of Pathology, Rahbar Medical & Dental College, Lahore, Pakistan
- Associate Professor, Department of Pathology, Ameeruddin Medical College Lahore, Pakistan
References
- Kang M, Chung DH, Kim NR, Cho HY, Ha SY, Lee S et al. Intraoperative frozen cytology of central nervous system neoplasms: an ancillary tool for frozen diagnosis. J Pathol Transl Med. 2019;53(2):104–11. https://doi.org/10.4132/jptm.2018.11.10
- Namdar ZM, Omidifar N, Arasteh P, Akrami M, Tahmasebi S, Nobandegani AS et al. How accurate is frozen section pathology compared to permanent pathology in detecting involved margins and lymph nodes in breast cancer? World J Surg Oncol. 2021 1;19(1):261. https://doi.org/10.1186/s12957-021-02365-5
- Vélez D, Ríos A, Vélez A, Bohórquez M. Diagnostic accuracy and discrepancy of frozen section analysis in a Colombian intermediate care center. Univ Med. 2021;62(3). https://doi.org/10.11144/Javeriana.umed62-3.froz
- Komenaka IK, Torabi R, Nair G, Jayaram L, Hsu CH, Bouton ME et al. Intraoperative touch imprint and frozen section analysis of sentinel lymph nodes after neoadjuvant chemotherapy for breast cancer. Ann Surg. 2010;251(2):319–22. https://doi.org/10.1097/SLA.0b013e3181ba845c
- Bharadwaj B, Deka M, Salvi M, Das BK, Goswami BC. Frozen section versus permanent section in cancer diagnosis: a single centre study. AJCC. 2022;7(2):247–51. https://doi.org/10.31557/apjcc.2022.7.2.247-251
- Mohamed A, Hassan MM, Zhong W, Kousar A, Takeda K, Donthi D et al. A quantitative and qualitative assessment of frozen section diagnosis accuracy and deferral rate across organ systems. Am J Clin Pathol. 2022;158(6):692–701. https://doi.org/10.1093/ajcp/aqac115
- Wang J, Zhao Y, Chen Q, Zhang P, Xie W, Feng J et al. Diagnostic value of rapid on-site evaluation during transbronchial biopsy for peripheral lung cancer. Jpn J Clin Oncol. 2019;49(6):501–5. https://doi.org/10.1093/jjco/hyz025
- Oki M, Saka H, Kitagawa C, Kogure Y, Murata N, Adachi T et al. Rapid on-site cytologic evaluation during endobronchial ultrasound-guided transbronchial needle aspiration for diagnosing lung cancer: a randomized study. Respiration. 2013;85(6):486–92. https://doi.org/10.1159/000346987
- Wang KG, Chen TC, Wang TY, Yang YC, Su TH. Accuracy of frozen section diagnosis in gynecology. Gynecol Oncol. 1998;70(1):105–10. https://doi.org/10.1006/gyno.1998.5057
- Adhikari P, Upadhyaya P, Karki S, Agrawal CS, Chettri ST, Agrawal A. Accuracy of frozen section with histopathological report in an institute. J Nepal Med Assoc. 2018;56(210):572–7.
- Asoda S, Miyashita H, Soma T, Munakata K, Yamada Y, Yasui Y, et al. Clinical value of entire-circumferential intraoperative frozen section analysis for the complete resection of superficial squamous cell carcinoma of the tongue. Oral Oncology. 2021;123:105629. https://DOI.ORG/10.1016/j.oraloncology.2021.105629
- Varvares MA, Poti S, Kenyon B, Christopher K, Walker RJ. Surgical margins and primary site resection in achieving local control in oral cancer resections. Laryngoscope. 2015;125(10):2298–307. https://doi.org/10.1002/lary.25397
- Ali JP, Mallick BA, Rashid K, Malik UA, Hashmi AA, Zia S, et al. Diagnostic accuracy of intraoperative frozen section for margin evaluation of oral cavity squamous cell carcinoma. BMC Res Notes. 2024;17(1):43. https://doi.org/10.1186/s13104-024-06698-8
- Tamhane AN, Shukla S, Acharya S, Acharya N, Hiwale K, Bhake A. Intraoperative surgical margin clearance - correlation of touch imprint cytology, frozen section diagnosis, and histopathological diagnosis. Int J Appl Basic Med Res. 2020 ;10(1):12–6. https://doi.org/10.4103/ijabmr.IJABMR_325_18
- Olson SM, Hussaini M, Lewis JS Jr. Frozen section analysis of margins for head and neck tumor resections: reduction of sampling errors with a third histologic level. Mod Pathol. 2011;24(5):665–70. https://doi.org/10.1038/modpathol.2010.233
- Mahe E, Ara S, Bishara M, Kurian A, Tauqir S, Ursani N et al. Intraoperative pathology consultation: error, cause and impact. Can J Surg. 2013;56(3):E13–8. https://doi.org/10.1503/cjs.011112
- Ferreiro JA, Myers JL, Bostwick DG. Accuracy of frozen section diagnosis in surgical pathology: review of a 1-year experience with 24,880 cases at Mayo Clinic Rochester. Mayo Clin Proc. 1995;70(12):1137–41. https://doi.org/10.4065/70.12.1137
- Vahini G, Ramakrishna BA, Kaza S, Rama Murthy N. Intraoperative frozen section -a golden tool for diagnosis of surgical biopsies. Int Clin Pathol J. 2017;4(1):22–6. https://doi.org/10.15406/icpjl.2017.04.00084
- Tangde A, Shrivastava V, Joshi A. Analysis of frozen section in correlation with surgical pathology diagnosis. Int J Res Med Sci. 2019;7(6):2312–7. https://doi.org/10.18203/2320-6012.ijrms20192519
- Novis DA. Detecting and preventing the occurrence of errors in the practices of laboratory medicine and anatomic pathology: 15 years’ experience with the College of American Pathologists’ Q-PROBES and Q-TRACKS programs. Clin Lab Med. 2004;24(4):965–78. https://doi.org/10.1016/j.cll.2004.09.001
Keywords: Frozen section, histopathology, touch imprint, diagnostic accuracy, specimens, surgical margins, oropharyngeal squamous cell carcinoma.
Publication History
Received: April 01, 2024
Revised: June 07, 2024
Accepted: June 20, 2024
Published: June 25, 2024
Authors
Hamna Salahuddin
University College of Medicine and Dentistry, Ameer-ud-din Medical College
Sadia Sharif
University College of Medicine and Dentistry
Shizra Kaleemi
Al Aleem Medical College
Kanwal Babar
Chughtai Lab, Lahore, Pakistan
Abeer Zaheer
Rahbar Medical & Dental College
Sadia Anwar
Ameeruddin Medical College
